The skin disease caused by a fungus on the face is a type of mycosis of smooth skin, but has some features of external manifestations.
Mycosis of the facial skin is caused by a fungus of the genus Trichophyton, so the disease is classified as trichophytosis. The lesion does not involve the area of skin under the beard and mustache in men. The pathology is considered separately from mycosis of smooth skin, since its manifestations are often confused with pityriasis versicolor, rosacea, seborrheic dermatitis, or symptoms of lupus. Therefore, treatment for mycosis of the facial skin is prescribed by a dermatologist only after a thorough diagnosis.
The disease is quite rare. Infection occurs mainly through transmission of the pathogen:
- from animals;
- less often from a sick person to a healthy one.
At the same time, foci of infection may appear on the scalp or torso.
Mycosis of the facial skin causes not only health problems. Its signs are clearly visible and therefore cause aesthetic discomfort in the patient and surrounding people.
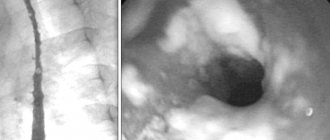
Signs of the disease are presented in the photo of facial skin mycosis:
Rubrophytia
The cause of rubromycosis (rubrophytosis) is the red fungus trichophyton (Trichophyton rubrum). The fungus got its name for its ability to form a red pigment when growing on Sabouraud's nutrient medium. The widespread distribution of fungi in the environment is the cause of frequent human mycoses.
Rubrophytosis affects the skin of the feet, interdigital spaces on the hands and feet, and nails. The skin of the trunk and large folds is slightly less commonly affected. Even less commonly, the fungus affects the skin of the face and head. A sick person and his personal belongings are a source of infection in public places - swimming pools and baths. The disease is transmitted to all members of his family. Decreased immunity and failure to comply with personal hygiene rules contribute to the development of the disease.
Skin manifestations of rubrophytosis
The disease manifests itself in the form of an erythematosquamous and follicular-nodular form.
Erythematosquamous form
The erythematosquamous form is characterized by the appearance of large spots, on the surface of which papules and vesicles are visible. Dilated capillaries give the lesion a reddish appearance, on the surface of which peeling is noted. The affected area becomes covered with crusts over time. The lesion is surrounded by an intermittent ridge, on the surface of which papules and vesicles are visible.
Follicular nodular form
The follicular nodular form of rubrophytosis is a continuation of the development of the previous form as a result of the lack of proper treatment.
Rice. 6. The photo shows rubrophytia (erythematosquamous form).
Rice. 7. Rubrophytosis of the facial skin (fungus trichophyton rubrum).
Rice. 8. The photo shows rubrophytosis of the skin of the breast (fungus trichophyton rubrum).
Rice. 9. The photo shows rubrophytia (a common form). Fungus trichophyton rubrum.
Treatment of mycosis of the facial skin
Before starting treatment for mycosis of the facial skin, the doctor diagnoses the disease. It includes clinical assessment and laboratory tests. A fungal infection is indicated by an edematous ridge along the periphery of the lesion. The diagnosis is confirmed when the pathogen is detected in a skin scraping.
External antifungal drugs are used for therapy. One of the effective remedies is Clotrimazole lotion for nails and skin. It is more convenient to use than ointment or cream, it is quickly absorbed and does not cause skin irritation. You can buy this drug for the treatment of mycosis of the facial skin in Moscow or the regions on our website. It has an affordable price.
The lesion needs to be treated twice a day. The duration of the course is determined by the doctor, usually it is about a month.
If the patient begins to uncontrollably use corticosteroid creams in an attempt to independently get rid of itching and inflammation, the disease may be complicated by fungal folliculitis. In this case, it is necessary to take antifungal drugs orally. As a result, the cost of treatment increases significantly. Therefore, you should consult a dermatologist before using any skin treatment.
Microsporia
The causative agent of the disease is fungi of the genus Microsporum. The source of infection is cats with trichophytosis; less commonly, the disease is transmitted from dogs. Very rarely the disease is transmitted from a sick person. Mushrooms are very stable in the external environment. They live on skin scales and hair for up to 10 years. Children get sick more often, as they are more likely to come into contact with sick stray animals. In 90% of cases, fungi affect vellus hair. Much less often, microsporum affects open areas of the skin.
Skin manifestations of microsporia
The disease is manifested by the presence of round-shaped lesions. Along their periphery there is an inflammatory ridge with blisters and crusts, rising above the surface of the skin. Peeling is observed on the surface of the affected area. More often there is only one focus. Less commonly, multiple lesions no more than 2 cm in diameter appear. The lesions may merge.
Rice. 10. The photo shows microsporia (lesion focus).
Rice. 11. The photo shows microsporia of the facial skin.
Rice. 12. The photo shows microsporia of the skin of the face and neck. Multiple lesions.
Rice. 13. The photo shows microsporia of the scalp.
Rice. 14. The photo shows microsporia of the skin of the hand.
Rice. 15. The photo shows microsporia of the skin of the body (fungus of the genus microsporum).
Rice. 16. The photo shows microsporia of the skin of the face and eyelids.
Rice. 17. The photo shows microsporia of the facial skin. Multiple lesions.
Rice. 18. The photo shows microsporia of the skin of the lower eyelid of the left eye (fungus of the genus microsporum).
Rice. 19. The photo shows microsporia of the facial skin. Characteristic signs.
Trichophytosis
The culprit of the disease is fungi of the genus Trichophyton, which parasitize the skin of humans, cattle and rodents. The disease is most often recorded in the fall, when field work begins. Then the source of the disease becomes hay and straw. In this case, exposed areas of the body are affected. Fungi that parasitize humans can become a source of trichophytosis. The disease is highly contagious (infectious). The person himself and his things are the source of infection. With this form of trichophytosis, open areas of the body are also affected, but with a prolonged course, the skin of the buttocks and knees can be affected.
Skin manifestations of trichophytosis
The affected areas of the skin are round in shape, bright red, similar to those with microsporia, but much larger, with elements of peeling and small nodules. There is an inflammatory ridge along the edges. Fungal infection occurs in the form of 3 forms, which, as the disease develops, replace each other: superficial form, infiltrative and suppurative.
Rice. 20. The photo shows trichophytosis (fungus). The lesion is large.
Rice. 21. The photo shows trichophytosis of the facial skin.
Rice. 22. The photo shows trichophytosis (chronic form).
Rice. 23. The photo shows trichophytosis of the beard and mustache area (fungus of the genus trichophyton).
Rice. 24. The photo shows trichophytosis of the smooth skin of the forearm.
Rice. 25. The photo shows trichophytosis of the skin of the trunk.
Rice. 26. The photo shows trichophytosis of the skin of the face (left) and hand (right).
Prevention
When the first symptoms of the disease appear, you should consult a doctor and begin treatment. Independent use of antifungal and other medications can lead to attenuation of the signs of the disease and the formation of carrier status of the pathogen. At the same time, humans remain a dangerous source of infection.
During treatment, family members of the patient need to carefully monitor the cleanliness of their hands and face. It is useful for both the sick person and those around them to use preventive measures to avoid fungi getting on healthy skin. One of them is Mycospray, which, when used regularly, effectively prevents the development of fungal infections.
The patient should have separate bedding and towels, which must be boiled when washing.
After eliminating the symptoms of the disease, the patient must visit the dermatologist several more times and undergo the necessary tests. This will help avoid relapse of the pathology or the formation of a fungal carrier state.
Pityriasis versicolor or versicolor versicolor
Tinea versicolor is a fairly common disease. The disease is more common in young and middle-aged people. Fungi parasitize in the uppermost layers of the skin and in the areas of hair follicles. Under certain conditions they can cause disease. It is believed that the cause of the disease is a change in the chemical composition of sweat due to excessive sweating. Diseases of the stomach and intestines, endocrine system, neurovegetative pathology and immunodeficiency are the trigger for the development of pityriasis versicolor. Fungi infect the skin of the body. Lesions are often found on the skin of the chest and abdomen. The skin of the head, extremities and groin areas is much less frequently affected.
Skin manifestations of pityriasis versicolor
With pityriasis versicolor, pink spots appear, the surface of which slightly peels off. The spots tend to merge. Their color changes over time to light or dark brown.
Rice. 27. The photo shows pityriasis versicolor of the facial skin.
Rice. 28. The photo shows facial skin with pityriasis versicolor.
Rice. 29. The photo shows pityriasis versicolor of the skin of the chest.
Rice. 30. The photo shows pityriasis versicolor of the skin of the chest and torso.
Rice. 31. Pityriasis versicolor of the skin of the back.
Rice. 32. Pityriasis versicolor (fungus) of the skin of the hands.
Seborrheic dermatitis
Seborrheic dermatitis is caused by the lipophilic fungi Malassezia furfur (Pityrosporum). Fungi parasitize the skin of many people. The scalp is affected by the fungus Pityrosporum ovale (P. ovale). Fungi Pityrosporum orbiculare (P. orbiculare) infect the skin of the body. Pathogens concentrate in areas of greatest accumulation of sebum, which is produced by the sebaceous glands. The causative agents of seborrheic dermatitis use sebum in the process of their life. The rapid growth of fungi is provoked by neurogenic, hormonal and immune factors.
With seborrheic dermatitis, the lesions are widely localized, but most often the disease affects the scalp. Lesions may appear at the border of hair growth, eyebrows and eyelashes. The skin in the mustache and beard area is affected. Often lesions are recorded in the nasolabial folds, on the skin of the ear canals and behind the ear areas. Less commonly, the skin of the sternum and body folds is affected.
The pathogen can infect the skin around the anus and genitals. In the case of negative developments, the disease becomes widespread.
Skin manifestations of seborrheic dermatitis
Skin manifestations of seborrheic dermatitis are represented by areas of inflammation with elements of peeling. If the process is localized in open areas of the skin, then the inflammatory component becomes less noticeable, and peeling intensifies. Sometimes the lesion becomes covered with hemorrhagic crusts. The disease is sometimes accompanied by itching, which can be quite intense. When a secondary infection occurs, suppuration is noted.
Rice. 33. Seborrhea in the photo. Damage to the scalp.
Rice. 34. Seborrhea in the photo. Damage to the eyelash area.
Rice. 35. The photo shows seborrhea. Damage to the ear area.
Rice. 36. Seborrhea in the photo. Damage to the ear canal area.
Rice. 37. The photo shows seborrheic dermatitis (facial skin lesions).
Rice. 38. The photo shows seborrheic dermatitis (damage to the mustache area).
Candidiasis
The culprit of candidiasis is yeast-like fungi of the genus Candida, which are widespread in the environment. They constantly, starting from the moment of birth, parasitize the skin and mucous membranes. The disease is promoted by a sharp decrease in immunity and the prescription of long courses of broad-spectrum antibiotics. A large number of mushrooms can get on human skin at once. In some professions, the pathogen reaches a person constantly in small portions.
With candidiasis, changes appear primarily on the skin of large and small folds of the body. As the disease develops, the lesions spread to the skin of the body. Somewhat less frequently, lesions are observed on the skin of the palms and soles. The disease often affects infants. Patients with diabetes mellitus and severe somatic pathology are at risk for candidiasis. The disease lasts a long time. Recurs often.
Skin manifestations of candidiasis
Initially, the affected areas acquire a reddish color, against which multiple small bubbles are visible. The process is spreading very quickly. The reddish color changes to deep red. In place of the vesicles, areas of erosion appear. The boundaries of the lesion are clearly defined. Along its periphery, areas of the exfoliated stratum corneum of the epidermis are visible.
Rice. 39. The photo shows candidiasis (facial skin lesions).
Rice. 40. The photo shows candidiasis (skin lesions on the lower part of the face).
Rice. 41. The photo shows candidiasis (facial skin lesions in a child).
Rice. 42. The photo shows candidiasis of the skin of the body.
Rice. 43. The photo shows candidiasis (common form).
According to scientific publications in recent years, against the background of the protracted COVID-19 pandemic, there is a tendency towards an increase in fungal complications both in the acute period and after recovery from coronavirus pneumonia. Especially if the disease was severe and the patient was treated in hospital for a long time.
According to some reports, in approximately 20% of patients with COVID-19 in the ICU, when septic complications develop, the cause of deterioration is the addition of fungal microflora. Diagnosis in such cases is complicated by the nonspecificity of clinical manifestations and the complexity of laboratory identification methods.
The outbreak of “black fungus” in India drew the closest attention of scientists around the world to the problem of invasive (deep) mycoses. Leading researcher at the Republican Scientific and Practical Center for Pediatric Oncology, Hematology and Immunology, Candidate of Medical Sciences, spoke about this in an interview with Medvestnik. Sciences, Associate Professor Mikhail Chernovetsky.
Mikhail Anatolyevich, why has the problem of invasive mycoses worsened during the COVID-19 pandemic?
In fact, this problem is always extremely relevant for certain categories of patients whose condition is associated with immunosuppression. In particular, these are patients with oncological, hematological diseases, after hematopoietic stem cell transplantation (HSC) or organ transplantations, suffering from type 1 and 2 diabetes mellitus, who have undergone extensive surgical interventions, who have been in the ICU for a long time with a central venous catheter, on Ventilation
In such cases, there is always a risk of bacterial and fungal complications. Usually, a bacterial infection develops first, which is treated with antibiotics, after which fungal microflora joins. All this is also typical for patients with COVID-19, severe forms of which are associated with disruption of local and systemic immune defense mechanisms. The situation is aggravated by inadequate prescription of antibiotics and systemic glucocorticosteroids (GCS).
What types of fungal microflora cause invasive mycoses?
In the first place are yeast fungi, mainly of the genus Candida, and this is far from the most difficult option in terms of diagnosis and treatment, the main thing is to identify it in time and quickly prescribe adequate antimycotic therapy. Somewhat less common are deep lesions caused by mold fungi, usually of the Aspergillus genus. However, during the COVID-19 pandemic, more and more publications are appearing on the increasing proportion of molds in the structure of systemic mycoses.
The predisposing factor is obviously damage to the pulmonary epithelium by the SARS-CoV-2 virus, which facilitates the penetration of mold microflora into the lungs, since infection with fungi of the genus Aspergillus occurs mainly by inhalation by inhaling spores.
Bread affected by mucor mold. Another trend during the pandemic is that among mold fungi, the etiological role of the so-called mucor fungi, mainly representatives of the genera Mucor, Rhizomucor, Rhizopus, is increasing. The systemic lesions they cause are called “mucoromycosis”.
Mucormycosis. These are very aggressive, rapidly developing infections with damage to internal organs and tissues and high mortality.
By the way, the “Indian black fungus” that frightened the whole world also refers to mucor fungi (mainly of the genus Rhizopus). As a rule, it affected patients treated for COVID-19, most often patients with diabetes and who received corticosteroids during treatment, as well as people with weakened immune systems.
Why were there so many cases of eye damage in India that some patients even had to have their vision organs removed?
These were already far advanced states, when the fungal mycelium sprouted into the physiological sinuses of the skull and the orbit of the eye. In the case of mucor fungi, all this happens very quickly within 2–3 weeks; they are able to grow through any tissue, including bone. If the eye is not removed at this stage, it spreads to the brain and kills the patient.
Clinical manifestations of infection with mucor fungi are varied. Most often, this is rhinocerebral mucormycosis with damage to the maxillary, frontal and orbital sinuses of the skull, perforation of the palate and nasal septum, orbit, and paralysis of the facial muscles. Invasion of the fungus into the human body also leads to tissue necrosis, which visually appears as black lesions. In severe cases of systemic mucormycosis, disseminated necrotic lesions can affect almost all internal organs, with a mortality rate of 100%.
With pulmonary mucormycosis, progressive multiple appearance of infiltrates in the lungs, severe hyperthermia, bloody sputum, and progressive pneumonia are observed. Mortality in the pulmonary form is up to 65%. There are also lesions of the gastrointestinal tract (with the development of necrotic ulcers, intestinal perforation and peritonitis) and the skin (with ulcerations, deep abscesses, black necrotic lesions).
Is a person with mucormycosis dangerous to others?
No. Infection with mucor fungi (mucormycetes), like other molds, can occur through inhalation by inhaling spores or by eating foods affected by mucor mold, or in rare cases through damaged skin or mucous membranes. Moreover, the likelihood of developing the disease directly depends on the state of immunity.
A patient with mucormycosis, even with severe lesions, does not experience such rapid growth and maturation of the mycelium that fungal spores are released into the environment, so it cannot be said that he can become a source of infection for others, with the exception of some very casuistic cases.
It is no coincidence that the sharp increase in invasive mucormycosis this summer in India coincided with the growth and peak of the incidence of COVID-19 in this country. Several factors came together: weakened people with COVID-19 and after recovery, heat, a mild, humid climate in which mold fungi feel at ease, and the peculiarities of culture, living conditions and lifestyle in a given country.
Do you mean non-compliance with sanitary standards and rules?
About 8 years ago, long before the COVID-19 pandemic, I had to go on a business trip to India. With colleagues from the Center for Expertise and Testing in Healthcare and the Republican Center for Hygiene, Epidemiology and Public Health, we visited a medical equipment manufacturing plant in Hyderabad to inspect the production conditions on site, as well as see how this equipment is used in medical practice. Everything was great at the plant, as well as in the hotel where we stayed, but the rest of it gave me (and my diploma qualification is a medical hygienist-epidemiologist) a culture shock.
Crowds of people, motorized carriages and no traffic rules; in 30-degree heat, street vendors sell raw chicken meat from wooden trays, there is garbage along the roads, some people live in real shacks, cook and sleep on the street, sometimes just on the ground. In the center of the city there is a large lake of a poisonous green color, in which even local residents do not risk swimming. I really remember the monkeys that ran freely through the trees near our hotel.
The Institute of Medical Sciences located in the city also surprised with its contrasts. These include shabby walls and ceilings with crumbling plaster, an abundance of intertwined electrical wires, furniture and elevator equipment from the last century, and at the same time a lot of quite modern medical equipment. By the way, laboratory research there was carried out at a quite decent level. In general, Indians are very good-natured and sociable people, who gave us a warm welcome.
Mikhail Chernovetsky in the laboratory of the Institute of Medical Sciences in Hyderabad (India, 2012).
Are mucor mushrooms dangerous only for countries with hot, humid climates?
Under natural conditions, mucor micromycetes are widespread throughout the world; in most cases, they are saprophytic microorganisms found on dead plant cells, in soil, compost, and food debris. At the same time, in a number of countries, mucor mushrooms are used in local cuisine.
For example, in Southeast Asia, when preparing a dish from soybeans (tempeh), a special starter containing Rhizopus oligosporus or Rhizopus oryzae is used to ferment them and gives the product a special smell (nutty-mushroom) and taste. This “delicacy” is especially popular in Cambodia, Burma and other countries of Southeast Asia. Thus, the same mushroom can be used, on the one hand, to prepare a national dish, and on the other, cause severe invasive mycosis with disability and high mortality. It was Rhizopus oryzae that was most often detected in patients with systemic mucormycosis in India.
In total, over 867 varieties of mucor fungi (mucormycetes) have been described, among which Rhizopus oryzae (arrhizus) and Lichtheimia corymbifera are of greatest etiological importance.
Melon with colonies of Rhizopus orysae.
Are these dangerous types of molds found in Belarus?
I can only speak about the data from the laboratory of our center. I recently analyzed the etiological structure of fungaemia (detection of fungi in the blood) over a 19-year period. A total of 212 blood cultures of fungal microflora were registered. In the vast majority of cases (91%), of course, these were yeast fungi, mainly of the genus Candida.
During this time, there were 19 cultures of mold microflora from the blood, including in one patient it was Mucor spp. and one Rhizopus spp., the rest are predominantly Fusarium spp. and several Aspergillus. If we take bronchoalveolar lavage, biopsies of the bronchi and lungs, then the percentage is different: in approximately 60% of cases mold fungi (including Aspergillus and Mucormycetes) were sown, and in 40% yeast flora was sown. These data are now being refined and prepared for publication.
It is a clear fact that molds, including mucoraceae, are becoming an increasing problem for immunosuppressed patients around the world. At the 26th international online conference “Current issues in pediatric oncology, hematology and immunology” recently held in our center, our colleagues from Russia, the National Medical Research Center of Hematology, spoke about this. Interesting data was shared by specialists from the Moscow City Research and Production Center for the Fight against Tuberculosis: in patients with tuberculosis with damage to the lung tissue against the background of reduced immunity, mold flora, including mucor flora, began to be sown more often, although this is mainly due to the generic affiliation.
What does this mold look like in the environment? Is it only dangerous for people with weakened immune systems?
The name “black fungus” comes from the color of the clinical manifestations - black scabs on the skin and mucous membranes. In the environment, this mold, on the contrary, is white and looks like a kind of “fluff”. If you watch, after some time black dots begin to appear there. In our country, such mold can be seen on affected vegetables, for example, on tomatoes in greenhouses.
This could just be mucor mold, although white, gradually blackening mycelium is also characteristic of other types of mold. At the same time, some types of mucor fungi may have a different color of the colonies, for example, a bluish-greenish tint. For accurate diagnosis, it is necessary to grow this mold in the laboratory on special nutrient media and then study its micromorphological properties under a microscope.
A tomato affected by mucor mold.
Various types of molds, including Aspergillus spp., are often found in damp, cool rooms, on damp books and household items, fallen leaves of trees, and affect crops. In ordinary life, people often have to inhale Aspergillus spores, but the human immune system can cope with this quite well.
Of course, when working for many hours without a respirator with moldy grain in a granary or when washing fungal mycelium from walls without personal protective equipment during repair work, it is quite possible for aspergillosis to develop in a person with normal immunity, which manifests itself mainly in damage to the lungs. But for immunosuppressed individuals, including those in the ICU or those who have recently had severe COVID-19, inhalation of large quantities of Aspergillus spores always carries a greater risk of invasive mycosis, which can affect the lungs and other internal organs in a short period of time. You need to remember this.
Are there any clinical signs by which a doctor can quickly suspect the addition of a secondary fungal infection and the development of invasive mycosis?
When, during treatment of an infectious disease with the use of antibacterial therapy, the patient’s condition does not improve and a persistent fever persists, then you definitely need to think about the likelihood of fungal microflora joining. To exclude these suspicions, it is necessary to collect blood and culture it to isolate a fungal blood culture.
In our center, given the patient population, hyperthermia is immediately a reason to test for the presence of infectious agents in the blood, and the prescription of antibiotics is carried out strictly according to clinical protocols, taking into account antibacterial sensitivity. This principle also applies when prescribing antifungal therapy - using special tests, we determine the minimum inhibitory concentration of antifungals to the isolated fungal microflora.
For more information on how laboratory diagnostics of invasive mycoses is carried out using both traditional microbiological studies and additional biomarker, mass spectrometric and molecular genetic methods, see here.
Photo by Tatyana Stolyarova, “MV”, and from the archive of M. Chernovetsky.
Treatment of skin fungus
Mycoses are difficult to treat due to impaired cellular immunity. When treating them, old proven remedies and modern antifungal drugs are used, which are divided into drugs that stop the growth of fungi and drugs that kill them. Some of these drugs are obtained synthetically, others are natural. There are narrow- and broad-spectrum antifungal drugs. In addition, different forms of the disease have their own nuances of treatment, so only a doctor can choose the right treatment.
The basis of treatment for skin fungus is:
- The use of general and local antifungal drugs.
- Treatment of somatic pathology.
- Antifungal treatment of personal belongings and household items to prevent re-infection and adherence to personal hygiene rules.
Local treatment of skin fungus
Fungal infections (mycoses) are a very common disease. A doctor’s arsenal includes many medications, such as old, well-proven ones, as well as new drugs that are available in the form of ointments, creams, lotions, sprays, drops and powder. They are easily applied to the skin.
- When swelling, skin damage, oozing and secondary infection occur, antifungal drugs with corticosteroids and a broad-spectrum antibiotic (Triderm cream, Mikozolon, Lotriderm, etc.) are used. Triderm cream is available in the form of ointment and cream, which allows it to be used for different types of fungal damage and at different stages of the pathological process. The simultaneous use of Lamisil spray gives a good effect.
- When acute inflammatory phenomena subside, drugs are used that kill fungi or stop their growth and reproduction. The group of azoles for topical use is represented by Clotrimazole, Miconazole, Bifonazole, Econazole, Isocanazole, Ketoconazole, Metronidazole, Fluconazole, etc. The group of allylamine amines is represented by Naftifine and Terbinafine (Lamisil). A group of medications of various chemical groups is represented by preparations of undecinic acid (Undecine and Zincundan), quinosol, urea, acids (lactic, acetic, benzoic), Octicyl, Decamine, Anmarin, aniline dyes, etc.
Some information about Lamisil
- Lamisil is highly active against all types of fungi, including yeast and mold.
- Lamisil exhibits high activity in the treatment of complications of the disease and allergic rashes.
- The drug is available in the form of a spray, gel (Lamisil Dermgel), cream and film-forming solution (Lamisil Uno), which ensures maximum comfort of its use.
- The drug is used to prevent disease and treat shoes.
- Lamisil restores skin pH and skin hydration levels.
- Promotes epithelization of skin lesions with cracks.
- When using Lamisil Uno, the film covering the skin of the feet lasts up to 72 hours, ensuring that the drug reaches the stratum corneum of the skin for a long time.
- The clinical effectiveness of the drug reaches 72%.
Treatment of skin fungus with systemic antifungal drugs
Treatment of fungal infections with tablets and injections (systemic drugs) is used for moderate and severe disease. Taking them increases the chances of cure, but requires constant medical supervision due to a number of side effects.
For the treatment of fungal diseases, 2 groups of antimycotic tablet drugs are used:
- Group 1 of drugs (azoles) is represented by itraconazole (orungal), fluconazole, ketocornazole;
- Group 2 drugs (allylaminamines) are represented by terbinafine and naftifine. Itraconazole and terbinafine quickly penetrate the stratum corneum of the skin and remain there for a long time.
Selection of doses of antifungal drugs and determination of the duration of treatment is carried out only by a doctor
If the disease is combined with skin lesions in other parts of the body, the doctor will decide to prescribe more powerful antifungal drugs.
Pathogenetic therapy
Pathogenetic therapy drugs are prescribed for any pathology. With their help, the effectiveness of treatment increases and the likelihood of adverse reactions decreases.
In case of fungal infection it is necessary:
- correct immunological disorders,
- reduce allergic manifestations,
- make up for the lack of sulfur, which is found in eggs, cottage cheese, herbs, etc.,
- take vitamins of group A.
Timely initiation and correct selection of treatment for fungal infection will allow you to achieve a healthy appearance in the shortest possible time, eliminate the feeling of discomfort and improve your general condition.
Reasons for treatment failure
The main reason for the ineffectiveness of treatment for fungal diseases is the patient’s violation of the treatment regimen.
- More than a third of patients consider their disease not serious and refuse treatment.
- About 70% of patients do not believe that the prescribed treatment will bring a positive result.
- Half of the patients are not satisfied with the previous treatment.
- Up to 70% of patients stop treatment when a positive result is achieved and no longer come to see a doctor to monitor for cure.
Classification of mycoses
Mycoses are usually divided according to the degree of involvement of the skin, mucous membranes and appendages of the skin in the pathological process:
- Keratomycosis
. Fungal microorganisms multiply only in the stratum corneum of the skin; keratomycosis does not cause extensive inflammatory changes on the body. - Dermatophytes
. The changes affect the dermis and epidermis, as well as nails and hair follicles. - Candidiasis
. In addition to the skin, mucous membranes may be involved in the pathological process. - Deep mycoses
. Not only the skin is affected, but also a number of internal organs.