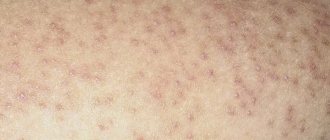
A plantar wart is a benign growth on the skin of the feet that can form on one side or affect both feet at the same time. The development of warts is provoked by infection and activation of the human papillomavirus in the body. Treatment is complex and requires correction of external defects and strengthening of the immune system to prevent recurrence of epithelial growths.
What is the ICD-10 code for a plantar wart?
A wart on the foot is a reason to consult a dermatologist, podiatrist, or cosmetologist to eliminate discomfort and pain when walking.
First, the doctor conducts a thorough diagnosis to determine the type of formation, the level of oncogenicity of the specific HPV strain that caused the appearance of this type of growth. The specialist excludes signs of malignant degeneration.
According to the International Classification of Diseases ICD-10, pathological papillomavirus formations on the feet have code B07.
Localization on the feet (feet, toes, damage to the periungual fold, the nail itself, interdigital space) often leads to damage to warts, the development of clinical manifestations (pain, inflammation, bleeding), symptoms quickly progress due to the constant pressure of weight on the soles, aggravation of the condition of the growths.
Types and causes of appearance
The main etiological factor in the development of warts on the foot and sole is HPV infection from a carrier of the virus.
Routes of infection:
- transmission through microcracks in the legs, wounds, abrasions when visiting public bathing places: swimming pools, beaches, showers in sports clubs;
- use of public household items, lack of individual shoes, hygiene products; towels, razors, underwear, bed linen;
- with direct skin-to-skin contact;
- self-infection in the absence of personal hygiene: dirty hands, scratching wounds.
The virus can remain in a latent phase for a long time.
There are predisposing factors for increased growth of warts on the soles:
- weakened immunity due to long-term viral and cold diseases;
- autoimmune pathology;
- hormonal disruptions in the body (pregnancy, lactation, menopause, puberty, treatment with corticosteroids, disruption of the thyroid gland);
- exposure to aggressive detergents on the skin of the feet;
- varicose veins, atherosclerotic vascular lesions, diabetic foot, microcirculation disorders in the lower extremities;
- exposure to uncomfortable shoes provokes foot deformation, increased sweating or dry skin, maceration is a favorable environment for the appearance of warts on the soles;
- frequent stressful situations, depression;
- metabolic disorders, unbalanced nutrition;
- presence of harmful habits: alcohol abuse, smoking, drug addiction.
There are several types of papillomavirus growths on the sole:
- single forms, multiple formations;
- mosaic, homogeneous structure;
- the structure can be flat, convex;
- in color - from pale pink to dark brown. A wart may turn black when its roots grow into vascular formations;
- the internal root can be localized in the thickness of the epidermis or grow into the dermis, which complicates the removal process.
Etiology of warts vulgaris
The human papillomavirus (HPV) is present in the blood of 90% of the population of our planet, but not all carriers notice the appearance of skin warts . This is due to the peculiarity of the viral agent, which can remain in an inactive form for a long time, while maintaining vital activity. Activation of HPV is caused by a decrease in the immune response, which occurs against the background of a deterioration in the general condition of the body. Frequent accompanying conditions for the formation of vulgar warts are the following factors:
- Hormonal disorders;
- Exacerbation of chronic diseases;
- Infectious or inflammatory process;
- Neuro-emotional and physical fatigue;
- Stress;
- Hypovitaminosis or vitamin deficiency.
It has been noted that quite often the formation of a primary (maternal) wart occurs at the age of 7-14 years. This is due to the high probability of the child becoming infected with the papilloma virus. Infection can occur both through contact with a carrier and through the use of common household items and toys. For children, the typical route of penetration of the viral agent is through the damaged surface of the skin: scratches, abrasions, wounds.
A characteristic feature of epidermal warts is their ability to autoinoculate, which manifests itself in the spread of a cosmetic defect to healthy tissue areas. For vulgar warts, this can manifest itself in the formation of paired or “kissing” growths, which look like symmetrical growths, most often separated by a skin fold. Quite often, the back of the hand is subject to multiple rashes.
Are plantar warts contagious?
Need advice from an experienced doctor?
Get a doctor's consultation online. Ask your question right now.
Ask a free question
The danger of plantar elements is that they are easy to injure, causing the growth of multiple elements with damage to the skin of the feet, legs, and other parts of the body. Virtually all types of warts are contagious, and plantar warts are no exception. Cases of self-infection and relapse of the disease, even after a course of therapy, are often diagnosed by doctors if there are several growths on the patient’s body. To prevent transmission of the virus and reinfection, it is worth conducting a thorough diagnosis (tests for HPV, histology of biopsy specimens), and comprehensively treating the body, and not just external manifestations.
Viral warts are a fairly common pathology of the skin and mucous membranes in both children and adults. According to the observations of a number of authors, clinical manifestations of human papillomavirus infection of the skin are observed in 3-9% of children and adolescents and in 28-30% of adults. There is no significant correlation between the incidence of this pathology and race or gender. About 38-42% of people carry HPV on apparently healthy skin.
The causative agent of the disease is the human papillomavirus (HPV), which belongs to the DNA-containing viruses of the papavavirus family (Papavaviridae). Currently, about 200 HPV genotypes that infect humans, mammals and birds have been identified and characterized; of these, the genera whose representatives infect humans are include alpha-, beta-, gamma-, mu- and nupa-pillomavirus. The most common causes of viral warts are HPV types 2,27 and 57 (alpha-papillomavirus), type 4 (gamma-papillomavirus) and type 1 (mu-papillomavirus). HPV types 3,7,10 and 28 (alpha-papillomavirus) are less common. papillomavirus), HPV types 65,88 and 95 (gamma-papillomavirus) and HPV type 41 (nupa-pillomavirus).
Human papillomaviruses have tissue specificity - the ability of certain types of HPV to infect tissue characteristic of their localization:
- HPV types 1,2 and 4 are detected with plantar warts;
- HPV types 2,4,26,27,29,57 - for vulgar warts;
- HPV types 3,10,28,49 - for flat warts;
- HPV type 2.7 – for “butcher’s warts”;
- HPV types 13 and 32 - with focal epithelial hyperplasia;
- HPV types 5,8,9,10,12,15,19,36 - with verruciform epidermodysplasia;
- HPV type 60 - for cystic warts.
Transmission of the virus can occur through household contact, through auto- or heteroinoculation at sites of damage to epithelial tissue. The risk of HPV infection depends on a number of factors, such as the localization of lesions, quantitative indicators of HPV (viral load), the degree and nature of contact, the state of general and local immune status. Infection is facilitated by the presence of microtraumas and inflammatory processes of the skin. It should be taken into account that HPVs are present not only in the cells of the basal layer of lesions, but also in clinically intact nearby areas of the skin and mucous membranes, where the virus can persist in a latent or inactive state, and the infection is activated can lead to relapse of the disease even several years after treatment. In the presence of favorable factors, the process of replication of human papilloma viruses in the epithelium begins, which leads to impaired cell differentiation and the formation of morphologically altered tissues.
What is the difference between a plantar wart and a corn with a stem?
When examining a formation on the foot, a specialist doctor makes a differential diagnosis of a growth of viral origin, a callus with a core.
When determining the difference between a plantar wart and a corns with the core of the lower extremities, it is necessary to focus on comparative characteristics:
| Name of education | Wart on the sole | Dry callus (corns) |
| Reason for appearance | Viral infection – HPV. | Trauma with the development of tissue necrosis. |
| Circulation | It grows through capillaries and can become red or, if deeply localized, black. | Absent, bleeding is excluded in case of injury or puncture. |
| Form | Nodular, regular shape with clear boundaries, always rises above the surface of the skin. | May have unclear boundaries. |
| Soreness | Pain when walking or pressing on the sole. | There is often no pain, even when removal is attempted. As the rod grows, pain and burning appear. |
| Color | From pale pink to dark brown. | Light yellow or beige. |
A wart is a dangerous form of pathology and requires treatment from a doctor. Corns can heal on their own when the stem is removed.
Viral wart in a child
Principles of treatment
In pediatric dermatology, there is a rule: viral warts that do not bother the child and do not have a risk of malignancy require only active observation.
Such formations can spontaneously regress within two years. It is imperative to treat warts in patients with immunodeficiency conditions to avoid self-infection. Therapy is also indicated if the wart causes itching, pain, creates psychological discomfort, or bleeds. The main method of treating a viral wart in a child remains removal by destruction. An immunologist may prescribe antiviral therapy with interferon drugs.
Physical destruction
For children, this type of therapy is a priority, as it has no toxic side effects. The choice of method depends on the location of the wart, its type, and size. Any of the techniques is performed against the background of local anesthesia (anesthetic cream or infiltrative anesthesia with lidocaine solution):
- Cryodestruction.
The essence of the method is the effect of liquid nitrogen on the proliferation zone. A contact cryoprobe with special attachments is used. Exposure time is up to five minutes. Repeated procedures are carried out if necessary after 1–2 weeks. - Electrocoagulation.
The destruction of a viral wart occurs as a result of the action of a low power electric current. The coagulator provokes layer-by-layer thermal damage to pathological tissue. The technique is bloodless, allowing you to work as accurately as possible in the hearth. - Radiocoagulation.
With this type of destruction, electromagnetic waves are used. Under the influence of radio waves, intercellular connections are broken, the pathological tissue is stratified and destroyed. - Laser destruction.
Wart removal occurs through laser ablation. Depending on the size of the formation, exposure to the beam lasts up to 2-3 minutes. If there is a need for repetition, the next manipulation is carried out after 1 month.
Chemical destruction
The basis of the technique is the application of local agents with a keratolytic effect for the purpose of cytolysis of pathological tissues. Several acids are approved for use in children: salicylic 15-40%, oxalic, acetic, lactic, nitric in various combinations. The treatment regimen depends on the course of the disease. The drug of choice for the treatment of flat warts is creams based on trans-retinoic acid (a form of vitamin A). The course of use is long - up to three months.
Surgery
Surgical intervention is justified if there is a risk of atypical transformation of a viral wart in a child, with a large area of damage. Methods of surgical correction:
- Blunt excision
. To remove the formation, non-sharp surgical instruments are used - specially designed scissors. The method is considered the most effective in children. Has the smallest number of relapses – about 10%. - Curettage.
It involves peeling off a wart with a surgical curette. Efficiency is enhanced by parallel cryodestruction. Curettage is used for medium-sized viral warts. - Excision.
Full surgical treatment with removal of the wart with a scalpel within healthy tissue. The method is traumatic, so it is used when absolutely necessary. Excision is indicated for deep damage to the dermis.