What is paronychia and how does it differ from felon?
In short, felon is a general medical name for various types of purulent inflammation of the tissues of the hands and feet. These inflammations can have different localizations on the affected limb, being cutaneous, subcutaneous, articular and even bone. Paronychia is a special case of panaritium: it is an inflammation of the tissue around the nail plate. Sometimes paronychia is called periungual felon. Paronychia in children occurs mainly as a result of mechanical trauma. It can happen during a manicure or pedicure, or while playing - a child can injure the skin near the nail or plant a splinter, get burned, or spend some time in tight, uncomfortable shoes. The child may unsuccessfully bite or tear off an interfering hangnail or bite his nails. Of course, the wound itself does not necessarily lead to tissue inflammation. Therefore, any cuts and punctures of the skin should be treated with an antiseptic as soon as possible. But if an infection gets into the wound, the tissues turn red, swell, and later pus may appear - these are already manifestations of paronychia. Less commonly, it happens that paronychia is not preceded by trauma. In adult patients, the cause is most often a fungus, in children - staphylococcus and streptococcus. In general, children suffer from paronychia more often than adults because they are more likely to be injured and have poor hygiene.
Atopic dermatitis in children: how to relieve itching?
19.02.2021
Atopic dermatitis is a skin disease, the main symptom of which is severe itching, causing the skin to crack, become wet and become covered with a crust or rash. In most cases, the skin is extremely dry and hypersensitive. This disease very often begins at an early age and, with interruptions of remission, accompanies a person throughout his life.
Causes of atopic dermatitis
The exact causes of this disease are still not reliably known. It is generally believed that the disease is inherited and is caused by changes in the gene responsible for the barrier function of the skin. If one of the parents has atopy, then most likely it will manifest itself in the child. The epidermis is the outer layer of the skin that protects it from external irritants and microbes. In people with atopic dermatitis , it is genetically impaired and does not fulfill its function: it does not moisturize the skin, which makes it dry and flaky, prone to allergic reactions .
Irritants for such skin are:
- food products (citrus fruits, tomatoes, fried foods, nuts, chocolate, etc.);
- household chemicals and hygiene products;
- clothing made of synthetic and woolen materials;
- dry indoor air leads to peeling of the skin;
- exercise and heavy sweating ;
- stressful situations and nervous tension;
- hot and chlorinated water.
All this leads to severe itching, redness and excessive dryness. Itching usually worsens in the evening and at night, as well as in the morning.
How to help a child with severe itching?
Itching is very difficult for children. They will not be able to sleep until they scratch the problem area until it bleeds . It is very difficult to explain to a child that scratching will then take a long time and be painful to heal. An infection can get into the wound, causing suppuration and mycoses. Because of the constant discomfort caused by itching, children become nervous, irritable, their sleep is disturbed, and they begin to feel embarrassed to walk around in open clothes.
If the child begins to itch and signs of atopy appear, you should consult a dermatologist . He will prescribe antihistamines and corticosteroid ointments and creams. These medications can soothe itching, relieve swelling and inflammation.
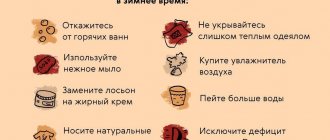
In addition to these remedies, the following recommendations can help reduce itching:
- following a hypoallergenic diet . It is necessary to exclude foods that cause an allergic reaction (chocolate, citrus fruits, fish, fried foods, etc.). Along with medications, diet is mandatory to achieve relief from the disease;
- The child should be washed in warm, but not hot water, using products that have a neutral pH, without dyes or fragrances;
- moisturize the skin after bathing with creams with emollients. Emollients are substances that protect it from moisture loss and restore its protective function. Their regular use can help you avoid medications;
- Regularly moisten the room using ventilation and a humidifier;
- maintain the air temperature no more than 22 degrees;
- do not wrap the child up, do not allow excessive sweating . Cold is one way to soothe itching;
- trim the child’s fingernails to prevent severe scratching of the skin;
- wet skin wraps. They help keep the skin moisturized and promote more active penetration of special ointments that are used during this procedure. Due to the evaporation of water from the bandage , the surface of the skin is cooled, which helps reduce itching and pain. Before performing wraps, you should consult your doctor . In severe forms of dermatitis, wraps are carried out in medical institutions.
Atopic dermatitis is more severe in children than in adults. For treatment, you must consult a doctor and teach your child to live with this disease, following diet and other recommendations.
Published in Dermatology Premium Clinic
Which doctor should I make an appointment with if my child has an inflamed finger?
If you have recently discovered inflammation around your child's nail, it makes sense to first make an appointment with your pediatrician. In children, paronychia often causes not only local pain and discomfort, but also a general deterioration in well-being: fever, tearfulness and moodiness from a constant irritant, sleep disturbances. You may even experience weakness and nausea. All these are consequences of intoxication. Therefore, you need to contact your pediatrician as soon as possible. If you leave it too long, there is a chance that the infection will affect the nail, and then it may even have to be removed - partially or completely. After examining the finger, a competent pediatrician will either prescribe conservative therapy for local treatment of the damaged area, or, if the infection has already developed to a purulent stage, refer the little patient to a specialist - a pediatric surgeon. If you find pus on your own, you can immediately make an appointment at a children's clinic directly with a surgeon, bypassing the pediatrician.
How is paronychia treated?
At the stage of conservative treatment, depending on what caused the lesion, the doctor may prescribe antifungal drugs or antibiotics - both local and general, taken orally. Warm lotions are also usually prescribed and applied to the affected area. Levomekol is often prescribed for treatment, which has a good anti-inflammatory effect, including during infection with staphylococcus. Surgical treatment of paronychia is no different from any other purulent inflammation. The abscess is opened, cleaned of purulent contents, the wound cavity is drained, if necessary, and the affected area is disinfected. Until recovery, you will have to change the bandage every day. This procedure is performed under local anesthesia and takes on average 20 minutes. The child may be prescribed antibiotics - local, in the form of an ointment, or for oral administration. During the rehabilitation period, the finger cannot be wet. Therefore, you will have to refuse to visit the pool and sauna. You can swim if the child himself or the adult who helps him can make sure that the finger remains dry.
The current pandemic is impacting dermatology practice. In particular, the number of face-to-face consultations is decreasing in favor of teledermatology, and there is no certainty regarding the outcome of coronavirus infection in patients with common inflammatory dermatoses (psoriasis and atopic dermatitis) receiving immunosuppressive/immunomodulatory systemic therapy. However, dermatologists around the world are collecting data on skin lesions that may be undetected symptoms of COVID-19.
Vladimir Adaskevich, Head of the Department of Dermatovenereology of VSMU, Chairman of the Belarusian Public Organization of Dermatovenereologists and Cosmetologists, Professor, Doctor of Medicine. Sciences. From urticaria to “covid fingers”: world experience
It should be noted that many viral diseases, including chickenpox, measles and mononucleosis, are accompanied by tell-tale skin rashes, often the result of the body's heightened inflammatory response to fight infection. There are now increasing reports and preliminary observations indicating that SARS-CoV-2 may also infect the skin.
At the end of March 2022, an Italian doctor sent a letter to the editor of the Journal of the European Academy of Dermatology and Venereology describing skin conditions observed in 20% of 88 patients with COVID-19 in Lombardy, the worst-hit region of Italy. Most developed a red rash on the torso, and some developed hives-like rashes or chickenpox-like blisters.
In early April, the French Society of Dermatology, which represents more than 400 specialists, issued a statement that patients with probable COVID-19 had reported hives, a red rash and lesions on the extremities that resembled frostbite. Finally, in mid-April, a letter to the editor of the Journal of the American Academy of Dermatology was received from a group of Italian doctors describing chickenpox-type rashes as a rare but specifically associated manifestation of COVID-19. However, it is difficult to determine whether these skin symptoms are actually caused by the SARS-CoV-2 virus or are a side effect of the medications used to treat the virus.
The condition of pseudofrostbite, described by French dermatologists, in the United States is called “covid fingers” - it is characterized by purple, bruise-like swelling and swelling. The American Academy of Dermatology registry has documented more than 100 such cases. “Covid fingers” are observed quite often during illness and, as a rule, among patients with several other symptoms of COVID-19.
However, despite the name, it is not yet completely clear that this condition is caused specifically by coronavirus infection. Many individuals with these symptoms were not tested for COVID-19 because they did not require intensive medical monitoring. In some patients with this symptom, coronavirus infection was not confirmed, but there was no other explanation for the abnormal skin condition. In this connection, it was assumed that in some cases of asymptomatic or mild disease, “Covid fingers” developed quite late, so the tests came with a negative result.
It is clear that in patients with confirmed COVID-19, skin manifestations are not the main concern, but dermatological care is necessary to relieve discomfort. In such cases, specialists use typical local therapy. But some preliminary research suggests that patients with COVID-19 may develop rashes due to impaired blood flow, which is more serious: small blood clots in the skin may indicate the presence of similar ones elsewhere in the body.
Chinese researchers, based on data on 140 patients infected with the new coronavirus, identified drug hypersensitivity in 11.4% and urticaria in 1.4% of patients as skin manifestations.
British doctors described the first case of a new inflammatory condition called Kawasaki disease in a 6-month-old baby with symptoms including fever, a persistent red rash on the arms and legs; dry cracked lips, bumps on the tongue, swollen hands, conjunctivitis. The test for coronavirus infection was positive.
A Kawasaki disease-like syndrome believed to be caused by COVID-19 has caused the death of 12 children in the UK. However, some researchers are not sure whether these deaths are related to coronavirus infection.
It is not yet known whether skin lesions and disruption of the skin barrier can facilitate transmission of SARS-CoV-2 through indirect contact. It remains to be determined whether specific mucosal and skin lesions are associated with coronavirus infection, although some unpublished observations indicate cases of transient smallpox-like exanthema in the early phase of the disease.
The most common skin manifestations of COVID-19
A peer review of the following study was published at the end of April in the British Journal of Dermatology. Spanish experts described the skin rashes they observed in 375 patients with coronavirus infection over a 2-week period. Five types of rash were identified: acral areas of erythema-edema with vesicles or pustules (pseudofrostbite) (19% of cases); other vesicular eruptions (9%); urticarial lesions (19%); other maculopapules (47%); livedo or necrosis (6%).
- Acral areas of erythema-edema with vesicles or pustules
(pseudofrostbite). These lesions, which affect the hands and feet, may resemble chilblains (small itchy swellings of the skin) with small red or purple spots caused by subcutaneous hemorrhages. The rashes are usually asymmetrical. They are associated with younger patients, last on average 12.7 days, develop late in the course of COVID-19, and are observed in less severe disease. The rash sometimes causes pain (32%) or itching (30%).
- Other vesicular eruptions.
Manifested by the sudden development of blisters on the trunk, which could also affect the limbs. The blisters were sometimes filled with blood and became larger or more widespread. They are associated with middle-aged patients, last on average 10.4 days, often appear (15%) before the onset of other symptoms, and are observed in moderate disease severity. Itching is frequent (68%).
- Urticarial lesions.
They are pink or white swellings of the skin that resemble the usually itchy blisters of hives. The rashes mainly developed on the trunk or spread throughout the body. In several cases observed on the palms.
- Other maculopapules.
Small, flat and raised red bumps. In some cases, they were located around the hair follicles, and varying degrees of peeling were also noted. Some of the elements were described as similar to pityriasis rosea. Blood spots under the skin may also be present, either in the form of specks/dots or larger areas. These rashes are associated with shorter duration (6.8 days on average for urticarial lesions and 8.6 for maculopapular lesions), usually appear along with other symptoms, and are observed with more severe COVID-19 (2% mortality in the sample). Itching is very common in urticarial lesions (92%), and in maculopapular lesions it occurs in 57% of cases.
- Livedo or necrosis.
Livedo is the result of impaired circulation in the blood vessels of the skin, causing a vascular pattern in the form of a red or blue mesh to appear on the surface. Necrosis means the premature death of skin tissue. These two symptoms reflect varying degrees of vascular occlusion, with narrowing or blocking of arteries that restrict blood flow to specific areas of the body (in this case, the torso or extremities). Such rashes are associated with older patients and more severe disease (mortality rate 10%). However, these manifestations of COVID-19 are more variable, including transient livedo in patients who did not require hospitalization.
The researchers noted that some of the skin manifestations associated with COVID-19 are common and can have many causes. This applies, in particular, to maculopapules and urticarial lesions. By themselves, they do not help in making a diagnosis. Livedo and necrosis, on the other hand, are quite rare and most often occur in older and sicker patients. However, it is difficult to say whether they are caused directly by COVID-19 or are an indicator of complications.
Inflammatory skin diseases and coronavirus
A team of dermatologists in New York City is studying the connection between COVID-19 and pre-existing inflammatory skin diseases such as eczema and psoriasis. To do this, Mount Sinai Hospital's Icahn School of Medicine is recruiting specialized patients undergoing treatment in hopes of studying how susceptible they are to COVID-19 compared to others. And since many of the drugs used in this category are aimed at reducing inflammation in the body, doctors speculate that these drugs may also improve the immune system's ability to fight SARS-CoV-2. The results of the Mount Sinai study and all data on dermatological reactions to COVID-19 are still preliminary. American dermatologists suggest that patients with unusual skin rashes use telemedicine to consult with a specialist who will help determine whether these manifestations are related to COVID-19 and justify the reason for self-isolation.
The statement of the European Task Force on Atopic Dermatitis (ETFAD) is important. Patients with severe atopic dermatitis often receive immunomodulatory systemic drugs, which also affect the severity of comorbid pathology (bronchial asthma, COPD, eosinophilic esophagitis, kidney disease and allergies).
Abrupt cessation of stable systemic therapy may lead to exacerbation of all of these diseases. If it must be suspended, patients should be provided with sufficient local therapy, coupled with recommendations on the amount necessary to prevent exacerbations, before systemic treatment is resumed. At the same time, monitoring and treatment of comorbid conditions such as bronchial asthma are required. In severe and complicated cases, hospitalization in a specialized treatment center is required.
Severe and untreated atopic dermatitis is known as a risk factor for disseminated viral skin disease. On the other hand, many traditional systemic immunomodulatory drugs, such as cyclosporine, may interfere with the body's defense mechanisms against viral infection. It is not yet known how SARS-CoV-2 affects patients with atopic dermatitis, including those receiving immunomodulatory therapy.
Disseminated cutaneous viral infection (eczema herpeticum, herpes zoster, or seasonal nasopharyngitis) seen in atopic dermatitis may serve as a potential model for evaluating COVID-19 treatment in patients receiving systemic therapy. But the conclusions in this case are very limited. It is believed that targeted therapies that selectively target type 2 inflammation, in particular the use of biological agents, do not increase the risk of viral infections and may be preferable to traditional immunosuppressive drugs in a pandemic.