Eczema is a dermatological inflammatory skin disease, which externally manifests itself in redness of the skin and a rash of fluid-filled blisters. It is because of them that the disease got its name, because translated from Greek ἔκζεμα is a derivative of the word “boil.”
Indeed, redness and rashes on the skin are not an attractive sight, and others begin to avoid a person with eczema. In addition, people are afraid of getting infected - after all, not everyone knows that eczema is safe for them.
What is eczema?
Eczema began to be identified as a separate disease only in the 19th century, but not because it did not exist before. It’s just that the external manifestations of eczema are similar to the symptoms of other skin diseases, and doctors did not have the proper knowledge and experience to distinguish them from each other.
So what is eczema? This is a chronic inflammation of the outer layers of the skin, alternating an acute phase and a period of remission (attenuation of the disease). Eczema is most often observed on the face, hands and feet, but it can develop on absolutely any part of the body.
Redness, swelling and blisters cause the patient to feel severe itching and burning, the affected area of the skin itches, and sometimes becomes painful.
Microbial eczema in pregnant women
Often pregnant women can suffer from dermatosis. Their body undergoes certain changes. The immune system is weakened and hormonal levels are disrupted. There are no particular risks for the fetus or woman. But unpleasant sensations such as itching and a constant desire to scratch create some discomfort. If painful symptoms occur, you should immediately visit a dermatologist.
Methods for diagnosing skin diseases:
- Diagnosis of skin diseases
- Diagnosis of skin diseases at home
- Diagnosis of allergic skin diseases
- Diagnosis of bacterial skin diseases
- Diagnosis of viral skin diseases
- Diagnosis of hair diseases
- Diagnosis of nail diseases
- Diagnosis of skin tumors
- Blisters on the skin
- Dermatoscopy
- Demodex tests
- Diagnosis of sexually transmitted infections
- Mushroom tests
- Skin scraping
Causes of eczema
The true causes of the development of this disease have not yet been clarified. Experts agree that the occurrence of eczema is multifactorial.
Dermatologists believe that eczema is an allergic reaction of the body to a disturbance in its metabolic processes. The driving factor can be a disorder of the endocrine and nervous systems, as well as a person’s genetic predisposition.
Sometimes eczema occurs at the site of long-term non-healing burns and wounds due to microbes developing in it, which provoke an inflammatory process.
The risk of developing eczema increases if you have the following factors:
- lack of vitamins, microelements and unsaturated fatty acids in the body;
- the presence of parasites in the body (worms);
- allergic reaction to food, dust, chemicals, pollen, etc.;
- disturbances in the functioning of the digestive tract;
- inflammation of the gallbladder (cholecystitis);
- dysbacteriosis;
- kidney damage;
- fungal skin diseases;
- hormonal changes in the body;
- chronic infectious diseases;
- immunodeficiency (especially hereditary);
- stress and overwork;
- hypothermia or overheating of the body.
Microbial eczema in children
Infants aged two months to six months, as well as children and teenagers, can develop microbial eczema. Painful signs may appear:
- For hereditary reasons;
- Due to weak immunity;
- For diabetes mellitus;
- In children with a disrupted endocrine system;
- Against the background of ongoing allergic diseases.
The above reasons are associated with hormonal fluctuations. A baby who feeds on mother's milk is not afraid of this disease. Those who are healthy, kept clean, do not suffer from dermatosis.
Types of eczema
Eczema is divided into several forms depending on the course of the disease and the mechanisms of its development.
- True eczema is also idiopathic. There is swelling of the skin and multiple rashes of blisters, which, when bursting, form weeping areas that eventually become covered with a hard crust. The affected skin peels off and itches, but the disease, subsiding, again enters the acute stage.
- Microbial eczema is one that develops on wounds and burns due to inflammation due to the proliferation of microorganisms. Without proper treatment, microbial eczema can greatly increase in size and become a true, chronic form.
- Mycotic eczema occurs when the body has an allergic reaction to fungal infection. To cure such eczema, you must first get rid of the root cause - mycosis.
- Seborrheic eczema develops, as a rule, in patients with seborrhea (dysfunction of the sebaceous glands).
In addition, doctors often distinguish lip eczema (rash of blisters on the lips) and breast eczema in women (redness and blisters observed on the nipples) into separate forms.
How is eczema treated during pregnancy?
Since eczema during pregnancy can have a different course, methods for correcting symptoms are selected individually. The general principle of treatment is to prescribe ointments and other local remedies that will have minimal effect on the woman’s body.
Perhaps, in addition to a dermatologist and gynecologist, you will need to consult other specialists, for example, a gastroenterologist, who will rule out stomach diseases, or an ENT specialist, who will detect inflammation of the ENT organs. This is explained by the fact that the cause of exacerbation of eczema may be another disease. Taking this into account, as well as taking into account the gestational age and symptoms, the doctor selects how and with what to treat eczema during pregnancy.
Hormonal drugs
You can use hormonal ointments only as prescribed by a doctor. Such drugs can have a negative effect on the fetus. For this reason, they are not used in the first trimester of pregnancy. Most hormonal ointments are allowed from 12-16 weeks and provided that the potential benefit to the woman is greater than the risk to the fetus. This can only be assessed by a specialist who will take into account the ability of a particular drug to penetrate the placenta and its effect on the tone of the uterus.
They try to prescribe hormonal ointments for eczema during pregnancy in extreme cases, when normalization of the diet and non-hormonal remedies have not produced results. Another rule is to use such serious drugs in short courses and only topically, that is, for treating the skin and not for oral administration.
Non-hormonal drugs
In most cases, treatment of eczema in pregnant women occurs with the use of non-hormonal ointments, which have a gentle effect on the woman’s body, helping to eliminate inflammation and unpleasant symptoms. Among such drugs are Bepanten, Elidel, and Zinc ointment.
At the PsorMak clinic, for treatment they use a non-hormonal ointment based on plant components, developed according to the original method of Dr. V. F. Mak, who has more than 25 years of experience in dermatology. The unique treatment method has already helped hundreds of patients, as can be seen by studying their reviews and treatment results. Herbal ointment does not irritate the skin and does not aggravate the course of the disease, but gently relieves redness, inflammation, itching and other unpleasant symptoms of eczema.
Diet and prevention
In order not to provoke an exacerbation of eczema, a woman needs to follow a diet. It is healthy to eat a lot of vegetables and fruits, fresh herbs, cereals, lean meats, and dairy products. Must be avoided:
- baking,
- chocolate,
- citrus fruits,
- nuts,
- whole cow's milk,
- seafood,
- red vegetables and fruits,
- honey
Your home should be free of any allergens, such as feather pillows or carpets, that may harbor mites. It is necessary to have less contact with household chemicals - carry out cleaning and wash dishes using gloves. Clothes should be made from soft natural fabrics with a small content of viscose, without synthetics and wool.
It is equally important to maintain the correct daily routine, avoid stress, relax and spend more time in the fresh air.
And the most important thing is not to self-medicate, but at the first unpleasant symptoms, immediately consult a doctor so as not to aggravate the disease and cope with it faster through timely measures taken. If you encounter eczema during pregnancy, contact the PsorMak clinic, where you can be diagnosed and receive the correct treatment. November 5, 2021
Author of the article: dermatologist Mak Vladimir Fedorovich
Bibliography
- Akhtyamov, S.N. Practical dermatocosmetology / S.N. Akhtyamov, Yu.S. Butov. M.: Medicine, 2003. - 391 p.
- Arkhangelskaya, E.I. Materials on the clinic, etiology and pathogenesis of diffuse streptoderma and microbial eczema: abstract. dis. Dr. med. Sciences / E.I. Arkhangelskaya. L., 1973. - 38 p.
- Aizikovich, JI.A. Abstracts of scientific works of the VIII All-Russian Congress of Dermatovenerologists / JI.A. Aizikovich, T.V. Sokolova. 4.1. // Dermatology. - 2001.- P. 205.
- Buxton, P.K. Dermatology / P.K. Buxton. M.: Publishing house BINOM, 2005, - 175 p.
- Belousova, T.A. Neurogenic factors in the pathogenesis of eczema: abstract. dis. . Ph.D. honey. Sciences/T.A. Belousova. M., 1984. - 18 p.
- Demidova, M.A. Epidemiological and pharmacoeconomic aspects of the use of antihistamines in the treatment of patients with eczema / M.A. Demidova, E.V. Bogdanova // Ross. magazine skin and venereal diseases. 2009. - No. 2. — P. 46-49.
- Kudryavtseva, E.V. Lokoid and modern approaches to external therapy of atopic dermatitis / E.V. Kudryavtseva, AB Karaulov // Immunopathology, allergology, infectology. 2003. - No. 4. — P. 57-62.
- Mikhailenko, A.A. Allergy and allergic diseases /AA Mikhailepko, G.A. Bazanov. M.: Med. information agency, 2009. - 304 p. thirty.
- Prokhorenkov, V.I. Eczema / V.I. Prokhorenkov, T.A. Yakovlev 3rd ed. - Krasnoyarsk: PIK "Offset", 1994. - 255 p.
results
Eczema is an acute or chronic allergic recurrent inflammatory skin disease caused by various exogenous and endogenous factors, characterized by a polymorphic rash caused by serous inflammation of the skin, polyvalent sensitization and severe itching [9, 10].
Classification of eczema
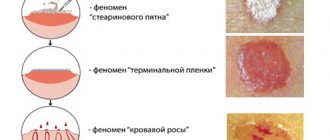
. There is no generally accepted classification of eczema. Based on clinical manifestations, domestic dermatologists distinguish the following forms of eczema: true (pruriginous, microbial, dyshidrotic), seborrheic, horny (tilotic), childhood and occupational. Varieties of M.E. are coin-shaped (nummular or plaque), paratraumatic, mycotic, varicose, sycosiform and eczema of the nipples and pigment circle in women [9, 10]. In accordance with the Federal Clinical Guidelines for the Management of Patients with Eczema (2016), all of them, regardless of the form, are encrypted as L.30 [10]. However, this section contains only L.30.0 - coin-shaped eczema; L.30.1 - dyshidrosis; L.30.2 - skin autosensitization; L.30.3 - infectious dermatitis; L.30.4 - erythematous intertrigo; L.30.5 - pityriasis white; L.30.8 - other specified dermatitis; L.30.9 - dermatitis, unspecified. This significantly complicates the statistical accounting of the occurrence of various clinical variants of eczema. Some authors designate ME as “infectious eczema” [11], which according to ICD-10 probably corresponds to infectious dermatitis (L.30.3). But there are significant differences in the pathogenesis of eczema and dermatitis. Depending on the duration of the disease, acute (up to 3 months), subacute (3-6 months) and chronic (more than 6 months) stages of the disease are distinguished [12] (Fig. 1).
Rice.
1. Stages of microbial eczema. a - acute; b - subacute; c - chronic. Foreign authors identify true eczema with atopic dermatitis (atopic eczema), although these nosological forms have clear differential diagnostic criteria. Eczema also includes nummular, vesicular palmoplantar eczema and autosensitizing dermatitis [13]. The first two types of eczema actually correspond to microbial and dyshidrotic eczema. Returning to the traditions of domestic dermatology, in Russia all scientific publications on ME are based on the clinical forms accepted in our country.
Pathogenesis of microbial eczema
. The etiopathogenetic aspects of ME, according to scientific research, are multifaceted. However, the mechanisms of development of immune abnormalities in the body as a whole and directly in the skin of patients have not been fully established, so an integrated approach to studying the pathogenesis of eczema is necessary [14-16]. Eczema, including ME, is formed under the influence of immunological, neuroendocrine, metabolic, infectious-allergic, vegetative-vascular, hereditary and other factors [9, 17-21]. The predominant significance of certain endogenous and exogenous influences is ambiguous, therefore it is generally accepted to consider ME as a polyetiological disease.
The role of the skin barrier in the pathogenesis of microbial eczema.
Intact skin protects the human body from the penetration of infectious pathogens. This is due to the tight adhesion of horny scales, acidic pH (4.5-5.3), fatty acids of sebum, the synthesis of some interleukins in the epidermis, as well as the biological balance and antagonistic interaction of pathogenic, conditionally pathogenic and non-pathogenic microflora [4] . Changes in the structure of the stratum corneum lead to increased skin permeability to fungi and bacteria [22]. A shift in the pH of the epidermis to the alkaline side leads to increased desquamation of corneocytes, disruption of the formation of lamellar bodies, causes thinning of the skin and slows down the restoration of the skin barrier. In general, post-inflammatory epidermal barrier deficiency may be due to involucrin deficiency leading to impaired corneocyte cohesion; lack of natural moisturizing factors that promote dehydration and lipids of the stratum corneum; genetically determined filaggrin deficiency [23]. Microbial allergens have pronounced antigenic activity and cause and maintain immune inflammation. Violation of the integrity of the skin when scratching it due to itching forms an entry point for infection. Exudation that accompanies eczema promotes the concentration of proteins on the surface of the skin and creates favorable conditions for the proliferation of secondary infections [4].
The state of the skin microbiota in patients with microbial eczema.
In recent years, more and more attention has been paid to studying the state of the skin microbiota in ME patients [21, 24—26]. In a healthy person, the microflora takes part in the implementation of the protective function of the skin by suppressing pathogenic microorganisms with non-pathogenic ones [27]. Species and quantitative changes in the composition of normal skin microflora can be accompanied by both the development of the disease and the manifestation of diseases that occur subclinically [28, 29].
, Staphylococcus
aureus
is sown in 80% of cases
S. haemolyticus
in 14% , and non-lipophilic yeast fungi, mainly of the genus
Candida
spp., in 40.7%.
[24]. A study carried out 10 years later in Moscow also established the predominance of gram-positive coccal microbiota, represented mainly by Staphylococcus
spp.
(64.3%) and Streptococcus
spp
.
(33.3%) [21].
The authors also established the presence of S. aureus
(33.3%),
Klebsiella pneumoniae
(19.8%),
and Proteus vulgaris
(16.7%) in the nasopharynx.
Infectious pathogens with a lower frequency were also sown in the discharge of the urogenital tract and when examining stool for dysbacteriosis. The predominance of coccal microflora in lesions in ME is evidenced by the results of studies performed in Samara [25]. Staphylococci were cultured in 96.7% of patients. species composition was represented by: S. aureus
(65%),
S. epidermidis
) ,
S. saprophytes
(3.3%).
was cultured in 13.4% of patients .
In isolated cases,
Propionibacterium ,
Corinebacterium
(
5% each) and
E. coli , Proteus
,
Klebsiella
(3.3% each).
It is significant that in 2/3 (66.7%) of cases the growth of a monoculture was registered, and in 1/3 (33.3%) - an association of 2-3 microorganisms. , S. aureus
predominated in the lesions 1535.6±41.8 and 1682.2±52.6 CFU/ml, respectively). On externally unchanged skin, its population was significantly smaller (403.0±36.4 and 515.8±61.0 CFU/ml) [11].
Quantitative differences in the species composition of skin microbiota pathogens in ME patients with acute and chronic disease were identified when compared with healthy people [26]. The level of total density of microorganisms on inflamed areas of the skin during the acute course of the process was 38 times higher than on externally unchanged skin (1562±14.9 CFU/cm2 versus 41.2±6.1 CFU/cm2); in the chronic course of the disease, this indicator differed by 21 times (1562±14.9 CFU/cm2 versus 75.2±8.2 CFU/cm2). Compared to healthy individuals (3.6±0.5 CFU/cm2), the differences were already 434 and 20.9 times, respectively. The structure of the microbiota was sharply dominated by gram-positive microorganisms, the density of which in the lesions during the acute process was 10 times higher than during the chronic process (221.2±2.0 CFU/cm2 versus 22.0±4.1 CFU/cm2) and significantly higher than in the same patients on unchanged skin (132.1±1.4 and 14.7±0.2 CFU/cm2, respectively). And when compared with healthy people (0.7±0.1 CFU/cm2), this indicator differed by 315.7 and 34.4 times, respectively. Total density of pathogens of the genus Staphylococcus
spp.
during an acute process on the affected areas of the skin was 37.1±2.6, which was significantly higher than on externally unchanged skin (24.8±2.9 and 16.1±1.8 CFU/cm2, respectively). Compared to healthy individuals, with ME in lesions these indicators were 17.7 and 11.2 times higher. At the same time, the density of yeast-like fungi of the genus Candida
spp
.
was higher in chronic ME compared to acute ME (5.7±0.4 CFU/cm2 versus 3.1±0.2 CFU/cm2) and differed by 28.5 and 15.5 times compared with that in healthy individuals (0.2±0.01 CFU/cm2).
In a chronic process, the contamination of affected and apparently unchanged areas of the skin with Candida
spp. was almost identical.
Immunoallergic concept of the development of microbial eczema.
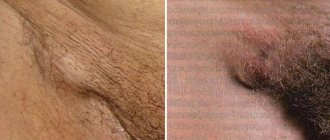
Leading in the pathogenesis of ME are infectious allergens - bacterial, viral, fungal, protozoal, etc. [12, 30-33]. The disease can also be provoked by exogenous stimuli - physical, mechanical and biological. The immunoallergic theory is clearly confirmed by the empirically identified stages of the course of M.E. Initially, the disease develops in the form of eczematization at the site of non-allergic banal pyodermitis, and then through eczematids and localized forms it is transformed into a generalized process [34, 35]. Foci of M.E. often occur in places of long-term persistent pyoderma (Fig. 2) and around purulent wounds (Fig. 3, a, b, c), when scratching scabious lymphoplasia of the skin (Fig. 4) [34, 36-38]. ME is a complication of dermatophytosis of large folds and feet (Fig. 5), superficial skin candidiasis (Fig. 6), and develops against the background of a varicose symptom complex [9, 39-41] (Fig. 7). Initially, sensitization may be monovalent in nature, but over time it becomes polyvalent [3]. The pathogenesis of ME is shown in Fig. 8.
Rice. 2. Microbial eczema at the site of persistent staphylococcal impetigo.
Rice. 3. Paratraumatic microbial eczema. a - at the site of intramuscular injection of calcium chloride; b - at the site of a thermal burn; c - around the fistula opening in osteomyelitis.
Rice. 4. Microbial eczema at the site of scabious lymphoplasia of the skin in the elbow area.
Rice. 5. Mycotic eczema, complicating dermatophytosis of large folds and feet.
Rice. 6. Mycotic eczema, complicating superficial skin candidiasis (absence of eponychium is a diagnostically significant symptom).
Rice. 7. Varicose eczema (a, b), a combination of varicose and mycotic eczema (c).
Rice.
8. Scheme of the pathogenesis of microbial eczema. In the pathogenesis of ME, a decisive role is played by bacterial sensitization with the leading role of S. and ureus
and
St. _ hemolyticus
[30, 41, 42]. Sensitization to these allergens is characterized by an increase in the frequency and severity of an immediate-type hyperergic reaction (IHT) and a decrease in these indicators for a delayed-type hyperergic reaction (DTH). On the one hand, the possibility of activation of ME due to the persistence of bacterial microflora in foci of chronic infection in other organs and systems of the body (nasopharynx, tonsils, gastrointestinal tract, hepatobiliary system, reproductive system, etc.) cannot be ruled out. Foci of chronic infection occur in 65.3% of ME patients [30]. On the other hand, the presence of a deficiency of cellular and humoral immunity in ME patients contributes to the formation of foci of chronic infection and persistence of predominantly pathogenic microorganisms on the skin [43].
The data obtained are clear evidence of the need to use topical drugs with a wide spectrum of antimicrobial activity for ME.
A comprehensive assessment of immunological disorders in ME revealed changes in many indicators of the cellular, humoral and cytokine components of the immune response (Table 1).
Table 1. Changes in indicators of immune status in patients with ME
Patients with ME develop an immunologically determined, latent syndrome of endogenous intoxication, which manifests itself clinically as a complex of nonspecific symptoms. An increase in the concentration of circulating immune complexes (CIC) and the value of the leukocyte intoxication index (LII) is directly proportional to the intensity of immunopathological processes. The clinical form of ME, the prevalence of rashes, and the duration of exacerbation are directly dependent on the severity of immunological changes and endotoxemia. The key indicator of endotoxemia is the content of IgG, IgG2 in the bloodstream. A decrease in the expression of TLR2, TLR4 and TLR9 on blood cells is observed as the severity of the disease increases, which is often accompanied by the development of clinically severe forms of dermatosis. A decrease in the level of antimicrobial peptides in the blood serum of patients correlates with the duration and severity of the eczematous process. During an acute process, the level of CD14+DR+ monocytes increases, and during an exacerbation of the chronic process, their decrease occurs. An increase in IL-2 concentration indicates an active acute inflammatory process. Increased levels of IL-17 and interferon-γ (IFN-γ) are associated with the development of allergic inflammation and protection against infection. IFN-γ ensures the launch of a cytokine cascade aimed at the formation of a focus of inflammation with the involvement of effector cells. A decrease in the level of lactoferrin in the blood serum indicates the activation of a bacterial infection.
These studies indicate that for topical treatment of ME, drugs with a pronounced anti-inflammatory effect should be used. These drugs include topical corticosteroids (TCS), which have taken one of the leading positions in the treatment of steroid-sensitive skin diseases. Currently, dermatologists prescribe them 3.9 times more often than doctors of other specialties. ME belongs to the group of dermatoses for which TCS therapy is pathogenetically justified and used in combination with drugs from other groups. TCS is an etiotropic and pathogenetic therapy in cases where the basis of the disease is inflammation in the skin, especially immune-mediated. TCS have anti-inflammatory, antiallergic, vasoconstrictor and immunosuppressive effects. They regulate the immune response by reducing the number of lymphocytes, inhibiting T lymphocytes, increasing apoptosis of T and B lymphocytes, inhibiting the formation of immune complexes and reducing the activity of the complement system. This leads to inhibition of the hyperreaction of the immune system upon contact with the antigen. At the same time, without local and externally controlled immunosuppression, it is impossible to achieve the required effectiveness of the drug against hyperimmune allergic dermatoses. On the other hand, the presence of an immunosuppressive effect excludes the possibility of using single-component TCS in the treatment of dermatoses combined with infectious pathological processes. Compared to traditional means for external therapy, TCS have significant advantages and suppress all the main components of allergic inflammation. The infectious process should be stopped by prescribing combined TCS. Taking into account the biorhythm of cortisol production in the body and the rhythm of epidermal proliferation, TCS should be used in the morning to enhance the anti-inflammatory effect, and in the evening for the antiproliferative effect [23].
The role of yeast-like fungi of the genus
Candida spp .
in the pathogenesis of microbial eczema.
Candida
can be causative allergens . [3, 45-47]. The widespread use of antibiotics, corticosteroids, and hormonal contraceptives has contributed to the interpretation of candidiasis as one of the serious infectious complications of drug therapy [48, 49]. With M.E. Antibiotics form the basis of traditional treatment regimens, often in the form of repeated courses [10, 50]. The reasons for prescribing antibiotics to patients with ME are traditional treatment regimens, sanitation of foci of chronic bacterial infection in various organs and secondary pyoderma on the skin. Candidiasis of the skin and mucous membranes as infectious complications of antibacterial therapy in our practice was registered in 85% of patients with ME [42]. This high frequency is due to the fact that patients who had been receiving traditional therapy for a long time, including repeated courses of antibiotic therapy with various drugs without antimycotic support, came for consultation with the professor. Complications from the use of antibiotics are numerous and affect the course of ME [1].
Yeast-like fungi of the genus Candida
spp.
belong to opportunistic microorganisms and can induce the formation of HNT in 62.3–78% of patients with ME [30, 33]. skin testing has shown that in patients with ME there is a change in skin reactivity to S. aureus , St. _ hemolyticus , C. albicans
.
The frequency and size of the wheal increases with HNT and the frequency and average size of papules decreases with HRT [30, 41]. Micromycetes Candida
spp., being typical pathogens of opportunistic infections, exhibit their pathogenic potential under the condition of disturbances in the host's antimicrobial resistance system. They complicate the underlying pathological process, causing resistance to therapy and drug intolerance [48].
Allergenic effect of S. and ureus
and
C. _ albicans
in ME are significantly enhanced under conditions of mixed infection.
The synergism of bacterial and yeast microflora in various pathological conditions and in ME has been clinically and experimentally proven [41, 51, 52]. Pathogens of bacterial microflora during associated infection are often characterized by antibiotic resistance, lysozyme, adhesive, hemolytic, lecitellase, and DNA activities [52]. Colonization of the pharynx and nose simultaneously with S. aureus and Candida
spp.
with ME leads to a more severe course of the disease and chronicity of the process. The index for assessing the severity of ME in the presence of candidiasis is significantly higher than in its absence (23.4±7.7 points versus 13.1±4.4 points). The continuous course of the disease is recorded 2.2 times more often, and candidamycids often appear (23%) [42]. response in the form of specific IgM antibodies and IgG antibodies to C. albicans
is registered in 81.2% of patients.
The absence of mannan antigen, the main protein of the cellular machine C, . albicans
is direct evidence of the presence of non-invasive candidiasis and justifies the advisability of using topical antimycotics [33].
The data obtained indicate the advisability of examining patients for the presence of yeast-like fungi of the genus Candida
spp., using clinical and laboratory data for this purpose (Fig. 9).
If Candida
spp. is detected. Specific therapy should be carried out using combination drugs with antimycotics, and in their absence, a course of preventive therapy.
Rice.
9. Scheme of examination of a patient with microbial eczema to identify superficial candidiasis of the skin and/or mucous membranes. Diagnosis of ME is based on the history and clinical picture of the disease. According to indications and for the purpose of differential diagnosis, laboratory tests are prescribed. The most significant are a clinical blood test and an enzyme-linked immunosorbent assay (ELISA) for determining antibodies to antigens of yeast-like fungi of the genus Candida
spp.
,
Giardia, Ascaris, Opisthorchia, Toxocara and others. If candidiasis is suspected, a bacterioscopic examination of the throat, nose and genitals for the presence of pseudomycelium is initially carried out. Its presence is a key mechanism in the pathogenesis of candidiasis. It is advisable to conduct a cultural study of scrapings from lesions on the skin, throat, nose, and genitals to identify bacterial microflora, yeast microflora and determine its sensitivity to antibacterial and antimycotic drugs.
Prevention
For prevention, two types of care products are used.
- Moisturizing products with powerful emollients, such as urea and glycerin, soften and prevent the body from drying out due to the fact that, distributed in the outer layers of the epidermis, they attract moisture. They are applied throughout the day as needed.
- Natural oils, waxes and silicones create a protective barrier on the surface of the skin, preventing moisture evaporation. They are best used after a shower and applied to a damp area of the body.