Congenital abnormalities of the hand
Hand surgeons at the CONSTANTA Clinic in Yaroslavl correct various deformities with which children are born. Sometimes, when examining the fetus with ultrasound (ultrasound) of a pregnant woman, the problem already becomes noticeable, but more often parents encounter it unexpectedly, after the birth of the baby. Experts find it difficult to name its exact cause. Two versions are considered the most likely:
- Genetic predisposition There is an “error” in the genetic parental information passed on to the child. The “wrong” gene of one of the parents, “dormant” for a number of generations, manifested itself in the form of a defect that can be further inherited.
- Spontaneous malformations These include cases not related to heredity when malfunctions occur during the formation of the fetus in the mother's womb. The tiny hand develops in the 4th week of pregnancy, when the fetus is still very small. Its size is no larger than a grain of rice, and by the 8th week the hand should already have all the sections of an adult hand. From the 4th to the 8th week is an important period of pregnancy for the formation of hands. Deviations from the norm can be caused by the slightest disruptions in the functioning of the mother’s body. Often these are infectious diseases of the mother.
Brief descriptions of common types of anomalies
- Syndactyly - fingers fused with each other (webbed) The deformity is characterized by the fusion of two or more fingers. It can be complete along the entire length or partial, affecting bone or only soft (skin) tissues. Syndactyly is one of the most common types of defects. On average, 2 out of 10 thousand babies are born with it.
- Polydactyly – six-fingered, extra (double) fingers. The pathology is characterized by the presence of more than 5 fingers on the baby’s hand. Often the very first (large) one is doubled. The second most common case is doubling of the last (little finger). A type of polydactyly with double fingers located in the center is not often found.
- Clinodactyly - curvature or bending Curvature is often observed in the middle phalanx. In most cases - on the little finger. The problem is usually cosmetic in nature. Surgical treatment is performed for aesthetic reasons.
- Stenosing ligamentitis - a finger that clicks when moving (Knott's disease) A defect that is addressed to our hand surgeon very often. The anomaly is manifested by the fact that active flexion and extension movements of the finger, most often the first (thumb), are accompanied by a characteristic click. As the disease progresses, bending becomes impossible at all. A spindle-shaped seal is tactilely felt on the surface of the palm, moving along the finger as it moves. This reveals a defect in the flexor tendon that requires correction.
- Brachydactyly, ectrodactyly - shortening A congenital defect is characterized by underdevelopment of the finger, shortening of the length up to absence. Brachydactyly differs from ectrodactyly in the presence of nail plates. Often both types of defects can be combined with syndactyly. These pathologies are called symbrachydactyly and ectrosyndactyly.
- Brachymetacarpy - short metacarpal bone The defect is manifested by an abnormally short finger due to a sunken “knuckle”. The retraction is clearly noticeable in a compressed cam position. The defect affects the 3rd, 4th, 5th metacarpal bones in different combinations. The anomaly is bilateral, with simultaneous damage to the metatarsal bones of the legs - brachymetarization.
- Camptodactyly – flexion deformity The fifth toes are most often affected by congenital flexion contracture. Such a little finger may have deformations of varying complexity, and cannot straighten in a passive position during active movement. In this case, there may be no fold on the surface of the palm, as the skin stretches like a sail.
- Hypoplasia is a specific pathology of the thumb. The defect can be expressed by shortening or thinning of the finger. It may be completely absent or remain suspended on a thin skin stalk. Often this deformity is accompanied by a radial type of clubhand.
- Congenital grooves (constrictions) The anomaly looks like a constriction from a thin thread tightly tied to a limb. A common developmental deviation that has a variety of locations on the limbs: thigh, lower leg, forearm, fingers, etc.
- Concrescence is a fusion . The pathology consists of the presence of two fingers on one metacarpal bone. Since they share a common bone, the functioning of the metacarpophalangeal joint becomes a problem. The interdigital space narrows, the palm is reduced in width, and the movements of the fingers are joint.
- Splitting of the hand in two The disease is characterized by splitting of the hand into two parts (like a “crab claw”). Often the pathology is bilateral, spreading to the feet.
- Radial clubhand - insufficient development of the radius bone. The defect is visually noticeable due to the inclination of the hand towards the thumb in combination with a shortened forearm. The defect can have varying degrees of severity, up to the absence of bone.
- Ulnar clubhand - underdevelopment of the ulna. A deformity in which the ulna is not sufficiently developed. It has the opposite appearance of radial clubhand: the position of the hand deviates towards the little finger. The pathology is often accompanied by dislocation of the head of the elbow joint. The options described are among the most common. The list of possible deviations in the development of the upper limbs is not limited to them. These descriptions are very brief and are for reference only. Complete information regarding your child’s problem can only be obtained through a consultation with a specialist in our Clinic.
Clinic CONSTANTA. Treatment of syndactyly (fusion of fingers).
Skin rashes in children: rashes, exanthemas, enanthemas
Rashes on the skin (exanthema, exanthema ) and mucous membranes (enanthema, enanthema ) can occur not only with viral and bacterial infections, but also with diseases of a non-infectious nature.
It is important to decide whether these changes represent a primary injury to the child's skin or whether the clinical signs have changed due to secondary factors (infection, trauma, or treatment). Examination by a pediatric dermatologist Moscow - Markushka clinic.
Elements of rashes in a child, children. Primary and secondary elements
There are primary and secondary elements of rashes. Primary elements are classified as roseola, spot, papule, nodule, wheal, vesicle, vesicle, hemorrhage. Secondary elements include pigmentation and depigmentation, scale, crust, erosion, crack, abrasion, ulcer, scar, cicatricial atrophy, lichenification, vegetation.
Primary elements of rashes in a child, children: roseola, spot, erythema, hemorrhage, pinpoint hemorrhages - petechiae, papule, tubercle, node, blister, vesicle, bubble
Roseola is a pale pink or red speck ranging in size from 1 to 5 mm. The shape is round or irregular, the edges are clear or blurred, does not protrude above the skin level, disappears when the skin is pressed and stretched. Roseola occurs in many infectious diseases, especially typhoid fever. Multiple roseola 1-2 mm in size are usually described as a pinpoint rash (with scarlet fever), in the process of resolution they become covered with scales or disappear without a trace.
The spot (makula) has the same color as roseola, size - from 5 to 20 mm, does not protrude above the skin level. The shape is most often incorrect. The spot disappears when pressure is applied to the skin and appears again after the pressure is removed. Multiple spots ranging in size from 5 to 10 mm are described as a small-spotted rash (for example, with rubella - a child is vaccinated against rubella at the Markushka children's clinic). Spots 10-20 mm in size form a large-spotted rash (for example, with measles, allergies - examined by a pediatric allergist in Moscow, Markushka clinic).
Erythema is large areas of hyperemic skin that are red, purple-red, or purple in color. It occurs as a result of the fusion of large spots formed by the dilation of blood vessels not only of the papillary layer of the skin, but also of the subpapillary vascular plexus. Spots larger than 20 mm that tend to coalesce should be considered erythema. Erythema is most typical for erysipelas, thermal, and ultraviolet burns .
Hemorrhage (haemorrhagia) is bleeding into the skin as a result of destruction of skin vessels. It looks like dots or spots of various sizes and shapes and does not disappear when the skin is stretched. The color is initially red, purple or violet, then, as the hemorrhage resolves, it becomes yellow-green and finally yellow (formation of hemosiderin during the breakdown of red blood cells). Color changes are clearly visible in larger hemorrhages.
Pinpoint hemorrhages are called petechiae (petechia). Multiple round hemorrhages measuring 2 to 5 mm are described as purpura . Irregular hemorrhages measuring more than 5 mm are called ecchymoses . Hemorrhages may overlap with other elements of the rash. In such cases, they speak of petechial transformation of roseolas, spots, papules. As a rule, this is observed in severe cases of the disease. Hemorrhagic rashes are detected with typhus (often in combination with roseola - roseola-petechial rash), hemorrhagic fevers, and sepsis. Hemorrhagic elements of irregular shape on a dense basis (stellate rash) are characteristic of meningococcemia and pneumococcal sepsis. Minor hemorrhages can also have a non-infectious origin (capillary toxicosis, toxic-allergic vasculitis, vitamin deficiency C, etc.).
Papule (papula) is an element of the rash that rises above the level of the skin, which is often determined by touch. It has a flat or dome-shaped surface, size - from 1 to 20 mm. The shape and color are the same as those of roseolas and spots. Papules often leave behind pigmentation and flaking of the skin. Papules that merge with each other form plaques, and when the latter merge, areas appear that are located on large areas of the skin, the size of a palm or more. Often, during a routine clinical examination of a child, it is very difficult or even completely impossible to distinguish roseola from papules. On the other hand, the same sick child can simultaneously have roseola, papules (typhoid fever, paratyphoid fever, infectious mononucleosis), papules and spots (measles - child measles vaccination, children's medical).
A tubercle (tuberkulum) is a limited, dense, cavityless formation protruding above the surface of the skin with a diameter of 1-2 to 5-10 mm. The tubercles are formed as a result of the accumulation of a specific inflammatory infiltrate in the dermis. Clinically, the tubercle is similar to a papule, but differs from it in that when palpating the tubercle, a dense infiltrate in the skin is always clearly visible. In addition, tubercles, unlike papules, undergo necrosis during reverse development, often form ulcers and leave behind a scar or cicatricial atrophy of the skin. The tubercles are most typical of cutaneous leishmaniasis, leprosy and tuberculous skin lesions, tertiary and late congenital syphilis.
A node (nodus) is a cavityless, limited compaction that goes deep into the skin, often standing above the skin level. The size of the knots ranges from a hazelnut to a chicken egg and more. They are formed as a result of the accumulation of cellular infiltrate in the subcutaneous tissue and the dermis itself. Inflammatory nodules have a soft or doughy consistency, unclear boundaries, and the skin over them is red. Nodules that appear as a result of specific inflammation (colliquatic tuberculosis, syphilitic gumma) have a dense consistency, are sharply demarcated from the surrounding tissues, and are prone to decay and ulceration with subsequent scarring.
A blister (urtica) is an acutely inflammatory, cavity-free element slightly elevated above the skin level, measuring from 2-3 to 10-15 cm or more, has a round or oval shape, and is often accompanied by itching. Color - from white to pale pink or light red. The blister usually forms quickly and disappears quickly, leaving no trace behind. It occurs as a result of limited acute inflammatory swelling of the papillary layer of the skin and simultaneous expansion of the capillaries. The appearance of urticarial elements is characteristic of allergic reactions of various origins (drug, food, cold allergies), including those of an infectious nature. Sometimes occurs in the pre-icteric period of hepatitis B (vaccination of a child against hepatitis in the Markushka children's clinic).
A vesicle (vesicula) is a cavity element measuring from 1 to 5 mm, representing a detachment of the epidermis. Usually the bubbles are filled with transparent, cloudy or bloody contents, they can shrink and give a transparent or brown crust. If the cover of the bubble is opened, then erosion is formed - a wet surface of pink or red color limited by the size of the bubble. The bubbles do not leave any scars on the skin. If a large number of leukocytes accumulate in a vesicle, it turns into an abscess - a pustule. Inflammatory changes are noted at the base and around the vesicle. Pustules are divided into single-chamber (chickenpox) and multi-chamber (natural smallpox). A group of blisters located on inflamed skin is called herpes. Vesicles are characteristic of herpes and enterovirus infections, chickenpox and natural pox. Chickenpox vaccination - Markushka Children's Clinic.
Bubble (bulla) is a cavity element with a diameter of up to 3-5 cm, located in the upper layers of the epidermis and under the epidermis. The contents of the blisters can be serous, bloody, or purulent. They can collapse, forming a crust, or open up, forming an erosive surface that turns into unstable pigmentation. The bubble occurs more often against the background of an erythematous spot, less often - against the background of unchanged skin (neonatal pemphigoid). The elements can be located both inside the epidermis, in the styloid layer (pemphigus vulgaris), and under the epidermis (multiform exudative erythema, dermatosis herpetiformis). It is observed with bullous form of erysipelas, sometimes with chicken pox, thermal burns.
Secondary elements of rashes in a child, children: hyperpigmentation, depigmentation, scales, erosion, abrasion, ulcer, cracks, tears, crust, scar, lichenification, vegetation
Secondary morphological elements are formed as a result of the evolution of the primary elements of the rash .
Hyperpigmentation (hyperpigmentatio) is a change in skin color as a result of an increase in melanin in it or the deposition of hemosiderin of primary elements.
Depigmentation (depigmentatio) occurs as a result of a decrease in the melanin content in the skin, observed after the disappearance of a nodule, tubercle - resolution of spotty-flaky (pityriasis versicolor, eczematoids) and papular (psoriasis) elements.
Scale (sguama) is an accumulation of rejected cells of the stratum corneum, sometimes the underlying layers of the epidermis. Scales occur on primary morphological elements - papules (psoriasis, syphilis), tubercles, after the resolution of blisters (eczema), etc.
Erosion (erosio) is a skin defect within the epidermis as a result of the opening of a vesicle, blister, or abscess, repeating their shape and size. When vesicles and pustules merge, erosions have scalloped edges. Erosion can also occur as a result of maceration of the skin in the area of folds or during maceration of other elements of the rash, most often papules. When erosion heals, there is no scar left; usually there is only temporary pigmentation.
An abrasion (excoriatio) is a violation of the integrity of the skin that occurs as a result of scratching, scratching, or other damage. Abrasions can be superficial - within the epidermis, sometimes involving the papillary dermis, and heal without a scar. Deeper abrasions, involving the deeper layers of the dermis, leave behind a scar. Abrasions are characterized by a tendency to become infected.
An ulcer (ulcus) is a deep skin defect that reaches the dermis, subcutaneous fat, fascia, muscles, and bones. It occurs as a result of the breakdown of the tissue of the primary element (tubercle, node, ecthyma). Its size is from 1 mm to the size of a coin or palm and more; the shape can be round, oval, linear, oblong, irregular. The surrounding tissue is either inflamed (edema, hyperemia) or infiltrated. Ulcers always heal with the formation of scars.
Cracks, tears (fissura, rhagades) - linear damage to the skin in the form of its rupture, resulting from excessive dryness due to loss of elasticity due to inflammatory infiltration or overstretching of the skin. Cracks can be located within the epidermis and dermis. They are usually localized in the corners of the mouth, interdigital folds, on the palms, soles, above the joints, and in the anus. A superficial crack after healing leaves no traces. After healing of deep cracks, linear scars remain.
A crust (crusla) is formed on the skin as a result of drying of the discharge of a weeping surface (vesicle, vesicle, abscess, ulcer, erosion). The crusts can have different colors (with serous exudate, transparent with a yellowish tint; with purulent exudate, yellow, greenish or brown; with hemorrhagic exudate, brown or black) and shape (layered, oyster-like, etc.).
A scar (cicatrix) is the formation of connective tissue at the site of a deep defect. Occurs after healing of deep skin defects at the site of ulcerated tubercles, deep pustules, nodes, deep burns, wounds. Scar formation is accompanied by the death of sebaceous and sweat glands, hair follicles, blood vessels and elastic fibers, and the disappearance of the skin pattern. Typically, scars are located below the skin level or are at its level, less often they rise above the skin level - hypertrophic scars.
Lichenification (lichenificatio) is a focus of increased skin pattern, accompanied by thickening and compaction, hyperpigmentation, and dryness. Foci of lichenification are most often localized in the neck, elbow and popliteal folds, wrist and ankle joints, inguinal folds, scrotum and occur in chronic dermatoses accompanied by itching (eczema, neurodermatitis).
Vegetation (vegetatio) is a papillary thickening of the skin that occurs as a result of the growth of the styloid layer of the epidermis and papillomatosis of the dermis during a long-term inflammatory process. More often it forms in the area of papular elements and ulcers. Vegetations can erode, bleed, and are prone to secondary infection.
Consultation with a pediatric orthopedist
Treatment of congenital anomalies of the limbs is surgical. Parents should take this issue extremely responsibly, understanding the importance of early seeking medical help. Often, the outcome of treatment is influenced by the age of the child at which the operation was performed and the qualifications of the surgeon. Regardless of the type of congenital defect, medical consultation should be obtained as early as possible, in the first months of the child’s life. At the CONSTANTA Clinic in Yaroslavl you can make an appointment with an experienced hand surgeon, pediatric traumatologist-orthopedist Torno T.E.
During the consultation, the doctor:
- carefully examine the child (pathological changes are noticeable already in the first days of the baby’s life);
- determine the severity of the deformation;
- select the tactics of medical treatment;
- will calculate the exact cost of medical care.
What should parents do?
No matter how harmless the disease may seem, you should not hope that it will go away on its own. A child's body can be very vulnerable and defenseless. Only a doctor can determine why a rash appears on a child’s hands.
.
First of all, you need to visit a pediatric dermatologist
.
- If a child is suspected of having an allergic reaction, a dermatologist may recommend consultation with an allergist.
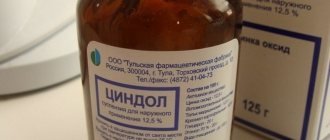
- Under no circumstances should you lubricate your baby’s skin with anything until he has been examined by a doctor. This is especially true for aniline dyes.
- To conduct a complete examination, the doctor at our clinic may prescribe a general blood and urine test, as well as take a skin scraping. It is possible to send skin swabs for bacteriological examination.
You should not try to self-medicate or look for answers on forums on the Internet. No correspondence consultation can be complete or replace a doctor’s examination.
Note to out-of-towners!
You can get medical advice via Skype or email. by mail, having previously sent the necessary photo and video materials to this address (photos of the child’s hands in different projections, a small fragment of video of finger movements).
Information for out-of-town patients
What do we offer our patients?
From the first call from his parents, every little patient finds himself in a Clinic with modern equipment, competent specialists, responsive staff, sincerely interested in the success of treatment.
Accommodation conditions adapted for children
The Clinic's hospital is equipped with everything necessary for the convenience of children. The beds in the wards have functional equipment. Our employees find a special approach to each child, actively communicate with their parents, answering all questions. Specialists closely monitor the baby’s well-being and give detailed recommendations to parents on recovery after surgery. A souvenir of your stay at the Clinic will be a gift from the doctor - a toy.
Possibility of treatment for free and at your own expense
At the CONSTANTA Clinic you can get the necessary medical care:
- For free. The charitable assistance of Rusfond allows us to provide surgical treatment of congenital malformations without payment from the patient.
- At my own expense. The cost of services obtained at your own expense may vary depending on the complexity and scope of the surgical intervention.
Free personal manager services
The personal manager’s assistance includes information support and solving organizational issues that arise during the preparation and process of treating your child. Such support from a Clinic specialist significantly saves time and is provided by us free of charge.
Clinic Constant. Information for parents of young patients
More information for parents of young patients can be obtained by phone.
Anesthesia for operations in children Treatment of children with the support of the Charitable Foundation
Causes of the rash
Most often, rashes on the palms of children are the result of exposure to allergens. The list of allergens is extremely large and is updated from year to year. This could be detergents or chemicals, plant pollen or animal dander. In addition, a rash may appear as a symptom of a food allergy.
Another common cause of a rash on the hands of children can be a bacterial or viral infection. Common examples of such infections include vesicular stomatitis and eczema.
In children of the first years of life, the cause of the rash is often childhood airborne infections. Insect bites can give a similar picture. If the rules of personal hygiene are violated, children often develop a pustular rash of staphylococcal origin - impetigo.
One of the most serious illnesses that debut with a rash on the hands is pseudotuberculosis.
If a rash appears in a child, you should not delay a visit to a specialist. The pediatric dermatologist at our clinic will conduct a thorough and comprehensive examination of the baby and prescribe the most gentle and safe treatment methods.