Groin pain is a common symptom because different tissues and organs intersect in this area, which can cause localized (local) soreness). The reason should be sought in the genitourinary or musculoskeletal system. A specific disease can be suspected by the nature of the pain, which can be weak, dull or strong, aching or sharp, constant or intermittent. Sometimes additional redness and swelling appear. It all depends on what caused the symptoms to appear. In this regard, we suggest studying the most possible causes of groin pain in men.
Inguinal hernia
A hernia in the groin area is the most common of all types of hernias, and is 6 times more common among men than among women. With this disease, the peritoneum and internal organs of the abdominal cavity (usually the intestines) protrude under the skin through the inguinal canal. This is faced by men who are associated with hard work and have an enlarged inguinal and umbilical ring. A hernia occurs because the thinnest and weakest parts of the abdominal wall are located in the groin area.
At first there may be no pain, just a bulge. Sometimes it can be reduced, but in a lying position it may disappear. But with further development of the disease, complications are possible. Thus, pain in men in the left groin is caused by strangulation of a left-sided inguinal hernia. The same can happen on the right side if the protrusion occurs on the right.
Skin diseases of the male genital area
Traditionally, the XVII Congress “Men's Health” was held as an interdisciplinary event, in which representatives of a wide variety of medical specialties took part. In particular, one of the sessions was devoted to the diagnosis and treatment of patients with skin diseases of the male genital area. Several reputable Russian dermatovenerologists presented reports on this topic.
Skin lesions of the groin area in men: taxonomy and clinical review
Head of the Department, Professor of the Department of Dermatovenereology and Cosmetology of the Central State Medical Academy of the Administration of the President of the Russian Federation, Chief Researcher of the International Scientific and Research Center of Moscow State University. M.V. Lomonosov, Doctor of Medical Sciences, Professor Andrei Nikolaevich Lvov said that genital rashes in men have a conditional classification and are divided into infectious and inflammatory diseases (the largest group), connective tissue diseases, dermatoses, oncological diseases and viral diseases. He noted that the bulk of errors in diagnosing genital rashes are made by doctors of three clinical specialties - obstetricians-gynecologists, urologists and proctologists. “Not everything that looks like balanitis actually is. At the same time, there is a fairly wide range of comorbid situations when classic dermatosis manifests itself in the same way as syphilis. On the one hand, psoriatic papules and plaques, and on the other hand, syphilitic psoriasiforms (papular elements of secondary syphilis) imitate psoriasis, incl. genital localization. In this case, we are talking about a combination of two conditions, and this is easy to prove, since at the beginning of penicillin therapy all psoriasis forms disappear. In another example, erosive papules of the scrotum look classic, and annular papules with secondary syphilis on the glans penis resemble lichen planus. They are distinguished by a rich red color, swelling and isolation. In general, it is not so difficult to diagnose syphilis, it is important to remember about it in time,” the speaker said and then moved on to the pathogenesis of dermatoses of combined etiology.
“Bacteria or fungi are the primary etiological cause of dermatoses of combined etiology (25% of patients with mixed dermatoses), trigger bacteria and fungi provoke a sharp exacerbation of chronic dermatoses (19% of patients), and the addition of a secondary mixed infection can often be observed (56% of patients with chronic skin diseases ). Patients with dermatoses of combined etiology are indicated for external therapy with combination agents containing topical glucocorticosteroids (TGCS), antimicrobial and antifungal components, he said. “But even when we observe such patients, it is necessary to carry out differential diagnosis, first of all, with a syphilitic infection.”
Lichenoid and erosive dermatoses of the penis: differential diagnosis and principles of therapy
Venereologist, dermatologist of the City Dermatovenerological Dispensary, MD. Irina Olegovna Smirnova dwelled on the features of recognition and treatment of erosive lichen planus and Zun's balanitis: “In this case, first of all, the problem of the clinical picture of erosive lichen planus arises. In the vast majority of cases, it manifests itself in the formation of true erosion, the presence of a Wickham network along the periphery (whitish ridge), and damage to the mucous membranes of the oral cavity and skin. In addition, Zun’s balanitis is not characterized by cicatricial changes,” she explained. – The same picture is observed with psoriasis and focal neurodermatitis: these diseases can be very similar, especially if psoriasis is located only on the genitals. Nevertheless, an atopic history and the absence of balanitis, which can be observed with psoriasis, makes it possible to differentially diagnose focal neurodermatitis.”
Next, the speaker focused on approaches to the treatment of patients with skin diseases of the genital area: “This is always an interdisciplinary approach. At the same time, in addition to treatment, it is always important to pay attention to patient care for the genitals, she noted. – In 2022, Russian Clinical guidelines for the treatment of patients with lichen sclerosus and atrophic lichen were published, which involve therapy with high-strength TGCS (clobetasol, mometasone furoate in the form of an ointment daily, for a course of 4 weeks). Calcineurin inhibitors - CNIs (pimecrolimus, tacrolimus) are less effective and are more often used as maintenance therapy from 16 to 24 weeks. As for the treatment of patients with lichen planus, in this case high-strength TGCS (clobetasol) is used for a course of up to three months; topical CNIs (pimecrolimus, tacrolimus) are less effective. At least 40% of patients are indicated for complex therapy, incl. systemic: prednisolone is used (20 mg/day for 1 week with a dose reduction until complete withdrawal), hydroxychloroquine (20 mg 2 times a day), methotrexate (initial dose 5 mg/week with gradual titration of the dose depending on the formation of the clinical effect to 25 mg /week), mycophenolate mofetil (initial dose 500 mg/day with gradual titration to 1.5 g 2 times a day), surgical treatment (adhesiolysis, Fenton procedure, perineotomy). In this case, it is very important to draw the patient’s attention to basic care for the affected area: undertake gentle cleansing of the mucous membrane and genitals (washing should be done with warm water only with your fingertips no more than 2 times a day; moisturizing the affected area should only occur as indicated - in case of dryness, tightness ); It is not recommended to use products that can increase itching (wet wipes, including baby wipes, medical wipes, medications, rough fabrics and tight clothing). Patients are recommended to use undyed cotton underwear, washed with hypoallergenic detergents. It is also necessary to avoid scratching the affected area and use products that reduce the severity of itching. Adjuvant therapy should be regulated so that the maximum effect is achieved with a minimum amount of drugs.”
Doctor I.O. Smirnova emphasized that the issue of circumcision for lichen sclerosus is always decided individually: surgery is not always necessary after anti-inflammatory treatment, since in 50%, after performing circumcision, symptoms of lichen sclerosus persist (Koebner phenomenon - rash at the site of injury). “Therefore, if a decision is made about circumcision, then the procedure must be performed after anti-inflammatory therapy and under its cover,” summarized Irina Olegovna.
Analysis of international recommendations (IUSTI) for the treatment of patients with sexually transmitted infections
Chief Researcher of the Moscow Scientific and Practical Center of Dermatovenereology and Cosmetology of the Ministry of Health of the Russian Federation, Doctor of Medical Sciences, Professor Mikhail Aleksandrovich Gomberg drew the attention of urologists to the current Order of the Ministry of Health of the Russian Federation dated August 12, 2002 No. 403 “Infections registered in Russia as sexually transmitted (STI).” “All infections were collected in this group so that when making a diagnosis, the doctor must fill out a special form and perform all the actions necessary to identify an STI (involvement of a partner in the examination, examination for other possible infections, etc.). This order mentions the following diseases: syphilis, gonorrhea, trichomoniasis, chlamydia and two viral infections - anogenital warts and genital herpes,” he explained.
Next, Professor M.A. Gomberg noted that although bacterial vaginosis (BV) is not an STI, this disease is combined with the presence of a large number of sexual partners (both men and women), the emergence of a new sexual partner, non-use of a condom during sexual intercourse, and an increased risk of getting other STIs (for example, a woman’s infection with HIV and transmission of this infection to another sexual partner increases 3 times), complications during pregnancy. “But there are two points according to which BV is not classified as an STI: first, BV occurs in women who are not sexually active at all; second, treatment of sexual partners does not affect relapses of BV,” the speaker said.
Further, citing data from a number of studies, he answered the question “can bacteria associated with BV cause urogenital problems in men?” “Men, indeed, may have problems with those microorganisms that are associated specifically with BV,” said Professor M.A. Gomberg. “In this regard, my colleagues and I conducted a study where we focused on the problems associated with urethritis in our patients, assessing their presence of certain microorganisms that were most often associated with BV. We reported the results of this study at one of the congresses on the fight against STIs in Helsinki. This was one of the papers looking at the abnormalities that occur in men with urethritis and how they relate to the changes found in their female partners with BV. Our conclusions were as follows: BV occurs 3 times more often in women who have had sex with men with balanoposthitis or urethritis. The frequency and quantity of two main pathogens (Gardnerella vaginalis and Atopobium vaginae) in the urogenital biotope of the male urethra correlated with inflammation. Our data support the possible sexual transmission of G. vaginalis and other microorganisms associated with BV.”
Mikhail Aleksandrovich said that the above work was continued, as a result of which certain data were obtained on the prevalence of various microorganisms in urethritis, after which it was necessary to answer the question: how to treat patients with urethritis associated with BV in their partners. Such urethritis is Professor M.A. Gomberg and his colleagues proposed a new term - anaerobic urethritis.
Regarding therapy, the speaker said the following: “Nifuratel is a nitrofuran drug that is well tolerated, resistance to it is less likely to develop than to metronidazole, there are forms for systemic and intravaginal use, it also has a good risk/benefit ratio in the treatment of patients with vulvovaginal infections. "Nifuratel is primarily intended for the prevention and treatment of urinary tract infections and has excellent in vitro efficacy against G. vaginalis, Mobiluncus and A. vaginae, without inhibiting lactobacilli."
At the end of his report, Professor M.A. Gomberg recalled that on September 25, 2022, a state control program for the use of antimicrobial agents was launched in Russia. “This strategy defines the state policy to limit the spread of microbial resistance to antimicrobial drugs, biological and chemical agents for the period until 2030 and calls for the prescription of antimicrobial agents for certain indications and mainly from groups of drugs to which resistance of pathogens slowly develops.”
Prevention and treatment of HPV-associated diseases of the anogenital area in men
Dermatologist, Associate Professor of the Department of Dermatovenereology and Cosmetology of the Central State Medical Academy of the Administration of the President of the Russian Federation, Doctor of Medical Sciences. Evgenia Afanasyevna Shatokhina in her report focused on human papillomaviruses (HPV), which are not cultivated in cellular systems, are detected in keratinocytes in the form of episomes, have oncogenic properties and cause tissue transformations, benign or malignant tumors. She noted that in 95% of cases of cervical cancer, about 20 types of HPV are found, most often types 16 and 18. “Anogenital genital warts are a viral disease caused by HPV and characterized by the appearance of exophytic and endophytic growths on the skin and mucous membranes of the external genitalia, urethra, vagina, cervix, and perianal area,” the speaker said. – These diseases are classified as STIs, while 50–80% of the population is infected with HPV, but only 5–10% of infected individuals have clinical manifestations of the disease, asymptomatic carriage is observed in 6–10%, 20–50% of patients are diagnosed with HPV of high oncogenic risk "
Speaking about the pathogenesis of the disease, Dr. E.A. Shatokhina emphasized that HPV has a pronounced affinity for the cells of the epidermis and epithelium of the genital tract. In this case, 4 genes (E1, E2, E6 and E7) provide the processes of replication and transcription of the virion, and the E4 and E5 genes are expressed later, ensuring immune invasion and subsequent release. Early genes E6 and E7 determine the oncogenic potential of the virus. L1 and L2 encode structural proteins of the virus and are inverse agonists for the body's pattern recognition receptors, such as TLR, which in turn trigger a complex of protective reactions in the form of the production of inflammatory cytokines. Thus, the genome of the virus contains a complete set of genes that ensure its penetration into a human cell, replication and subsequent release.
Mentioning vaccines for the prevention of HPV infections, the speaker named Cervarix, Gardasil and Gardasil 9, and the nucleoside-like compound imidazoquinoline was recommended for the treatment of HPV infections.
Precancerous diseases and tumors of the skin of the male genital organs
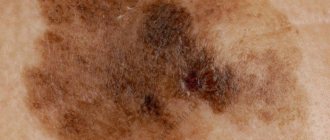
Oncologist, head of the oncosurgical department of tumors of the skin and soft tissues of the Moscow Clinical Research Center, Doctor of Medical Sciences, Professor Konstantin Sergeevich Titov began the report with a description of benign tumors of the skin of the male genital organs. In particular, he explained that seborrheic keratosis (SK) of the skin is the most common benign tumor of skin keratocytes in fair-skinned elderly and senile people on the skin of the chest and back. The etiology of KS is unknown, but a combination of genetic and environmental factors has been suggested, with an association with type 2 diabetes mellitus. KS is quite common on the male genital organs. KS is usually diagnosed clinically (history, examination and dermatoscopy), and differential diagnosis must also be made with anogenital warts, nevus, bowenoid papulosis, pigmented basal cell carcinoma and melanoma. In more complex cases, a biopsy is necessary. Multiple KS is often misdiagnosed as genital warts.
Professor K.S. Titov reported that KS usually does not require treatment, while the erroneous diagnosis of KS as an STI creates in the patient a feeling of guilt and emotional distress, which negatively affects the quality of his sex life. Therefore, it is very important to reassure the patient that KS is not an STI. “Verucous KS is best treated with curettage (using a sharp disposable curette) with minimal electrocautery under local anesthesia,” he explained.
Regarding the diagnosis and treatment of patients with epidermal cysts and idiopathic scrotal calcification, the speaker said the following: “When diagnosing, it is necessary to exclude metabolic disorders of calcium, phosphorus and parathyroid hormone if the patient has idiopathic scrotal calcification. Opening a cyst without removing it can lead to the development of a foreign body reaction with severe inflammation and cellular infiltration in the skin, followed by fibrosis. Histological examination of idiopathic scrotal calcification indicates calcified dermal deposits without a true epithelial lining. A focal granulomatous foreign body reaction with fibrosis and focal transepidermal clearance of calcium deposits may also be observed. The main method of treatment is surgery: simple excision under local anesthesia is recommended for single cysts; for multiple lesions, the operation is recommended to be performed under general anesthesia.”
At the end of the report, Professor K.S. Titov focused on the treatment options for patients with penile melanoma: “The method of choice is excision of the skin tumor with an indentation from its edge. In the presence of verified metastases of the inguinal lymph nodes, bilateral inguinal lymph node dissection is performed. Imiquimod can be used in the treatment of a patient with penile melanoma in situ, confirmed by incisional biopsy. Patients with metastatic forms of cutaneous melanoma are treated using immunotherapy with immune checkpoint inhibitors, targeted therapy (if the tumor has driver mutations in the BRAF and C-kit genes), stereotactic radiation therapy, and in some cases, surgical removal of distant solitary or residual melanoma metastases after conservative treatment."
Topics and tags
Diseases of the external genitalia
Magazine
Newspaper "Moscow Urologist" No. 2 2021
Comments
To post comments you must log in or register
Diseases of the reproductive system
Orchitis is inflammation of the testicles. In addition to pain in the groin, there is pain in the perineum and the affected testicle. If the disease has become chronic, then the man experiences aching pain in the groin.
Testicular torsion. Causes severe groin pain in men. It is acute, initially occurs in the scrotum, and very suddenly. The pain is so severe that it can cause nausea and vomiting.
Funiculocele is a cyst of the spermatic cord. Causes discomfort in the scrotum, which intensifies after physical activity, and a feeling of fullness. Pain is more often observed during sexual intercourse.
Varicocele is a varicose vein of the spermatic cord. The pain can be either mild or severe. Shooting and burning pain in the groin in men is most often caused by varicocele.
Other possible reasons:
- acute prostatitis,
- prostate adenoma,
- vesiculitis,
- balanoposthitis,
- prostate cancer.
Treatment
Treatment of urological problems is a long and scrupulous process. In most cases, only a set of measures can help.
We use methods such as:
- drug treatment;
- physical therapy;
- prostate massage;
- treatment with active oxygen (ozone therapy);
- mud therapy (Dead Sea mud);
- medical and medicinal droppers;
- adjusting the patient’s lifestyle and nutrition;
- development of an individual prevention program;
- monitoring the patient's condition after treatment.
Diseases of the urinary system
Urolithiasis disease. This is one of the common causes of acute groin pain in men. If the resulting stone has blocked the left or right ureter, the symptom may appear in the groin on the left or right. This is associated with renal colic. In addition to pain in the groin, a man will feel acute pain along the ureter (in the abdomen), which radiates to the external genitalia and bladder. Additionally, there is a frequent urge to urinate and blood in the urine.
Other diseases of the urinary system can cause pain:
- urethritis,
- cystitis,
- hydronephrosis,
- bladder cancer.
Treatment of candidiasis in the groin with folk remedies
The regimen and duration of treatment for candidiasis in the genital tract may be reduced.
In the event that the patient uses traditional methods in addition to medications.
Traditional medicine, of course, cannot cope with the disease when used in isolation.
However, they can speed up the effect of medications and alleviate the symptoms of the disease during the main treatment.
Naturally, the use of traditional medicine recommendations is possible only after the doctor’s approval has been received.
The patient may be recommended, for example, lotions with chamomile infusion or chamomile baths.
Herbs that have an antibacterial effect have a good effect.
They also prevent the development of secondary infectious processes.
All patients, regardless of the duration of treatment and the regimen used, are recommended to undergo follow-up tests after treatment.
With their help, it will be possible to confirm that the therapy was successful.
Based on the results of control tests, the patient is also deregistered from the skin and venereal disease clinic, if he was there.
Diseases of the musculoskeletal system
ARS syndrome is inflammation and degeneration of tendons and ligaments attached to the pubic bone and symphysis. Athletes face this. Pain is observed in the lower abdomen and groin area, intensifying with hip abduction.
Hip sprain. May be caused by a fall or sudden abduction of the hip while performing any exercise.
Coxarthrosis, arthropathy, femoral neck fracture. These are diseases associated with damage or disease to the hip joint and the proximal part of the femur where it attaches to the joint.
Diagnostic stages
If symptoms appear, contact a urologist. He may prescribe an additional consultation with a venereologist, allergist, or dermatologist, depending on the developing clinical symptoms. Laboratory and instrumental tests are required to determine the exact cause.
- General inspection
. The doctor examines the man’s penis and adjacent tissues. It can detect redness, inflammation, swelling, discharge and other negative reactions. - Anamnesis collection
. The patient explains his complaints and talks about recent changes in his life. He is always asked about hereditary diseases in the family. - PCR technique
. Detects any types of viruses and bacteria contained in urine or discharge from the penis. - Bacteriological culture
. The mucus is inoculated on a nutrient medium, and the exact type of bacterial pathogen is identified. Determine the antibiotics to which it is sensitive. - General blood test, biochemical test, general urine test
. These are general clinical studies that indicate the condition of the body as a whole, separately the blood, immunity and urinary system.
Thanks to diagnostic tests, you can accurately determine the diagnosis.
Why is it important to see a doctor?
There are many causes of groin pain, and the nature of the symptom can only be determined after a thorough diagnosis.
Self-medication can make the problem worse, so it is important to see a doctor as soon as possible. The State Urology Center provides qualified medical care under the compulsory medical insurance policy, so the procedures and treatment prescribed by the doctor will be free for you. First, sign up for a consultation with a specialist, then we can relieve you of unpleasant symptoms and restore your health. April 19, 2021
Hakobyan Gagik Nersesovich - urologist, oncologist, MD, doctor of the highest category, professor
All the symptoms of the disease...
Which doctor should I go to for help with candidiasis in the groin?
Often patients are interested, if they still could not avoid the development of pathology, which doctor should be consulted first.
Only a doctor specializing in venereology can fully assess the characteristics of the rash, the severity of the lesion and other symptoms of candidiasis.
He is the one who treats and diagnoses STIs, which include candidiasis.
However, there are alternatives to a venereologist.
For example, you can seek help from a mycologist.
A doctor, unlike a venereologist or infectious disease specialist, has a narrower specialty, dealing with diseases caused by various pathogenic fungi.
Since candida is a fungus, a mycologist can help a patient with symptoms of candidiasis.
Another option for men is a urologist, and for women a gynecologist.
These professionals, by virtue of their profession, are familiar with STIs and their symptoms, including candidiasis.
Moreover, urologists and gynecologists are often so familiar with such diseases that they can recommend treatment on a par with venereologists.
This is explained by the fact that the genitals are often affected by STDs.
Doctors specializing in diseases of these organs should be able to diagnose such pathologies and refer patients to the appropriate doctor, if possible.
Classification of pain in the perineum
The identification of different groups, categories or classes of pain symptoms occurring in the groin is based on various parameters. All of them are presented in our table below.
| Type of pain | Distinctive features |
| Classification based on predisposing factor | |
| Primary | Develops as a result of a perineal injury or due to a neurological disorder. |
| Secondary | Pain radiating to the perineum due to existing diseases of the internal organs. |
| Classification by origin | |
| Visceral | It occurs due to compression or irritation of the nerves located in the organs of the genitourinary system. |
| Neurogenic | Occurs due to damage to nerve tissue in the perineal area. |
| Psychogenic | It occurs as a result of disturbances in the patient’s psycho-emotional state due to stress, depression, and neuroses. |
| Classification by duration of manifestation | |
| Acute | It appears brightly and lasts for a short time: from a couple of minutes to several hours, but not more than 24 hours. |
| Chronic | It is mild and lasts for a long time: several months. |
| Classification by nature of manifestation | |
| Pulling | Such painful symptoms are characterized by duration and often intensify in a sitting position or during defecation. It is typical for the postpartum period and occurs due to swelling and sprains, and also develops with the following diseases:
|
| Sharp, sharp | It is typical for any perineal injuries, ranging from ordinary bruises to muscle ruptures. It is very intense and can even cause loss of consciousness. It may also occur with diseases such as:
|
| Bursting | Most often it occurs in women before childbirth, when the body is preparing for this process, as well as during inflammatory processes of the vaginal mucosa. |
Pain in the perineum in pregnant women
Patients often come to the gynecological department of our clinic with the question of why the perineum hurts during pregnancy and how dangerous it is. Normally, such symptoms are associated with the growth of the fetus and its descent. It is typical for the 3rd trimester - it is during this period, due to the development of the child, that there is an impact on the ligaments, nerves and muscles of the mother’s body, which are stretched. However, the occurrence of such symptoms in the early stages may be a sign that there is a high risk of miscarriage.
It is not uncommon for the fetus to put pressure on the nerve that runs nearby. The pain that occurs in this case limits movement and does not stop until the fetus changes position. Modern medicine cannot help in this case.
Perineum hurts before childbirth
Severe pain symptoms that occur over a long period of time are a sign that labor is approaching. It is caused by the expansion of the pelvic bones and other processes of preparation for the process, along with the approach of the fetus to the birth canal.
Perineum hurts after childbirth
Painful symptoms are felt by almost all women afterward, although its strength may vary. It depends on the presence/absence of injuries during childbirth. So, it goes away 3-4 days after birth when it occurs due to swelling and stretching of tissues, and persists much longer with ruptures of the perineum and sutures.