Dermatovenerologist
Khasanova
Alina Rashidovna
9 years experience
Make an appointment
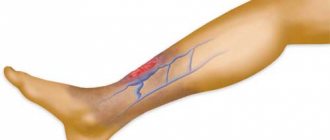
One of the forms of vasculitis that develops as a result of an allergic reaction of the body is erythema nodosum. This is the name for inflammation of the blood vessels that penetrate the epidermis, as a result of which painful pink or bluish nodules form in the dermis and subcutaneous fatty tissue. Vascular damage is local in nature and is limited mainly to the lower extremities.
Why does inflammation of the skin vessels develop?
There are several factors that provoke the onset of the inflammatory process in the vessels of the epidermis:
- bacterial infectious diseases caused by streptococci - scarlet fever, tonsillitis, pharyngitis, otitis media, etc., after which erythema nodosum of the lower extremities develops as a complication of the disease;
- long-term systemic disease - tuberculosis, lymphogranulomatosis, trichophytosis, yersiniosis;
- long-term course of treatment with antibiotics, bromides, salicylates, iodides or sulfonamides;
- vaccination;
- ulcerative colitis;
- cancer;
- Behçet's disease;
- pregnancy and the associated hormonal changes in the female body, and the risk of developing erythema nodosum increases significantly if the pregnant woman has a history of chronic infectious foci;
- hereditary predisposition to the disease: it is often diagnosed in several generations of the same family or in close relatives;
- allergies, which contribute to the development of a chronic form of pathology.
Erythema nodosum most often affects young people 20-30 years of age. Before the onset of puberty, the incidence is the same in boys and girls, but starting from adolescence, the disease occurs mainly in women, among whom the incidence is 3-6 times higher than in men. There is a certain seasonality: in winter and spring, the number of visits to the doctor about this increases significantly due to decreased immunity and an increase in the number of infectious diseases, including streptococcal infections.
Causes
These are various infectious causes: streptococcal infections (tonsillitis, scarlet fever), tuberculosis, yersiniosis, lymphogranuloma venereum, leprosy, histoplasmosis, coccidiosis. In a word, everything that we call “chronic foci of infections.” Non-infectious: sarcoidosis (a fairly common cause of erythema), nonspecific ulcerative colitis. It is also necessary to note the allergic nature of erythema, which most often occurs when taking sulfonamide drugs (sulfalene, sulfodimethoxine) and contraceptives.
Clinical manifestations of pathology
The characteristic symptoms of erythema nodosum allow specialists to accurately recognize the disease.
- Acute onset with a sharp deterioration in condition, chills, signs of fever, weakness, and loss of appetite.
- The appearance of nodular rashes on the skin, and the nodes form in the lower, densest layers of the dermis or in the subcutaneous layer of fatty tissue and rise above the skin level. The size of the nodes varies from 0.5 to 5 cm, swelling forms around them, due to which the boundaries of the node are blurred, marked only by a change in the color of the smooth skin to bright pink or bluish.
- Rapid increase in the size of nodes formed under the skin. After some time, growth stops.
- Soreness of the nodes is one of the characteristic symptoms. It can appear spontaneously or only when you press on the inflamed area of skin.
- Pain and inflammation in the joints is another characteristic sign. Large joints become inflamed in about a third of patients: tissue swelling appears and the temperature rises locally. Arthropathy and a feeling of stiffness are characteristic of most cases of the disease.
- After two to three weeks, the nodes begin to shrink and then disappear completely. In their place, spots with discolored skin remain for some time, and peeling of the skin is possible. At the same time, inflammation of the joints is resolved.
Acute erythema nodosum lasts about a month. In the absence of proper treatment, the disease becomes chronic with periodic remissions and exacerbations. Relapses are characterized by the formation of single inflamed nodes, which persist for several months with mild or completely absent signs of infectious intoxication.
Are you experiencing symptoms of erythema nodosum?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
General therapeutic recommendations
- Bed rest is recommended, which may lead to spontaneous resolution of the disease within a relatively short period of time. Since the disease resolves on its own, the most important thing is to identify and treat the underlying cause.
- Overall, erythema nodosum is a relatively common condition and is most often benign. Typically, the diagnosis is made clinically. Treatment is mainly symptomatic and consists of bed rest and non-steroidal anti-inflammatory drugs and potassium iodide. Since the disease resolves on its own, the main challenge is identifying and treating the cause of the condition.
Treatment of acute form
Potassium iodide (a preparation consisting of 76% iodine and 23% potassium) is the treatment of choice. Once ingested, potassium iodide is rapidly absorbed in the digestive tract and distributed throughout the intercellular space. Iodine is concentrated in the thyroid gland, as well as in other tissues such as the salivary glands, gastric mucosa and mammary gland. Potassium iodide can work quickly enough that it is easy to assess the effectiveness of treatment. The drug is prescribed orally at 300 mg 3 times a day. Complete remission of the lesions occurs within 10-14 days after the medication is prescribed, especially if the drug is started immediately after the onset of the disease. The best response is observed in patients with EU, which is associated with systemic symptoms such as fever, joint pain and the presence of C-reactive protein. Sometimes nausea and vomiting occur, but there is usually no need to stop treatment. Adverse skin reactions may include erythematous, purpuric, urticarial, acneiform, nodular, pustular, and vegetative lesions. In addition to these rather minor side effects, there may be more significant adverse reactions in pregnant women and in patients with a history of kidney or thyroid disease. Severe hypothyroidism secondary to exogenous iodide ingestion has been reported. Blocking its organic binding in the thyroid gland with an excess of iodide, which results in the cessation of the synthesis of thyroid hormones, is known as the Wolf-Chaikoff effect.
The mechanism by which potassium iodide exerts its effect is not clear. One hypothesis suggests that potassium iodide may cause the release of heparin from mast cells, and heparin in turn suppresses cellular immunity. The drug may also modulate neutrophil function by inhibiting the production of hydrogen peroxide and hydroxyl radicals. These oxygen intermediates are so reactive that they can damage tissue. Potassium iodide, by preventing the production of intermediate oxygen products, protects tissue from damage due to autoxidation.
- In the acute form, regardless of its etiology, bed rest and potassium iodide are recommended.
- In the case of an acute form with fever and arthralgia, treatment is carried out with colchicine at a dose of 1 mg/day for 1 month.
- Erythema nodosum may suggest sarcoidosis. In 80% of patients, sarcoidosis resolves spontaneously, and therapy is rarely indicated. Treatment in this case is the same as for the acute asymptomatic form, as described above.
- Erythema nodosum as a symptom of gastrointestinal infections is treated with erythromycin at a dose of 250 mg 4 times a day for 4-6 weeks.
- For disease caused by fungal infection, especially kerion of the scalp, the disease responds to griseofulvin, which is prescribed for a period of 6 weeks.
- Erythema nodosum, indirectly caused by oral contraceptives, often regresses when taking them is stopped.
- Acute forms of hepatitis B and C are sometimes associated with erythema nodosum. The nodules usually resolve slowly after the acute phase of the disease. A strong association has been reported between hepatitis B vaccination and the occurrence of the disease, with lesions resolving spontaneously.
Treatment of the chronic form
Erythema nodosum is a debilitating chronic disease for which many treatment options have been proposed, but none are universally effective. Although patients respond quickly to corticosteroids, the risk of chronic use prompts the search for an alternative approach.
Chronic cases often do not respond to large doses of aspirin, but may respond dramatically to the anti-inflammatory effects of indomethacin at doses of 100-150 mg/day. Suppression of the process by indomethacin is associated with blocking the activity of prostaglandin synthesis in subcutaneous adipose tissue, which affects both the cellular and humoral immune response.
The chronic form can also be successfully treated with naproxen. However, indomethacin is superior to systemic corticosteroids and may also have advantages over other, less potent nonsteroidal anti-inflammatory drugs.
Hydroxychloroquine is an effective and safe alternative therapy for some patients at a dose of 200 mg twice daily, which is then tapered to 200 mg once daily for 4 months.
Treatment of erythema nodosum leprosum
Thalidomide is currently recommended as first-line therapy for the treatment of leprosy EU. Sheskin analyzed data on 4,522 cases of erythema nodosum leprosy and found the drug to be 99% effective, although thalidomide has no direct effect on Mycobacterium leprae. Resolution occurs 24-48 hours after initiation of thalidomide therapy. The drug has also been reported to have a beneficial effect on reactive polyneuritis. Erythema nodosum leprosum is associated with increased levels of TNF-a and interferon-γ. After thalidomide therapy, the level of TNF-a in the serum of patients decreased, and the number of helper T cells also decreased. Thalidomide is known for its inhibitory effect on TNF-a. The optimal dose to obtain a rapid effect is 400 mg/day followed by maintenance therapy at a dose of 100 mg/day. Duration of treatment ranges from several weeks to several years. Plasma replacement has also been reported to be effective and free of relapse. This method was used when traditional treatments did not work.
Diagnostic methods
Laboratory test results do not provide a basis for definitively diagnosing erythema nodosum in a child or young person. They are aimed, first of all, at identifying the causes of the disease and its accompanying pathologies. The patient may be prescribed:
- clinical blood test;
- bacterial culture of nasopharyngeal mucus microflora to identify streptococci;
- stool culture for suspected yersiniosis;
- tuberculin diagnostics;
- skin allergy tests;
- blood test for rheumatoid factor and consultation with a rheumatologist;
- tissue biopsy of the nodular formation and histological examination of the sample to identify the inflammatory process in the walls of the capillaries.
After clarifying the etiological factor, concomitant vascular pathologies or foci of chronic infection, the patient may need consultation with a specialized specialist - an infectious disease specialist, pulmonologist, otolaryngologist, phlebologist, etc., as well as additional instrumental studies.
Diagnostics
The diagnosis is determined by clinical manifestations, but other studies are also prescribed to confirm it:
- biopsy;
- skin tests;
- chest x-ray;
- general blood and urine analysis;
- throat swab;
- Ultrasound of internal organs.
Differential diagnostics are carried out to exclude diseases:
- extrapulmonary tuberculosis;
- panniculitis;
- lipogranuloma;
- nodular vasculitis;
- migratory thrombophlebitis;
- skin calcification;
- insect bites;
- acute urticaria.
Therapy of the inflammatory process
Treatment of erythema nodosum is aimed, first of all, at getting rid of foci of chronic infection or other causative pathology. It includes:
- antibiotic therapy if the inflammatory process is infectious;
- desensitizing therapy if the cause of the disease is an allergic reaction of the body;
- taking anti-inflammatory drugs to relieve inflammation and relieve pain;
- plasmapheresis, cryopheresis or hemosorption to quickly eliminate intoxication;
- corticosteroid and anti-inflammatory ointments for inflamed joints and erythema nodes;
- physiotherapeutic treatment - ultraviolet irradiation, laser therapy, background cutter, magnetic therapy, etc.
For pregnant patients, clinical recommendations for erythema nodosum are significantly limited, since many drugs are undesirable to use. Previously, this disease served as a justification for artificial termination of pregnancy, but it has now been proven that it does not affect the development of the fetus.
Treatment
Treatment of erythema nodosum should begin with identifying its cause, and it largely consists of eliminating this cause. However, this is not always possible. In cases where erythema nodosum is associated with infectious factors, antibiotics are indicated. The effect is significantly enhanced when antibiotics are combined with small doses of corticosteroids. Anti-inflammatory drugs are also used - acetylsalicylic acid, indomethacin (methindol), butadione, ibuprofen and others. Potassium iodide is quite effective in daily doses of 300-900 mg for 2-4 weeks. In cases of a clear connection between exacerbations of erythema nodosum and menstruation, oral contraceptives are indicated for 3-6 cycles. The use of such drugs for medicinal purposes is permissible after consultation with a gynecologist. Of the physiotherapeutic methods, the following have a good effect on erythema nodosum: ultraviolet irradiation in erythema doses, magnetic therapy, laser therapy, phonophoresis with hydrocortisone on the area of inflammatory nodes or affected joints.