What is keratosis?
Let's start with the fact that cutaneous keratosis is a collective term that refers to a whole group of non-inflammatory diseases associated with impaired keratinization of the skin. Clinically, the process can manifest itself as slight peeling or the formation of thickened horny layers. There are follicular, seborrheic, and actinic keratoses.
Keratosis follicularis is characterized by the formation of horny plugs at the openings of hair follicles.
Seborrheic keratoses are plaque-like or nodular formations with a warty surface, covered with dry, horny masses that are flesh-colored, brown, or black in people over 50 years of age.
Actinic keratosis appears on exposed areas of the skin, initially appearing as bumpy, rough skin that eventually develops into rough, scaly patches ranging in color from normal skin tone to reddish brown. They are often limited in size and vary in size.
Prevention
There are no special methods for preventing keratosis pilaris. To reduce the risk of its occurrence, the following are relevant:
- relief of skin irritation;
- increasing the body's immune forces.
If you take precautions, treatment of keratosis if it occurs will be more successful.
The method of preventing actinic keratosis is to avoid exposure to direct sunlight. The risk of developing seborrheic keratosis can be reduced if you take proper care of your skin throughout your life - thanks to this, the aging process of the skin will occur later.
General recommendations for the development of any type of keratosis are to follow a healthy lifestyle and avoid prolonged exposure to UV rays on the skin.
On our website Dobrobut.com you can get more detailed information about how keratosis occurs, what it is, and how to treat it.
For what reasons do acquired keratoses occur?
The main cause of almost all keratoses is said to be chronic exposure to ultraviolet rays. In the literature, all changes associated with sun exposure are often grouped under the term dermatoheliosis. Thus, the damaging effect can affect the epidermis (senile, actinic keratosis), dermis (solar elastosis), blood vessels (telangiectasia), sebaceous glands (porokeratosis) and melanocytes (dyschromia).
The effects of sun damage to the skin gradually accumulate as the total amount of time spent exposed to UV rays increases year after year. This leads to the fact that the peak incidence of this nosology occurs at the age of 50 years and older.
However, nowadays, actinic keratosis has become much more common in young people. As a rule, these are people of the first and second phototypes (with fair skin, blond or red hair, and blue, green or gray eyes). There is a high likelihood of developing keratoses in young people exposed to sunlight for a long time.
The incidence is slightly higher in men because they tend to use little or no sun protection. Clinical studies estimate that about 60 percent of predisposed individuals by the age of forty have at least one element of actinic keratosis. Some experts believe that almost everyone over the age of 80 suffers from some form of keratoses.
In addition, persons whose immune defenses are weakened by chemotherapy, extensive exposure to x-rays or a number of industrial chemicals, patients with AIDS, patients who have undergone organ transplants, patients with disorders of the nervous and endocrine systems, etc. less able to combat the effects of radiation and, therefore, more prone to developing keratoses.
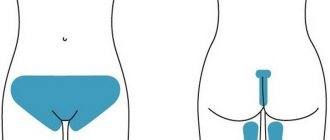
What are the symptoms of this disease? In what areas do they appear most often?
The patient, as a rule, may miss the onset of the disease and not pay attention to small irregularities, roughness, sometimes invisible to the eye, on the skin of the cheeks, bridge of the nose, ears, forearms, upper arms and forearms, back of the hands, back of the neck, upper chest, even on the scalp. Moreover, actinic keratosis can also develop on closed areas of the body that have been repeatedly exposed to the sun.
Developed actinic keratosis is represented by neoplasms from 0.1 cm to 2 cm or more. Over time, the spots become red or brownish in color and flake, and may rise above the skin in the form of growths. We most often see such patients at clinic appointments. Actinic keratosis usually develops very slowly and usually does not cause any discomfort other than aesthetic ones. Itching or burning in the affected area usually occurs in areas of long-term and severe keratinization. Most often, elements of skin keratosis develop slowly, but can disappear and reappear with repeated exposures that damage the skin. They can become inflamed and, in rare cases, even bleed.
Keratoma: how to treat?
To help the patient get rid of keratoma or actinic keratosis, the doctor prescribes a conservative or surgical treatment method. If drug therapy does not produce results, if the location of the formation is unsuccessful, if it is perceived as a cosmetic defect, surgery to remove the keratoma is prescribed.
Drug therapy
Drug treatment involves the use of various ointments, solutions or emulsions with active substances. It is immediately important to note that such methods are effective in the initial stages, when the stain has just appeared. Therapy must be prescribed by a doctor. Self-medication is strictly not recommended, as it can cause complications in the form of damage to surrounding healthy tissue.
Keratoma: how to remove surgically?
The keratoma is surgically removed using one of the following methods:
- laser method;
- cryodestruction;
- radiosurgery method.
The leader of choice is laser removal, since it minimizes the risks of negative consequences, bleeding, wound infection, and relapses. In a few minutes the formation is completely removed. And the wound heals within a few days.
Possible risks
Attempts to remove the keratoma yourself by tying it with thread or cauterizing it with aggressive media are strictly prohibited. This can lead to serious consequences, including the degeneration of a benign tumor into cancer.
Are there any new developments in this direction on the world market?
Well, for example, from 1998 to the present, the Australian biopharmaceutical company Peplin has been studying the topical treatment of actinic keratosis with the drug Ingenol Mebutate, which is the first in a new class of formulations and is derived from milkweed juice. This ingredient has a long history of traditional use for a variety of skin conditions, including the topical treatment of skin cancer and precancerous skin lesions. The company plans to enter the third phase of the trial soon.
What are destructive (ablative) methods?
All skin tumors must be examined by a dermatologist before removal due to the risk of skin cancer. Treatment performed in a timely manner will help prevent the development of basal cell carcinoma (BCC) or squamous cell carcinoma of the skin (SCC).
- Cryosurgery using liquid nitrogen is the most common method for treating keratoses, but is not suitable for hyperkeratotic lesions. Liquid nitrogen is sprayed directly onto the affected areas of the skin using a cryodestructor or applied using the “reed” method (application with a cotton swab on a wooden stick). Cryosurgery is easily performed on an outpatient basis, shows excellent cosmetic results and is well tolerated.
- Radio wave, electro- and diathermo-laser destruction.
- Photodynamic therapy involves the application of a photosensitizing agent, methyl aminolevulinate, and then exposure to light of a specific wavelength, which leads to tissue necrosis. Photodynamic therapy is well tolerated and has excellent cosmetic results.
- Surgical removal . The surface of the skin is cleaned with a special instrument (curette).
- Chemical peeling:
- Jessner's solution (resorcinol, lactic and salicylic acids in ethanol);
- trichloroacetic acid solution 35%.
- Dermabrasion . The affected areas of skin are removed using a fast-moving abrasive brush.
- Phototherapy (IPL) and fractional photothermolysis - coagulation of keratosis elements using light energy. Suitable for the initial manifestations of actinic keratosis.
Moderate actinic keratosis (AK) is a common photo-induced skin lesion that can progress to invasive squamous cell carcinoma and serve as a risk marker for skin cancer. Although numerous studies have published various therapeutic options for AK, only a few of them can be used by dermatologists in their daily practice. National and international guidelines have been published, however, these are based on clinical trials of heterogeneous patient groups and do not always reflect the spectrum of patients seen in daily practice. Introduction
The aim of this work by French dermatological experts was to present an analysis of AK adapted to daily practice, to provide an informed opinion on the latest procedures and to propose an algorithm for the treatment of AK for daily practice in France. Over a 12-month period, 6 expert dermatologists in the field of AK met regularly to formulate opinions on treatment in daily practice, taking into account a review of the literature and guidelines published since 1990. Definitions, terminology, diagnosis, and risk factors have been summarized. Evidence from the literature and practice related to initial assessment, indications for biopsy, indications for use, treatment options and effectiveness, monitoring and prevention were discussed. A pragmatic treatment algorithm was designed according to current data. This practical algorithm distinguishes different clinical situations depending on the number of AK lesions, severity of hyperkeratosis or suspicious nature, and includes cryotherapy, curettage-electrocoagulation, 5% 5-fluorouracil, 3% diclofenac sodium, 5% imiquimod, 150 and 500 mcg/ d ingenol mebutate, lasers, photodynamic therapy and surgery. These modern expert opinions on AK and its treatment provide a strategy and practical algorithm for the treatment of AK for French dermatologists.
Introduction
Moderate actinic keratosis (AK), also called solar keratosis, is a photo-induced chronic skin lesion that is often seen in adults. AK repeatedly occurs in sun-damaged areas and is one of the clinical signs of skin photoaging. This photoaging is most often characterized by mild actinic lentigo (sun spots) or wrinkles that precede the appearance of AK. Histologically, AK reveals atypical areas of proliferation and differentiation of keratinocytes. They are prone to develop into invasive cutaneous squamous cell carcinoma (SCC). Their presence is also considered a risk marker for skin cancer.
Moderately severe AK is common, with a predominance of 15.4% and 34% of men and 5.9% and 18.2% of women at 40 and 70 years of age, respectively. In the Southern Hemisphere, the prevalence can reach 40-60% in older people with a fair skin phototype. This prevalence increases sharply with age, especially in predisposed populations with light skin phototypes, and due to the accumulation of sun exposure over the course of a lifetime. The prevalence of AK in France is unknown, but its incidence is estimated at 5% of patients in dermatological practice. Treatment of AK, due to the aging population and the risk of transformation of AK to SCC, may become a public health concern over time.
The purpose of this report is to provide a practical algorithm for the treatment of AK, taking into account the most recent therapeutic approaches.
Methods
6 experts, all physicians and dermatologists with significant experience in dermato-oncology, dermatological surgery or dermatopathology, met to form an expert panel. The jury members were from different French regions (West, South-West, South-East, East, Ile-de-France), and from any hospital, university clinics and/or private practice. All participants are well known in the AK field.
Over the course of several meetings, these specialists worked on the format and writing of this report, mainly based on their own practice and guidelines, including, but not limited to: recommendations of the French Society of Dermatology 2009 and European recommendations 2011.
Topics discussed were based on definitions and terminology, diagnosis of risk factors associated with AK, initial evaluation, indications for biopsy, therapeutic, clinical outcomes and recurrence. A practical therapeutic algorithm was developed based on this information, as well as practical experience and a clinical panel. Proposals were approved only if there was consensus among experts or if the opinion was accepted by a majority vote. A meeting in 2011 and four subsequent meetings in 2012 resulted in the expert opinions presented below.
Results and discussion: expert opinions on the management of moderate AK
Moderate actinic keratosis (AK) is a precancerous skin lesion that rarely occurs as a single lesion but most often occurs as multiple lesions. This chronic condition is also considered a risk marker for cutaneous malignancies. SCC may develop initially or after progression of precursor lesions such as AK. This report examines only SCCs arising from AKs, which are epidemiologically and biologically distinct from SCCs arising from burns, chronic ulcers, or chronic skin infections. A theory has been put forward according to which AK is already considered an in situ SCC. Expert opinion considers AK to be a form of in situ cancer that does not require management like invasive SCC. Indeed, although the histological appearance and molecular biology-based evidence of AK indicate that it is an intraepidermal carcinoma, evolutionary clinical data indicate that the risk of transformation into invasive SCC of any AK is low. Moderately severe actinic keratosis can develop in the following three main directions: 1) spontaneous disappearance, 2) persistent course without progression and transition to invasive SCC, 3) progression to invasive SCC. The rate of spontaneous regression of AK, according to estimates in the literature, is defined as a regression of rashes over a 1-year period by 15-25%. Some authors have therefore highlighted the potential importance of spontaneous resolution and appearance of new lesions in AK. The incidence of invasive SCC in patients with AK is estimated in the literature as 5-20% over the next 10-25 years. The conversion rate of AK to SCC is much lower, in the range of 0.1% - 0.24% over 1 year. Surprisingly, 82.4–100% of patients with invasive open-site SCC had a history of AK. There are no clinical, histological or biological criteria that can reliably predict the transformation of AK to SCC. However, some AKs are clinically more suspicious than others. Malignancy is defined as an area of subclinical changes at the periphery of visible AK lesions that can be detected histologically or using molecular biology or imaging techniques (reflectance, confocal microscopy). Clinically, this risk of malignancy is defined as an anatomical region exposed to chronic insolation, in which there are multiple and/or recurrent elements of AK. In this risk area, other histological and clinical signs of photoaging (solar elastosis, wrinkles, spots, lentigines, telangiectasia) are often present. The most commonly affected areas of the skin are the forehead, temples, nose, scalp, ears, décolleté, back of the hands and forearms. The experts agreed with these definitions.
Diagnosis of moderate actinic keratosis
The diagnosis of AK is essentially clinical. Most often it occurs in people with a light skin phototype, in open areas exposed to the sun (face, back of the hands and scalp). Signs of helioderma are often associated with AK (wrinkles, freckles, spots). Visually, AK lesions are horny, of variable thickness, 1 cm or less in diameter, with varying degrees of erythema, and sometimes pigmented. They may also have a configuration that resembles a cutaneous horn. The rashes have horny layers and are rough to the touch.
Clinically, the differential diagnosis of AK mainly includes seborrheic keratosis, actinic lentigo (sun spots), flat warts, melanocytic lentigo, but also occasionally SCC, Bowen's disease, basal cell carcinoma, melanocytic nevus or melanoma. When examining patients with AK, a dermatologist should first look for other AKs or even skin cancer that may already be present. It is important to educate other health care providers who may evaluate patients with AK (eg, rheumatologists, internists, geriatricians, occupational physicians) about the risks of AK and encourage them to refer patients to a dermatologist for regular evaluation.
Risk factors for moderate actinic keratosis
- Organ transplantation
- Long-term immunosuppressive treatment (chemotherapy and biotherapy)
- Skin exposure to carcinogens
- Excessive sun exposure or phototherapy
- Light skin phototype (I/II), especially in the presence of other risk factors
- History of cutaneous squamous cell carcinoma
- Some hemopathy
Initial assessment and indications for biopsy.
The initial assessment is clinical. This should include, at a minimum, examination of exposed skin and a search for other lesions. The doctor should also evaluate the patient's phototype and the presence of markers of chronic sun exposure (wrinkles, spots). In typical cases, the need for a biopsy for histological confirmation of the diagnosis of AK, as a rule, does not arise. However, a biopsy to exclude or confirm invasive cancer may be performed in cases where the skin is thickened, the lesion is >1 cm in size, the lesion is induration, inflammation, ulceration, bleeding, there is rapid growth or tenderness on palpation, in cases of rapid recurrence ( 2-3 months) or persistence of the treated lesion after standard therapy; in cases where the lesions are located in the risk zone (lips, back of the hand, ear).
Treatment: who should be treated and when?
Systematic treatment of all AKs to reduce the risk of skin cancer in general is not indicated. However, treatment may be justified depending on the clinical characteristics of the AK, as well as the history of skin cancer, the patient's wishes, and the impact of the lesions on quality of life. If desired, regular monitoring of the patient should be undertaken to detect SCC as early as possible.
Physical Treatment Options
Cryotherapy
This approach destroys tissue at low temperatures. Freezing and thawing of cells causes tissue necrosis. Cryotherapy is a simple, fast and inexpensive method. There is no standard protocol for cryotherapy—length of exposure, number of cycles, or frequency of treatment. The approach is highly operator dependent. This method is most often used for the treatment of isolated AKs in France. This is the current "gold standard" for the treatment of AK.
Efficacy: Complete cure with cryotherapy within 3 months is observed in 68-75% of patients, and with therapy for 6 months - 82.5-88%. The main adverse effects were pain during and immediately after treatment. There is also a risk of hyper- or hypopigmented scars.
Expert opinion: Cryotherapy is indicated as the first line of standard treatment for isolated or small numbers of AKs.
Surgical procedures
Surgical excision of the lesion is considered the standard of care for suspicious isolated AKs that may progress to invasive SCC. Surgical excision of the entire skin area (head, back, arms) is rarely used, performed in special cases of multiple AK, resistant to local treatment and in the presence of several suspicious sites of transition to SCC.
Expert opinion: resection is indicated for the presence of suspicious isolated AKs.
Curettage and electrocoagulation
Mechanical curettage of AC using curettage followed by electrocoagulation has been described in the literature and may be an alternative to cryotherapy for first-line treatment. The procedure is quick and provides hemostasis, incl. in patients receiving anticoagulants. This treatment is described in the English and Italian guidelines for AK. This technique is rarely used in France. No data on its effectiveness have been published.
Expert opinion: Curettage and electrocoagulation may be an alternative for AK treatment. The method is indicated for isolated or in small quantities and hyperkeratotic, but not suspicious and clearly defined AKs.
Laser therapy
Ablation lasers Er:Yag and CO2 lasers are indicated for isolated or multiple AKs. The thermal effect, evaporation of tissue with loss of substance and coagulative necrosis of the edges lead to the healing stage. Side effects include erythema, pain, irritation, itching, swelling, and sometimes secondary infection.
Expert opinion: Er:Yag and CO2 lasers are indicated for single AC. However, there are no randomized studies objectively comparing these procedures with other lasers and other treatments.
Photodynamic therapy (PDT)
PTD is based on the use of a topical photosensitizer, which, after illumination using appropriate light, promotes the selective destruction of tumor cells. Another interest of PDT is its action within the field of carcinogenesis. Most studies use a heme precursor, such as methyl aminolevulinate or aminolevulenic acid, as a photosensitizer. PDT allows lesions to be removed in one session. The effect should be assessed after 3 months. If necessary, repeat the procedure. Most studies used 2 sessions 1 week apart.
Efficiency: The effectiveness of PDT after two sessions after 3 months is 59% - 91%. The recurrence rate of lesions at 12-month follow-up was 17%. The best results were obtained in studies using two PDT sessions. Adverse Effects: A total of 60-80% of patients showed transient local reactions after treatment with burning sensation, skin pain, crusting and erythema. PDT is an effective but painful technique. Three recent randomized controlled trials have shown the effectiveness of daylight PDT for the treatment of AK. This method appears to be simpler and better tolerated than conventional PDT.
Expert opinion: PDT is indicated for thin/non-hyperkeratotic few AKs of the face and scalp. It can also be used in other places. Pain is the main limiting factor for this treatment method.
Topical treatments
Dermocosmetics
Emollients improve patient comfort by reducing dryness and roughness of the skin. They contribute only to partial improvement in 44% of patients. Topical keratolytics containing urea or salicylic acid are indicated for hyperkeratolytic forms of AK and promote exfoliation of the superficial layers of the epidermis by cleaving corneodesmosomes.
DNA repair using the enzyme photolyase
Photolyase is a photoreactive DNA repair enzyme that specifically converts pyrimidine dimers back to their original monomeric form. In order to induce DNA repair in the skin epidermis, photolyase activation requires exposure to light with a wavelength of 300-500 nm. In the manuscript, Stege et al. show that after exposure to UV radiation, the application of topical photolyase caused subsequent photoreactivation with a decrease in the number of dimers and prevented radiation immunosuppression and erythema formation.
5-fluorouracil
5-fluorouracil (5-FU) is an antimetabolite of a cytotoxic agent belonging to the antipyrimidine group. It interferes with DNA synthesis and, to a lesser extent, inhibits RNA transcription. In France, 5% 5-FU cream has been used to treat AK since the 1960s. 0.5% 5-FU cream is not available in France. It is most often used 1-2 times a day for an average of 3-4 weeks. An occlusive dressing can be used for better penetration. The treated surface should not be larger than 500 cm2 per treatment.
Efficacy: After 3-4 weeks, the effect was observed in 43% - 96%. In 65% of patients, the lesions recurred 12 months after treatment.
Side effects: Pain, itching, burning sensation and hyperpigmentation may occur at the site of application. An erythematous inflammatory reaction may require temporary discontinuation of treatment.
Expert Opinion: 5-Fu can be used to treat multiple lesions of AK over large areas.
5-fluorouracil+salicylic acid
This combination therapy is not used in France.
Imiquimod
Imiquimod is an imidazoquinoline derivative whose main mechanism of action is activation of the innate immune system. In France, imiquimod is indicated in immunocompetent patients and should be used with caution in patients taking immunosuppressive drugs. It induces activation of Toll-like receptors 7 and stimulates the synthesis and release of cytokines (eg, interferon-alpha, IL-12). It has an indirect antitumor effect and is used to treat AK by stimulating cutaneous innate immunity. It is used in the form of a 5% cream of 250 mg in sachets for a single treatment of 25 cm2 of the affected surface. The maximum recommended dose is one sachet per use for a maximum of 8 weeks. The treatment regimen for AK consists of one cycle of three treatments per week for 4 weeks, with assessment 4 weeks after cessation of treatment. The cycle can be repeated later. In Europe, imiquimod 3.75% cream received approval in August 2012. This latter form is not sold in France and therefore cannot be evaluated in practice by specialists.
Efficacy: With the regimen used in France, the effectiveness is 26.8% or 55% after one or two cycles, respectively. Relapse within 1 year after treatment is recorded in 17.4-39% of treated areas.
Side effects: Local reactions such as itching, burning, erythema, pain, swelling, dryness, crusting, erosions and ulcers may occur. Systemic reactions (myalgia, fatigue, nausea) are less common. During the second treatment cycle, reactions occur to a lesser extent.
Expert opinion: Imiquimod 5% is recommended for the treatment of smoking hyperkeratotic AK and few AK on the face or scalp. Experts also recommend it for use in other places, although these have not been evaluated. It should be used with caution in cases where immunosuppressive therapy is ongoing, especially in organ transplant patients.
3% diclofenac, 2.5% hyaluronic acid
Diclofenac 3% gel is a non-steroidal anti-inflammatory drug that is used to treat AK in combination with hyaluronic acid. It inhibits the cyclooxygenase pathway, which leads to decreased synthesis of prostaglandin E2 (PGE2). The recommended dose is 2 times a day for 8-12 weeks (60-90 days). The maximum dose is 8 g of gel per day.
Efficacy: the maximum therapeutic effect is observed 30 days after cessation of treatment. Complete cure occurred in 31% and 47% after 2 and 3 months of follow-up, respectively. The 1-year relapse rate is 21% (recurrence of lesions that have disappeared).
Side effects: Local reactions such as contact eczema, xerosis, swelling, itching, scaly rashes, ulcerations and vesiculobullous rash are common.
Expert opinion: Diclofenac gel is well tolerated but appears to be less effective than 5-Fu or imiquimod. It is recommended for use in non-hyperkeratotic and superficial AK.
Ingenol mebutate
Ingenol mebutate is a biological compound (Euphorbia peplus). The mechanism of its action in AK is not entirely clear. In vitro and in vivo, it showed a dual mechanism: direct cytotoxicity with the occurrence of mitochondrial swelling and dissolution of the cytoplasmic membrane; and delayed immunomodulation of innate immunity through the production of anti-inflammatory cytokines (IL-8 and TNF-alpha) and activation of neutrophils. Ingenol mebutate gel 150 mcg/g is used on the face and scalp, and is applied once a day for 3 days in a row; 500 mcg/g gel is used on the trunk and extremities and is applied once a day for 2 consecutive days.
Efficacy: In a study involving the face and scalp and another involving the trunk and extremities, complete clearance was observed after 2 months of treatment in 42% and 34% of patients, respectively. 12 months after treatment, relapses were noted in 54% on the face and scalp and in 56% on the trunk and limbs.
Side effects: erythema, spreading lesions, crusts, edema, vesicles/pustules, erosions/ulcers. Local skin reactions resolved within 2-4 weeks, depending on the location.
Expert opinion: Ingenol mebutate is the first topical drug with a short course of treatment. It is indicated for the treatment of multiple hyperkeratotic AKs located over an area of 25 cm2 on the face and scalp, as well as on the trunk and extremities.
Treatment algorithm
The treatment algorithm was determined by experts who took into account both literature data and their own clinical experience. This algorithm took into account: the number of lesions, their hyperkeratotic nature and the absence of suspicious clinical external signs of malignancy. Physical modalities (cryotherapy or curettage and electrocoagulation) are indicated as first-line treatment for isolated or few AKs, and surgery or laser therapy is suggested as second-line treatment in cases of recurrence or treatment resistance. Any suspicious AKs should be biopsied or excised. First-line topical treatments for low-abundance AKs are 5% 5-fu, 3% diclofenac, 5% imiquimod, and 150 mcg/g (face and scalp) or 500 mcg/g (trunk and extremities) ingenol mebutate. The choice of treatment will depend on factors such as the patient's compliance with treatment, quality of life, other diseases and procedures associated and adverse events that may occur. Physical procedures are more indicated for elderly and lonely patients, for whom the use of topical agents may be difficult. Treatment of patients with AK is often long-term, because AK is a chronic disease and may require the use of sequential procedures or combination approaches. However, to date, the literature does not support a specific order of sequential therapy and no interest in maintenance therapy.
Local inflammatory reactions: what should be done on a practical level?
An inflammatory skin reaction can be provoked by some topical medications and may lead to early termination of the procedure. Patients with inflammatory reactions are advised to use a gentle gel cleanser that is compatible with the pH of the skin. To relieve pain, inflammation and/or swelling, thermal water sprays are used. For erosive lesions or crusts, dermocosmetics are prescribed 2 times a day. Emollients for dry skin. In case of a strong inflammatory reaction, a break in treatment is recommended. Corticosteroid drugs should be avoided because their anti-inflammatory effects may interfere with the local inflammatory responses required for the agent to be effective. It is necessary to use photoprotective agents on the treated areas, especially in spring and summer, to avoid photosensitivity and the risk of post-inflammatory pigmentation. Sometimes it is better to delay treatment for AK until the fall or winter.
Specific situation: organ transplant patients
Organ transplant patients are at increased risk of developing skin cancer. In these patients, the incidence of AK is extremely high, and the incidence of SCC is almost 100 times higher than in the general population in individuals of the same age and phototype. Risk is a variable that depends on the degree of immunosuppression, its duration, and the type of organ transplanted (higher risk for heart transplant patients than for kidney transplant patients). Current data suggest that AK in these patients will progress at a faster rate with more frequent transformation to SCC. However, the more frequent occurrence of SCC in such patients described in the literature is currently questioned. These patients require more careful monitoring and a stricter approach to treatment. Treatment of AK should be carried out, if possible, before organ transplantation.
Monitoring and secondary prevention
Patients with AK should be monitored regularly due to the chronic nature of the lesions and the risk of invasive SCC. Patients should be consulted annually. During these consultations, patients should be made aware of the need for an emergency consultation if any lesion changes very quickly, or in the event of recurrence after treatment. Patients with organ transplantation must be monitored in a special way, especially in the context of personalized monitoring. Sun-protective clothing and behavior, and the use of sunscreens (chemical or mineral filters), should be recommended for patients to minimize worsening of photo-induced skin damage and to prevent skin cancer. Sunscreen has been shown to be an effective method of preventing AK. Sunscreen use (more than SPF-15 applied every 2-3 hours) reduces the risk of AK lesions by up to 24% over time, even compared with beta-carotene and topical tretinoin 0.05% cream. AAD (American Dermatological Association) guidelines state that when choosing a sunscreen, choose a broad-spectrum (UVB/UVA) cream and that daily use of an SPF-30 product is recommended on all exposed skin.
conclusions
The purpose of this expert panel was to provide practical solutions for dermatologists in terms of a diagnostic, monitoring and treatment algorithm that they can use in their daily practice, based on the scientific literature and current recommendations.