Atopic dermatitis is a chronic, non-contagious inflammatory skin lesion that occurs with periods of exacerbations and remissions. It manifests itself as dryness, increased skin irritation and severe itching. It causes physical and psychological discomfort, reduces the patient’s quality of life at home, family and work, and externally presents cosmetic defects. Continuous scratching of the skin leads to secondary infection. Diagnosis of atopic dermatitis is carried out by an allergist and dermatologist. Treatment is based on diet, general and local drug therapy, specific hyposensitization and physiotherapy.
General information
Atopic dermatitis is the most common dermatosis (skin disease), developing in early childhood and maintaining certain manifestations throughout life. Currently, the term “atopic dermatitis” refers to a hereditary, non-contagious, allergic skin disease of chronic relapsing course. The disease is the subject of supervision of specialists in the field of outpatient dermatology and allergology.
Synonyms for atopic dermatitis, also found in the literature, are the concepts of “atopic” or “constitutional eczema”, “exudative-catarrhal diathesis”, “neurodermatitis”, etc. The concept of “atopy”, first proposed by American researchers A. Coca and R. Cooke in 1923, implies a hereditary tendency to allergic manifestations in response to a particular irritant. In 1933, Wiese and Sulzberg coined the term “atopic dermatitis,” which is now generally accepted, to refer to hereditary allergic skin reactions.
Atopic dermatitis
Causes
The hereditary nature of atopic dermatitis determines the widespread prevalence of the disease among related family members. The presence of atopic hypersensitivity (allergic rhinitis, dermatitis, bronchial asthma, etc.) in parents or immediate relatives determines the likelihood of atopic dermatitis in children in 50% of cases. A history of atopic dermatitis in both parents increases the risk of transmitting the disease to the child by up to 80%. The vast majority of initial manifestations of atopic dermatitis occur in the first five years of life (90%) of children, of which 60% occur during infancy.
As the child continues to grow and develop, the symptoms of the disease may not bother or weaken, however, most people live with a diagnosis of atopic dermatitis all their lives. Atopic dermatitis is often accompanied by the development of bronchial asthma or allergies.
The widespread spread of the disease throughout the world is associated with problems common to most people: unfavorable environmental and climatic factors, dietary errors, neuropsychic overload, an increase in infectious diseases and the number of allergic agents. A certain role in the development of atopic dermatitis is played by disorders in the immune system of children, caused by a shortening of breastfeeding, early transfer to artificial feeding, maternal toxicosis during pregnancy, and poor nutrition of women during pregnancy and lactation.
Causes of development of atypical dermatitis
Atopic dermatitis is an inflammatory, chronically relapsing pathology of the skin, accompanied by constant itching, as well as eczematous and lichenoid rashes. The disease is also called allergic eczema, as it very often occurs at the same time as:
- bronchial asthma;
- food allergies;
- allergic rhinitis;
- conjunctivitis;
- ichthyosis. [12]
Atopic dermatitis most often develops in childhood - the prevalence among children reaches 15-30%; in 9 out of 10 cases it develops in the first year of life. The incidence in adults is 2-10%. Women suffer from it more often than men. Most cases occur in cities with high levels of pollution and cold climates. [3]
This is an immune-dependent pathology. The reasons for its development are associated with mutations in genes that are responsible for the synthesis of filaggrin, a structural skin protein involved in the formation of the stratum corneum, which, in turn, is responsible for the barrier functions of the skin. Like a brick wall, the stratum corneum of the epidermis retains water and does not allow a large number of allergens and microorganisms to enter the body. In patients with dermatitis, the synthesis of filaggrin is impaired, and the connections between the cells of the stratum corneum are damaged. Because of this, the skin retains moisture worse and is more sensitive to any external influences. The mechanism is as follows: the pathogen enters the body through damaged skin, and the immune system produces immunoglobulins. Against the background of these processes, symptoms of atopic dermatitis arise. [4]
Symptoms of atopic dermatitis
The initial signs of atopic dermatitis are usually observed in the first six months of life. This can be triggered by the introduction of complementary foods or transfer to artificial mixtures. By the age of 14-17, in almost 70% of people the disease goes away on its own, and in the remaining 30% it develops into an adult form. The disease can last for many years, worsening in the autumn-spring period and subsiding in the summer.
According to the nature of the course, acute and chronic stages of atopic dermatitis are distinguished.
The acute stage is manifested by red spots (erythema), nodular rashes (papules), peeling and swelling of the skin, the formation of areas of erosion, weeping and crusts. The addition of a secondary infection leads to the development of pustular lesions.
The chronic stage of atopic dermatitis is characterized by thickening of the skin (lichenification), pronounced skin patterns, cracks on the soles and palms, scratching, and increased pigmentation of the skin of the eyelids. In the chronic stage, symptoms typical of atopic dermatitis develop:
- Morgan's sign - multiple deep wrinkles in children on the lower eyelids
- Symptom of a “fur hat” - weakening and thinning of hair on the back of the head
- The symptom of “polished nails” is shiny nails with worn edges due to constant scratching of the skin.
- The symptom of “winter foot” is puffiness and hyperemia of the soles, cracks, and peeling.
There are several phases in the development of atopic dermatitis: infant (first 1.5 years of life), childhood (from 1.5 years to puberty) and adult. Depending on the age dynamics, features of clinical symptoms and localization of skin manifestations are noted, however, the leading symptoms in all phases remain severe, constant or periodically occurring skin itching.
The infant and childhood phases of atopic dermatitis are characterized by the appearance on the skin of the face, limbs, and buttocks of areas of bright pink erythema, against which bubbles (vesicles) and areas of weeping appear, followed by the formation of crusts and scales.
In the adult phase, foci of erythema are pale pink in color with a pronounced skin pattern and papular rashes. They are localized mainly in the elbow and popliteal folds, on the face and neck. The skin is dry, rough, with cracks and areas of peeling.
In atopic dermatitis, focal, widespread or universal skin lesions occur. Areas of typical localization of rashes are the face (forehead, area around the mouth, near the eyes), skin of the neck, chest, back, flexor surfaces of the limbs, inguinal folds, buttocks. Plants, house dust, animal hair, mold, and dry fish food can aggravate the course of atopic dermatitis. Atopic dermatitis is often complicated by a viral, fungal or pyococcal infection, and is a background for the development of bronchial asthma, hay fever and other allergic diseases.
What it is?
Atopic dermatitis (AD) is an allergic skin disease that usually occurs in early childhood in people with a hereditary predisposition to atopic diseases, has a chronic relapsing course, age-related features of the localization and morphology of inflammation, characterized by skin itching and caused by hypersensitivity to both allergens and non-specific irritants.
The problem of AD is becoming increasingly important in modern medicine. The increase in incidence in the last 10 years, the chronic course of the disease with frequent relapses, and the insufficient effectiveness of existing methods of treatment and prevention make this disease one of the most pressing medical problems.
Atopic dermatitis is largely classified as a childhood disease, since its symptoms manifest in childhood.
The manifestation of AD symptoms in children is observed at the age of:
- 6 months in 50-60% of cases;
- up to 1 year in 75% of cases;
- up to 7 years - in 80-85% of cases (according to various authors).
Among the adult population in developed countries, AD occurs in 0.2-2% (5.9% in Russia). Over the past decades, there has been a significant increase in AD, its course becomes more complicated, and its outcome is aggravated.
AD is often combined with other allergic diseases:
- in 40% - with bronchial asthma;
- in 25% of cases – with allergic rhinitis;
- in 8% of cases – with hay fever.
Risk factors for developing atopic dermatitis
internal non-immunological, immunological
- heredity burdened with allergies;
- high intrauterine sensitization of the fetus associated with the pathology of pregnancy and childbirth;
- early artificial feeding;
- pathology of the gastrointestinal tract;
- intestinal dysbiosis from birth;
- frequent ARVI;
- the presence of foci of chronic infection;
- factors causing dry skin (impaired sweating, lack of interstitial fluid), changes in skin lipids, decreased itching threshold;
external
- exposure to reactive chemical compounds, food antigens, microorganisms, stressful situations, climatic conditions.
Trigger factors (provoking factors)
- Food product (usually cow's milk protein, egg, cereals, soy fish)
- Inhalation allergens (house dust, house dust mites, plant pollen). Microorganisms (St. aureus, V. Herpes, Malasseria furfur, especially Malasseria spp. and other mold fungi.)
Irritants
- Sex hormones
- Stress
- Climatic factors
The development of sensitization to these allergens occurs when they enter through the respiratory tract, gastrointestinal tract, or contact route (through the skin) and leads to the appearance of respiratory manifestations of atopy, such as allergic rhinitis and bronchial asthma. In more than 80% of patients, AD is associated with allergic rhinitis and in 30%-40% with bronchial asthma. In older children, food sensitization transforms into sensitization to aeroallergens:
Skin changes in AD are that with allergic inflammation, the skin of patients has a number of features and is characterized by:
- nonspecific hyperactivity to various stimuli and antigens;
- increased dryness;
- disorders of ceramide biosynthesis;
- increased physiological desquamation of the epithelium;
- thickening of the stratum corneum with the development of hyperkeratosis and pronounced peeling.
- Intense itching and scratching of the skin in combination with its hyperreactivity and a lower sensitivity threshold for itching determine the presence of a vicious circle: dry skin, itchy skin, inflammation.
Classification of AD
- Exogenous (allergic) AD associated with respiratory allergies and sensitization to aeroallergens. The risk of developing respiratory allergies in patients suffering from AD, according to various authors, ranges from 30 to 80%. 60% of AD patients have a latent tendency to develop bronchial asthma, and 30-40% develop it;
- Endogenous (non-allergic) AD, not associated with respiratory allergies and sensitization to any allergens.
Stages of the disease:
Age period:
- I age period – infant (up to 2 years)
- II age period – children (from 2 to 13 years)
- III age period – adolescence and adulthood (over 13 years old)
Stages of the disease:
- Exacerbation stage Phase of pronounced clinical manifestations
- Phase of moderate clinical manifestations
- Incomplete remission
Complications
- pyoderma;
- viral infection;
- fungal infection
Severity of the process
- mild course
- moderate severity
- severe course
Symptoms that require you to contact an allergist-immunologist
Main clinical signs of atopic dermatitis
- itchy skin;
- typical morphology and location of the rash according to the age period;
- tendency towards a chronic relapsing course;
- personal or family history of atopic disease;
- seasonality of exacerbation (deterioration in the cold season and improvement in summer);
- exacerbation of the process under the influence of provoking factors (allergens, irritants, foods, emotional stress); - connection between exacerbations and exposure to allergens;
- dry skin;
- white dermographism;
- tendency to skin infections;
- cheilitis (seed);
- Denny-Morgan sign (additional fold of the lower eyelid);
- hyperpigmentation of the periorbital area (around the eyes);
- increased levels of total and allergen-specific IgE in serum;
- peripheral blood eosinophilia.
Age characteristics and localization of skin lesions
| age periods | morphological characteristics | localization |
| infant (up to 2 years) | The predominance of the exudative form of blood pressure Inflammation is acute or subacute in nature Hyperemia, swelling, weeping, crusts are present | Face, outer surface of the legs, flexion and extension surfaces of the extremities. By the end of the period, the lesions are localized mainly in the area of the elbows and popliteal fossae, in the area of the wrists and neck. |
| children's (2-13 years) | The process is in the nature of chronic inflammation: erythema, papules, multiple peeling, thickening of the skin (infiltration), increased skin pattern (lichenization), multiple excoriations (scratching), cracks. At the sites where the rash resolves, there are areas of hypo- or hyperpigmentation. Possible Denny-Moran sign | Elbow and popliteal folds, back of the neck, flexor surfaces of the ankle and wrist joints, behind the ears |
| teenage and adult (from 13 and from 18 years old) | The phenomena of infiltration with lichenification predominate; erythema has a bluish tint. Papules merge into foci of continuous papular infiltration. | Upper body, face, neck, upper limbs |
The doctor evaluates
- the nature of the rashes and their correspondence to the age period
- presence or absence of scratching (intensity of skin itching)
- additionally, if any, symptoms of allergic rhinitis, allergic conjunctivitis, bronchial asthma
After which laboratory tests are prescribed to confirm the diagnosis.
Laboratory and instrumental studies
- Clinical blood test
- Determination of the concentration of total IgE in blood serum
- Skin tests with allergens to detect an IgE-mediated reaction
- Provocative test with food allergens
- determination of allergen-specific IgE-AT in blood serum
In addition, a general clinical examination is carried out, for example, 80-90% of patients have concomitant pathology of the digestive system. It has long been noticed that if there are several sources of the inflammatory process in the body, they “warm up” and increase the severity of each other. Therefore, after treating the concomitant pathology, the inflammatory process on the skin subsides and we need much less time and the amount of drugs used to stop it completely.
In light of all of the above, it is quite logical to additionally assign such studies:
- clinical and biochemical blood test
- general urine analysis
- coproocystoscopy
- bacteriological examination of feces
- esophagogastoduodenoscopy
- detection of Helicobacter pylori using a breath test
- Ultrasound of the abdominal organs
- X-ray examination of the chest and paranasal sinuses
- FVD assessment
- immunological examination (all immunoglobulins, possible selective deficiency of IgA, which often accompanies AD)
Specialist consultations:
- dermatologist - to establish a diagnosis, carry out differential diagnosis with other skin diseases, select and correct local therapy, and educate the patient.
- repeat consultation - in case of poor response to local glucocorticosteroid therapy or secondary infection.
- nutritionist – to create and correct an individual diet
- ENT – identification and sanitation of foci of chronic infection, early detection of AR symptoms
- neuropsychiatrist - for severe itching, behavioral disorders, psychotherapeutic treatment, training in relaxation techniques, stress relief and behavior modification.
Complications
The main reason for the development of complications in atopic dermatitis is constant trauma to the skin as a result of scratching. Violation of the integrity of the skin leads to a decrease in its protective properties and contributes to the addition of a microbial or fungal infection.
The most common complication of atopic dermatitis is bacterial skin infections - pyoderma. They manifest themselves as pustular rashes on the body, limbs, and scalp, which dry out and form crusts. At the same time, general well-being often suffers, and body temperature rises.
The second most common complication of atopic dermatitis is viral skin infections. Their course is characterized by the formation of bubbles (vesicles) filled with clear liquid on the skin. The causative agent of viral skin infections is the herpes simplex virus. The face (skin around the lips, nose, ears, eyelids, cheeks), mucous membranes (conjunctiva of the eyes, oral cavity, throat, genitals) are most often affected.
Complications of atopic dermatitis are often fungal infections caused by yeast-like fungi. The affected areas in adults are often skin folds, nails, hands, feet, scalp, and in children - the oral mucosa (thrush). Often fungal and bacterial infections are observed together.
Treatment of atopic dermatitis
Treatment of atopic dermatitis is carried out taking into account the age phase, severity of the clinical picture, concomitant diseases and is aimed at:
- exclusion of allergic factor
- desensitization (reduced sensitivity to allergen) of the body
- itching relief
- detoxification (cleansing) of the body
- removal of inflammatory processes
- correction of identified concomitant pathology
- prevention of relapses of atopic dermatitis
- combating complications (if an infection occurs)
Various methods and medications are used to treat atopic dermatitis: diet therapy, PUVA therapy, acupuncture, plasmapheresis, specific hyposensitization, laser treatment, corticosteroids, allergoglobulin, cytostatics, sodium cromoglycate, etc.
Diet therapy
Regulating nutrition and following a diet can significantly improve the condition and prevent frequent and severe exacerbations of atopic dermatitis. During periods of exacerbation of atopic dermatitis, a hypoallergenic diet is prescribed. At the same time, fried fish, meat, vegetables, rich fish and meat broths, cocoa, chocolate, citrus fruits, black currants, strawberries, melon, honey, nuts, caviar, and mushrooms are removed from the diet. Products containing dyes and preservatives are also completely excluded: smoked meats, spices, canned food and other products. For atopic dermatitis, a hypochloride diet is indicated - limiting the amount of table salt consumed (however, not less than 3 g of NaCl per day).
In patients with atopic dermatitis, there is a violation of the synthesis of fatty acids, so diet therapy should include food supplements saturated with fatty acids: vegetable oils (olive, sunflower, soybean, corn, etc.), linoleic and linolenic acids (vitamin F-99).
Drug treatment
Drug therapy in the treatment of atopic dermatitis includes the use of tranquilizers, antiallergic, detoxification and anti-inflammatory drugs. The most important in treatment practice are drugs that have an antipruritic effect - antihistamines (antiallergic) drugs and tranquilizers. Antihistamines are used to relieve itching and swelling of the skin, as well as for other atopic conditions (bronchial asthma, hay fever).
A significant disadvantage of first-generation antihistamines (mebhydrolin, clemastine, chloropyramine, hifenadine) is the rapidly developing addiction of the body. Therefore, these medications must be changed every week. The pronounced sedative effect, leading to a decrease in concentration and impaired coordination of movements, does not allow the use of first-generation drugs in the pharmacotherapy of people of certain professions (drivers, students, etc.). Due to the atropine-like side effects, a number of diseases are contraindications to the use of these drugs: glaucoma, bronchial asthma, prostate adenoma.
The use of second-generation antihistamines (loratadine, ebastine, astemizole, fexofenadine, cetirizine) is much safer in the treatment of atopic dermatitis in people with concomitant pathologies. They do not become addictive, and there are no atropine-like side effects. The most effective and safest antihistamine used to date in the treatment of atopic dermatitis is loratadine. It is well tolerated by patients and is most often used in dermatological practice for the treatment of atopy.
To alleviate the condition of patients with severe attacks of itching, drugs affecting the autonomic and central nervous systems (hypnotics, sedatives, tranquilizers) are prescribed. The use of corticosteroid drugs (methylprednisolone or triamcinolone) is indicated for limited and widespread skin lesions, as well as for severe, unbearable itching that is not relieved by other medications. Corticosteroids are prescribed for several days to relieve an acute attack and are discontinued with a gradual reduction in dose.
In severe cases of atopic dermatitis and severe symptoms of intoxication, intravenous infusion of infusion solutions is used: dextran, salts, saline, etc. In some cases, it is advisable to carry out hemosorption or plasmapheresis - methods of extracorporeal blood purification. With the development of purulent complications of atopic dermatitis, the use of broad-spectrum antibiotics in age-specific dosages is justified: erythromycin, doxycycline, metacycline for 7 days. When a herpes infection occurs, antiviral drugs are prescribed - acyclovir or famciclovir.
For recurrent complications (bacterial, viral, fungal infections), immunomodulators are prescribed: solusulfone, thymus preparations, sodium nucleinate, levamisole, inosine pranobex, etc. under the control of blood immunoglobulins.
External treatment
The choice of external therapy method depends on the nature of the inflammatory process, its prevalence, the age of the patient and the presence of complications. For acute manifestations of atopic dermatitis with weeping surfaces and crusts, disinfectant, drying and anti-inflammatory lotions (infusion of tea, chamomile, Burov's liquid) are prescribed. When stopping an acute inflammatory process, pastes and ointments with antipruritic and anti-inflammatory components are used (ichthyol 2-5%, tar 1-2%, naftalan oil 2-10%, sulfur, etc.). The leading drugs for external therapy of atopic dermatitis remain corticosteroid ointments and creams. They have antihistamine, anti-inflammatory, antipruritic and decongestant effects.
Light treatment of atopic dermatitis is an auxiliary method and is used when the disease is persistent. Ultraviolet irradiation procedures are carried out 3-4 times a week and practically do not cause adverse reactions (except for erythema).
Treatment
Therapy for children and adults is individual. Treatment is based on the collected data - age, time and causes of relapses, forms of manifestations, concomitant diseases, the degree of activity of the process at the time of contacting the doctor, the presence of complications.
Treatment of atopic dermatitis is carried out in parallel in several directions:
- general drug treatment;
- diet development;
- anti-inflammatory therapy with external agents;
- elimination of factors that provoke relapses, according to the doctor’s recommendations;
- climatotherapy;
- properly selected cosmetic care without dyes and fragrances.
GCS is used as external therapy - this is the first thing prescribed to the patient. When prescribing, doctors must clearly prescribe the dosage, treatment plan and timing, take into account contraindications, and choose the best progressive drugs.
Antihistamines are used as the basis of general drug treatment. Treatment of atopic dermatitis is carried out in different ways depending on what phase the patient is in - acute or chronic. Treatment for adults differs from treatment for infants and children.
During the acute phase, the following are used:
- 2nd generation antihistamines for 4-6 weeks;
- local lotions - oak bark tincture, tannin solution, rivanol solution, if there is exudation, dyes, for example, fucorcin and Castelani liquid);
- external glucocorticosteroids for 3-7 days;
- systemic corticosteroids (if therapy does not produce the expected results).
Chronic phase:
- 2nd generation antihistamines for 3-4 months;
- external corticosteroids;
- combination corticosteroids;
- immunosuppressive drugs;
- polyunsaturated fatty acids.
Additives in antihistamines can cause exacerbation, so the doctor should monitor the progress of treatment and promptly change the drug to another one that has other side additives.
After treatment has given results, it is important to carry out prevention to prevent the development of a new exacerbation. For this purpose, 3rd generation antihistamines are used, which are taken for 6 months (therapy can be extended), polyunsaturated fatty acids, immunomodulators and specific immunotherapy.
The use of first-generation drugs is currently not widespread, since they penetrate the blood-brain barrier, cause many side effects, reduce performance, tachyphylaxis, and dry mucous membranes.
Prevention
There are two types of prevention of atopic dermatitis: primary, aimed at preventing its occurrence, and secondary, anti-relapse prevention. Measures for the primary prevention of atopic dermatitis should begin during the period of intrauterine development of the child, long before his birth. A special role during this period is played by toxicosis of the pregnant woman, taking medications, and occupational and food allergens.
Particular attention to the prevention of atopic dermatitis should be paid in the first year of a child’s life. During this period, it is important to avoid excessive medication and artificial feeding, so as not to create a favorable background for the body’s hypersensitivity to various allergic agents. Following a diet during this period is no less important for a nursing woman.
Secondary prevention aims to prevent exacerbations of atopic dermatitis, and, if they occur, to alleviate their course. Secondary prevention of atopic dermatitis includes correction of identified chronic diseases, exclusion of exposure to disease-provoking factors (biological, chemical, physical, mental), adherence to hypoallergenic and elimination diets, etc. Prophylactic use of desensitizing drugs (ketotifen, sodium cromoglycate) during periods of probable exacerbations (autumn, spring) allows you to avoid relapses. As anti-relapse measures for atopic dermatitis, treatment is indicated in the resorts of the Crimea, the Black Sea coast of the Caucasus and the Mediterranean.
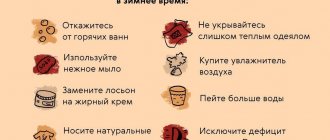
Particular attention should be paid to daily skin care and the correct choice of underwear and clothing. When taking a daily shower, do not wash with hot water and a washcloth. It is advisable to use gentle hypoallergenic soaps (Dial, Dove, baby soap) and a warm shower, and then gently pat the skin with a soft towel without rubbing or injuring it. The skin should be constantly moisturized, nourished and protected from adverse factors (sun, wind, frost). Skin care products should be neutral and free of fragrances and dyes. In linen and clothing, preference should be given to soft natural fabrics that do not cause itching and irritation, and also use bedding with hypoallergenic fillings.
Main goals and directions of therapy
AD is a chronic disease, so treatment should be gradual and long-term.
- Elimination of causally significant allergens with the prescription of diet therapy and control of adverse environmental factors;
- Elimination or reduction of inflammatory changes on the skin and skin itching.
- Restoring the structure and function of the skin (improving microcirculation and metabolism in lesions; normalizing skin moisture).
- Prevention of the development of severe forms of the disease, leading to a decrease in the quality of life of patients and their disability.
- AD is based on allergic inflammation, so the basis of treatment is antihistamines and anti-inflammatory drugs.
- Multiple organ lesions in AD require systemic basic therapy with antiallergic drugs.
- Identification and treatment of concomitant diseases that aggravate the course of AD. (treatment of pathologies of the digestive system, metabolite and antioxidant therapy, normalization of functional disorders of the nervous system, rehabilitation of foci of chronic infection).
Areas of AD therapy:
- diet therapy and elimination measures to eliminate causally significant allergens;
- systemic pharmacotherapy;
- antihistamines;
- membrane stabilizing drugs;
- drugs that normalize the functions of the digestive system;
- vitamins;
- immunomodulators;
- drugs that regulate the function of the ANS;
- preparations containing unsaturated fatty acids;
- antibiotics;
- systemic corticosteroids (for special indications);
- External therapy and rehabilitation.
Correction of immune disorders in AD
- Direct methods of immunocorrection are allergen-specific immunotherapy (ASIT), therapeutic plasmapheresis, and immunopharmacotherapy itself with corrective drugs, as well as the use of modern immunosuppressants.
- ASIT is the only method of therapeutic influence on all pathogenetically significant parts of the allergic process, which has a long-term preventive effect and allows for the reverse development of the pathological process, because at the same time, a decrease in nonspecific tissue sensitivity to the allergen is formed, hyperreactivity decreases, and signs of allergic inflammation are suppressed, which indicates a restructuring of the nature of the cellular and cytokine response from Th2 to Th1 - a response with a decrease in the content and production of Ig E.
Indications for ASIT are determined by a set of criteria:
- diffuse or widespread form of AD;
- moderate/severe;
- clinically significant sensitization to aeroallergens, confirmed on the basis of anamnesis, positive skin tests and/or detection of specific Ig E antibodies to a given allergen;
- hereditary burden of allergic diseases, especially respiratory allergies;
- hypersensitivity to one group of allergens.
Forecast
Children suffer the most severe manifestations of atopic dermatitis; with age, the frequency of exacerbations, their duration and severity become less pronounced. Almost half of patients recover by the age of 13-14 years. Clinical recovery is considered a condition in which there are no symptoms of atopic dermatitis for 3–7 years.
Periods of remission in atopic dermatitis are accompanied by subsidence or disappearance of symptoms of the disease. The time interval between two exacerbations can range from several weeks to months and even years. Severe cases of atopic dermatitis occur with virtually no clear intervals, constantly relapsing.
The progression of atopic dermatitis significantly increases the risk of developing bronchial asthma, respiratory allergies and other diseases. For atopics, an extremely important point is the choice of professional field of activity. They are not suitable for professions that involve contact with detergents, water, fats, oils, chemicals, dust, animals and other irritants.
Unfortunately, it is impossible to completely protect yourself from the influence of the environment, stress, illness, etc., which means that there will always be factors that aggravate atopic dermatitis. However, careful attention to your body, knowledge of the peculiarities of the course of the disease, timely and active prevention can significantly reduce the manifestations of the disease, prolong periods of remission for many years and improve the quality of life. And under no circumstances should you try to treat atopic dermatitis on your own. This can cause complicated variants of the course of the disease and serious consequences. Treatment of atopic dermatitis should be carried out by allergists and dermatovenerologists.
Diagnosis of skin pathology
At the moment, there is no specific laboratory test that can detect atopic dermatitis. The diagnosis is made based on the symptoms present and an assessment of the severity of the disease. The severity of atopic dermatitis is determined using the SCORAD scale, which includes a number of objective and subjective criteria. The first includes the strength and prevalence of lesions, the subjective - the intensity of itching during the day and night. [9]
To establish atopic dermatitis, it is necessary to identify specific IgE antibodies to allergens. For this purpose, cutaneous patch tests are performed, but only if the patient has delayed-type hypersensitivity.
Atopic dermatitis is often confused with other diseases. To avoid mistakes, differential diagnosis is carried out using laboratory tests:
- detection of platelet pathology;
- determination of immune status;
- microscopy of scales. [9]
Sometimes, to distinguish atopic dermatitis from other pathologies, the localization of the rash is sufficient. So vulgar psoriasis affects the extensor surfaces, while the manifestations of atopic dermatitis are localized in the flexor areas.