Skin diseases are accompanied not only by pain and severe discomfort, but also by the risk of unaesthetic scars or scars appearing on the skin. Therefore, it is extremely important to promptly contact a dermatologist who can diagnose the disease at an early stage and prescribe effective therapy. Our medical center provides the opportunity to receive qualified medical care, as a result of which it is possible to accurately diagnose and eliminate signs of skin damage. One of the most common problems with which patients come in this direction is demodicosis. This is a rather dangerous and problematic pathology, which is almost impossible to cope with on your own.
What is this?
Demodicosis in humans develops as a result of reproduction in the hair follicles, sebaceous glands of the skin and meibomian glands of the iron mite (Demodex). The breeding ground for the development of this parasite is sebum, so its main habitat is the skin of the face and external ears. But with a complicated course and lack of timely treatment, the skin of the chest and back is involved in the pathological process.
It is important to understand that healthy people can also be carriers of such a tick, since it is a representative of normal microflora. According to official statistics, about 60% of people are infected with Demodex, but not everyone develops this parasitic disease. Demodicosis of the body develops with the slightest disturbance of the biocenosis and a drop in immune defense.
Practical use
Trichopolum is applied to the affected areas with light movements, gently rubbed until completely dry. It is often recommended to apply the medicinal composition twice a day. The exact dosage is determined by the doctor, based on the results of the examination and the complexity of the pathological process. The composition is applied in a thin layer; using a large amount leads to an overdose, which causes side effects.
After rubbing, the components penetrate into the body and are quickly absorbed. It penetrates into the plasma and organs. The maximum concentration is observed after 2 hours.
Order an antiparasitic drug directly from the manufacturer
As a result of treatment, complications such as cystitis and other pathologies are possible.
Causes of demodicosis
As mentioned above, the main reason for the development of this disease is the active reproduction of the iron mite. There are several possible reasons that can lead to increased activity of these opportunistic microorganisms. These are internal and external factors. The first category includes:
- A significant drop in immune defense and exhaustion of the body caused by poor nutrition, autoimmune pathologies, previous diseases, constant stress, etc.;
- Viral and microbial diseases that occur in chronic forms (hepatitis, tuberculosis, etc.);
- Helminthiases. The vital activity of helminths contributes to the weakening of the immune system;
- Malignant neoplasms. With many types of oncology, the body becomes exhausted, making it more difficult for it to cope with infections;
- Damage to the gastrointestinal tract. There is a proven relationship between the bacterium Helicobacter pylori and demodicosis;
- Other skin diseases. These are seborrheic dermatitis, rosacea, acne, etc. In the presence of inflammatory processes or integrity disorders on the skin, the risk of pathogenic activation of opportunistic flora increases significantly;
- Hormonal imbalance associated with illness or natural condition (for example, pregnancy or breastfeeding).
Skin demodicosis can also develop as a result of exposure to unfavorable external factors. As a rule, they are combined with internal ones, but in some cases (for example, choosing the wrong skincare products) they can be the main etiology. Among them:
- Temperature effect. This parasite multiplies especially actively in warm conditions;
- Unhealthy Lifestyle. This includes poor nutrition, frequent stress and bad habits;
- Use of low-quality cosmetics for care. This is especially true for cosmetics that do not have quality certificates and do not meet legal requirements;
- Poor environmental conditions. High levels of environmental pollution lead to a weakening of the barrier function of the skin.
Demodectic mange symptoms
Due to the fact that this disease can affect different areas of the skin, the clinical picture differs. In the cutaneous form, the following signs of demodicosis appear:
- Acne of varying severity: from small nodules and ulcers to rosacea;
- A strong tooth that causes discomfort. In most cases, it intensifies in the evening and night;
- Excessive sebum production. It is the greasy environment that is most nutritious for ticks of this genus;
- Red spots that are a symptom of high blood pressure in the blood vessels. This indicates the presence of an inflammatory process in the body;
- Nose enlargement. If you contact a dermatologist late or in the absence of adequate treatment, it is possible to replace the functioning tissue with connective tissue.
Demodicosis of the eyelids and eyes, in turn, manifests itself as follows:
- Clumping of eyelashes. Along their growth line, a thin layer of film is formed that has adhesive properties;
- Redness of the eyelids as a result of the inflammatory process;
- Tired eyes. This symptom occurs due to inflammation and due to the fact that the patient is forced to strain his vision;
- Eyelash loss caused by damage to hair follicles.
3.Diagnosis of the disease
After a visual examination and conversation with the patient, the dermatologist prescribes a microscopic examination
.
Material for analysis is taken by scraping the epidermis from the affected areas of the skin. It is also recommended to analyze eyelashes
taken from different parts of the eyes. Express analysis makes it possible to get instant results. During the study, adult ticks, their eggs and shed chitinous shells are discovered. In order for the dermatologist to see a complete picture of the density of mite colonization of the skin, it is recommended not to wash your face for 24 hours before the examination. What is important for making a diagnosis in this case is not the fact of detecting a tick in itself, but the number and activity of the parasite, as evidenced by the number of larvae and eggs.
About our clinic Chistye Prudy metro station Medintercom page!
Diagnostics
Demodicosis on the face and skin is diagnosed by a dermatologist. If the disease is secondary and has developed against the background of the underlying disease, then doctors of other specialties (gastroenterologist, gynecologist, trichologist, endocrinologist, etc.) may be involved for diagnostic and therapeutic purposes. For diagnosis, first of all, visual inspection is used. The doctor evaluates the condition of the skin, eyes and affected areas of the body. In addition, eye biomicroscopy and laboratory examination methods are practiced. The most informative of them are:
- Slit lamp biomicroscopy of the eye is a non-invasive examination aimed at looking for active inflammation. This is an absolutely painless manipulation that does not require special preparation;
- Eyelash test - involves taking freshly removed eyelashes (4 from each eyelid) for further examination under a microscope. Using this method, it is possible to determine the number of parasites (the presence of more than 1 mite on 2-4 eyelashes is pathogenic). This is also a painless procedure, but before it is carried out it is necessary to abandon decorative and skincare cosmetics for several days;
- Biopsy. This is the most informative diagnostic method, but the most traumatic. Diagnosis is carried out under local anesthesia using a tubular knife or scalpel. The taken biomaterial is fixed in a formaldehyde solution for a day and treated with dyes. This makes it possible to fully visualize the gland and adjacent tissues with the pathogenic mite.
Classification
Demodicosis (photo can be found below) is classified into 2 main clinical forms - primary and secondary. The first diagnosis is made in the event of a sharp surge in parasitic reproduction and effective treatment with the use of antiparasitic drugs. In most cases, it occurs in people over 40 years of age. The secondary form is diagnosed by identifying concomitant skin lesions and systemic diseases (usually associated with immunodeficiency). In some cases, this diagnosis is found in people taking epidermal growth factor receptor inhibitors and in those who have been exposed to ultraviolet radiation.
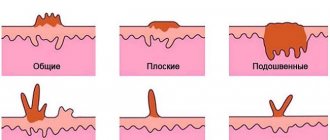
Based on the symptoms manifested on the skin, the following types of demodicosis are distinguished:
- Acneiform - the presence of papules and pustules similar to acne;
- Rosacea-like - papules appear due to diffuse erythema;
- Seborrheic - skin rash combined with peeling;
- Ophthalmic - inflammation of the eyelids, accompanied by discomfort in the affected eye.
Contraindications and side effects
Before applying the cream, you must take into account that it does not combine well with alcohol. Also, it should not be used in the presence of such deviations and pathologies:
- period of pregnancy and lactation;
- liver and kidney pathologies;
- intolerance to some components that make up the product;
- central nervous system dysfunction;
- leukocytosis;
- taking certain medications.
If the course is violated, the following complications are possible:
- skin hypothermia and itching;
- changes in plasma composition;
- lack of coordination;
- dizziness;
- dryness and vision impairment;
- drowsiness;
- lethargy;
- stomatitis;
- pancreatitis at the initial stage;
- nausea;
- dyspepsia.
If such manifestations occur, then you should consult a specialist. You may need to select another course using substitutes.
Order an antiparasitic drug directly from the manufacturer
Complications of the disease
Treatment of demodicosis on the face should be carried out exclusively with the assistance of a doctor. Self-medication or ignoring this problem may not only not bring the desired result, but also worsen the course of the pathology. Skin scratching and regular trauma to the skin (due to severe itching and the patient’s desire to remove the rash mechanically) lead to disruption of the barrier function. As a result, the risk of developing a pustular infection significantly increases, which can be diffuse and affect large areas of the body.
In addition, this disease (especially demodicosis on the face in women) leads to psychological problems. As a result of the appearance of visible defects, the patient becomes withdrawn, begins to feel embarrassed about his appearance and stops leading a full-fledged lifestyle (closes himself off from the outside world, stops communicating with people, prefers to be alone). As this problem worsens, the developed complexes can develop into psychoses, neuroses and prolonged depression.
A large number of people with this diagnosis have concomitant pathologies (gastrointestinal tract, endocrine glands, etc.) and chronic infectious foci. Demodicosis damage to the body contributes to the aggravation of these conditions and, accordingly, deterioration of well-being.
Trichopolum ointment
Since we are talking about skin lesions, treatment of demodicosis is not possible without topical application. The optimal solution would be Trichopolum ointment. It easily copes with ticks and their larvae. To ensure the effectiveness of the course, you must take the medicine as prescribed by your doctor. It is important to take into account a number of factors.
Do not forget that treatment is carried out not only locally, but also with drugs for internal use. This is the only way to solve the problem in a fairly short time.
Skin demodicosis
The transmission route is contact or contact-household. Can be transmitted through contaminated clothing, bedding, contaminated hands and more. Demodex is distinguished by its survivability under comfortable conditions that correspond to the daily life of most people. The parasite remains viable at a temperature of 17-20°C for 10 days or more, and in an aquatic environment at a temperature of 12-18°C for 3 days. When water is heated to 50° C, the microorganism dies within one minute, and at low temperatures it dies immediately.
To date, there is no single theory explaining the etiology of the development of the inflammatory process and the active reproduction of mites. But there are several predisposing factors that can provoke these processes:
- Excessive sebum production;
- Improper skin care, abuse of cosmetics (especially low quality);
- Long-term use of external corticosteroids;
- Poor nutrition (abuse of sugar, soda, spicy foods, coffee, alcoholic drinks);
- Concomitant gastrointestinal diseases;
- Reduced immunity;
- Hormonal imbalance, excess weight;
- Psychological problems, frequent stress.
Reviews
Trichopolum was used in the treatment of trichomoniasis, which was diagnosed several years ago. Gauze swabs lubricated with the product were inserted into the vagina. Often the procedure was carried out in the evening, before bed. A month later, the results showed that the disease had subsided.
Order an antiparasitic drug directly from the manufacturer
Marina, 32 years old
For a long time I struggled with acne and pimples. All to no avail. Everything changed after using Trichopolum. A few weeks later I forgot about these problems. In addition to acne and rashes, the ointment helps solve the problem of blackheads.
Alina, 28 years old
A few months ago I was diagnosed with demodicosis. After consultation, the doctor prescribed a comprehensive treatment, which included the use of Trichopolum. The procedure is very easy. First, the face is cleaned, after which a mask is applied. After a few days, the manifestations of the pathology became less noticeable.
Arthur, 36 years old
Demodectic mange of the eyelids
Treatment of demodicosis of the eyelids requires a comprehensive approach and qualified medical intervention. Demodectic blepharitis is a chronic disease that occurs with periodic exacerbation and remission. It has the following clinical picture:
- Severe eye fatigue associated with the need to strain to better focus on an object or letters;
- Intense itching in the eyelashes and eyebrows. Often this symptom intensifies with external exposure to heat, in the evening and at night;
- Foreign body sensation, burning and tingling that does not go away after washing or scratching;
- Sticky discharge from the eyes after waking up;
- Accumulation of foamy contents in the eye corners;
- Hyperemia, swelling and thickening of the eyelids (especially at the edges).
- The chronic form of demodectic blepharitis can be complicated by keratoconjunctivitis, keratitis and dry eye syndrome. Therefore, it is strongly recommended to consult with an ophthalmologist at our clinic, who will be able to prescribe preventative and therapeutic therapy aimed at maintaining eye health.
Therapy
Treatment measures are carried out over a certain period. This is due to the fact that parasite larvae sometimes lie quite deep, which protects them from negative external factors. As a result, the effectiveness is somewhat reduced, which requires long-term therapy. The course is based on the use of 250 mg tablets three times a day.
Order an antiparasitic drug directly from the manufacturer
Treatment for demodicosis is prescribed by a doctor, based on the indications and complexity of the pathology. On average, the course lasts no more than three weeks. If necessary, it is repeated after a week's rest. Using the medicine allows you to achieve the following goals:
- reduce swelling;
- strengthen the immune system;
- relieve inflammation.
Together with Trichopolum, you can use local gels and ointments. The exact dosage regimen is determined by the doctor. This takes into account a number of factors that may affect the final result. It is also important to observe the dosage and duration of the course.
Available in various forms
Demodicosis of the ear
This pathology does not always stop at the face. In advanced cases or in the absence of timely treatment, it spreads to neighboring areas of the body, including the ears. In such a situation, it will not be possible to quickly get rid of demodicosis, especially without medical help. Damage to the auricle is accompanied by the following clinical symptoms:
- Intense itching and irritation of the skin. As a result of constant scratching, bruises and microtraumas appear;
- Hyperemia and swelling of the ear, indicating an inflammatory process;
- The presence of red rashes of varying sizes and quantities;
- Pain upon contact with the skin (often a consequence of a violation of the barrier function of the tissue).
Demodicosis of the head
Ticks of the genus Demodex are representatives of opportunistic microflora of the skin on the body, including the head. They are present in almost all people on the planet. In everyday life, their activities do not cause visible discomfort; they exist in a mutually beneficial relationship with humans, fighting harmful microorganisms. But when the immune defense drops and unfavorable conditions set in, the parasites begin to multiply uncontrollably, as a result of which their numbers increase greatly, and the vital activity of these parasites becomes noticeable. This situation can result from:
- Hormonal imbalance;
- Long-term use of antibacterial and hormonal medications;
- Poor nutrition;
- Abuse of saunas, steam baths and solariums;
- Using low-quality cosmetics to care for skin and hair (since demodicosis needs to be treated comprehensively, our clinic specialists help patients choose the right and safe care products);
- Failure to comply with simple hygiene rules.
Demodicosis treatment
The treatment regimen for demodicosis is a set of measures aimed at eliminating external symptoms and the cause that provoked them. The final stage of therapy is the use of preventive measures that help consolidate the therapeutic result and prevent relapse of the disease. It is important to understand that it is almost impossible to cope with this problem on your own. This problem requires qualified help and long-term drug treatment, since an infected person is dangerous to others. It is a source of infection and can therefore infect other people.
Standard therapy aimed at eliminating demodicosis infection consists of several parts:
- Diet for demodicosis. The patient will need to give up fatty, spicy and smoked foods. It is also recommended to reduce your consumption of sugar and sweets. The diet should consist of low-fat fish, vegetables and fruits;
- Local treatment. For this purpose, sulfur ointment is used for demodicosis, creams and sprays that have antibacterial and antiparasitic properties;
- Systemic treatment. It is aimed at normalizing sebum production and eliminating existing imbalances (hormonal or metabolic). To do this, it is possible to involve specialized specialists, prescribe antibiotics in tablet or injection form;
- Symptomatic treatment. It is aimed at improving the patient’s well-being, eliminating active symptoms (inflammation, itching, soreness and redness). For this purpose, a special anti-demodetic mange may be prescribed;
- Physiotherapy. To improve the condition of the skin, electrophoresis, laser therapy and ozone therapy are prescribed.
Since it is practically impossible to cure demodicosis quickly but effectively, the average duration of the treatment course ranges from one to several months. The duration depends on the severity of the pathology and the individual characteristics of the body (in some cases, treatment may take a year or more). The main criterion for cure is a repeat tape test with a negative result.
As is known, mites of the genus Demodex are often considered the etiological and pathogenetic agent in the development of papulopustular dermatoses. An important point is that mites, complicating existing skin diseases, reduce the clinical effect of therapy, thus contributing to the transition of dermatoses to a chronic form. An additional difficulty for antiparasitic therapy is created by the structural features of mites, which makes it necessary to prescribe long courses of therapy and select drugs with a minimum molecular size. The effect of the drug is hampered by the dense cuticle covering the body of the mites, which has three layers: the outer layer is the epicuticle, the middle layer is the exocuticle and the inner layer is the endocuticle. The exo- and endocuticle are impenetrable, so the body of the mite is difficult to access by large molecules of exogenous substances, incl. for acaricidal drugs. Communication with the external environment of ticks occurs through water or gas exchange [3].
In order to achieve the elimination of ticks, antiparasitic (acaricidal) drugs are used. Over the years, metronidazole, which is a derivative of the nitroimidazole group, has proven the greatest clinical effectiveness. This drug is prescribed for a course of 4 to 6 weeks [7, 29]. It has been established that metronidazole enhances the protective and regenerative functions of the mucous membrane of the stomach and intestines [2, 4] and causes a pronounced anti-edematous effect [30]. The drug has a bacteriostatic effect, complicating the DNA synthesis processes of gram-negative anaerobic bacteria [13, 38], and is also antiparasitic against Demodex folliculorum [2].
Studies by DI Grove (1997) and PG Nielsen (1988) have proven the suppressive effect of the drug on some indicators of cellular immunity, in particular the suppression of leukocyte chemotaxis [26, 32]. The drug has an immunomodulatory effect due to the inhibition of vascular endothelial growth factors, preventing neoangiogenesis [15]. Tolerability of the drug is generally satisfactory. Side effects include headache, nausea, vomiting, dry mouth, urticaria, itching, leukopenia, candidiasis [13].
A.A. Frankenberg (2007) notes that in recent years, failures in the treatment of demodicosis with metronidazole have increased significantly. In his opinion, the ineffectiveness of therapy may be associated with the development of resistance of bacterial-parasitic flora to metronidazole, which has been used for more than 40 years [16]. As an alternative method of treating demodicosis, Ya.A. Yutskovskaya (2010) suggested using metronidazole topically. The study showed significant clinical improvement, which was manifested in a decrease in erythema, the number of papulopustular elements and the severity of the inflammatory process. According to the authors, laboratory elimination of mites after 14–21 days reached 2–3 mites in a scraping per 1 cm2 [17].
From the group of other synthetic antibacterial agents, the 5-nitroimidazole derivative ornidazole is widely used in cycles of 8 to 10 days. The drug has both antiparasitic and bacteriostatic effects, increases the activity of neutrophils, stimulates adrenergic structures, and enhances reparative processes [4, 18].
When comparing the effectiveness of the drugs ornidazole and metronidazole A.A. Frankenberg et al. (2007) the following results were obtained: the therapeutic effect when using ornidazole occurs almost 2 times faster compared to metronidazole; patient tolerability of the drug is satisfactory; minor side effects were noted, among which the most common were nausea and a metallic taste in the mouth; The blood and urine test results of the patients before and after treatment were within normal limits. When treated with metronidazole, side effects were observed more often, including: nausea, metallic taste in the mouth, dizziness, and the development of candidiasis. During 9 months of observation of patients taking ornidazole, there was no relapse [9, 16].
When choosing local treatment for demodicosis, one should take into account the general principles of external therapy used in dermatology. In some cases, etiotropic therapy should be immediately prescribed; in some cases, symptomatic therapy should be started, aimed at eliminating and resolving acute inflammatory manifestations and accompanying subjective sensations. Strict personalization of external treatment and constant monitoring of the patient's condition are necessary. In acute and subacute forms of the inflammatory process, you should first use dosage forms with a surface action of agents (lotions, shaken suspensions, pastes). After eliminating the acute inflammatory phenomena, the next stage is to switch to the ointment form of the drug, which acts directly on the etiological factor.
In external therapy, drugs containing metronidazole 1% in the form of an ointment or gel are most often used for 14 days. Metronidazole acts on the body's nonspecific resistance and affects cell-mediated immunity [33, 35]. As an alternative therapy, topical application of 10% benzyl benzoate ointment at night is possible [1, 6, 23]. Demoten gel (sulfur, hyaluronic acid, AloeVera juice, polyvinylpyrrolidone) for the treatment of patients with demodicosis and rosacea was highly praised [14].
In special cases, pathogenetic treatment is carried out for demodicosis. For example, in the case of acneiform type demodicosis or resistance to antiparasitic drugs, it is advisable to use systemic retinoids (isotretinoin) at a dosage of 0.1–0.5 mg/kg body weight per day for 2–4 months [24].
For the treatment of demodecosis of the periorbital region, alcohol-ether mixtures, 3–5% trichopolum cream, sodium sulfapyrazine, anticholinesterase agents (cholinomimetics): physostigmine, 0.02% phosphakol, 0.01% armin, 0.5% - ny tosmilen [11]. Good treatment results are observed with the use of blepharogel-1 and -2, blepharolotion [12].
Recently, dermatological practice has been significantly enriched with new drugs, significantly increasing the possibilities of choice in the treatment of patients with parasitic dermatoses. The drug Spregal, containing a solution of esdepaletrin and piperonyl butoxide, showed high effectiveness. It is used on the affected areas of the skin, rubbing with a swab 1-3 times a day. The drug is well tolerated and does not cause serious side effects [5, 8].
Permethrin (a group of pyrethroids) also has antiparasitic properties. Pyrethroids bind to the lipid structures of nerve cell membranes, disrupting the functioning of sodium channels that regulate membrane polarization. Repolarization of the membrane is hindered, which paralyzes the parasite. The important point is when pyrethroid molecules are able to penetrate the tick cuticle and concentrate in the hemolymph [3]. Permethrin 5% cream is applied twice daily for 15–30 days [31, 37]. However, we must remember that the permeability of different areas of the skin is not the same. Medicinal substances penetrate most actively into the skin of the face, where the thickness of the stratum corneum is minimal, so the rapid development of side effects in the form of erythema and simple contact dermatitis is possible.
The drugs ivermectin, lindane 1%, and crotamiton 10% also have acaricidal activity [23, 29]. Ivermectin is a synthetic derivative of compounds with antiparasitic activity known as avermectins. The drug is effective against endoparasites with tropism for the skin (Strongyloides stercoralis, Ancylostoma braziliense, Cochliomyia hominivorax, Dermatobia hominis, Filaria bancrofti, Wucheria malayi, Onchocerca volvulus, Loa-loa) and ectoparasites (Sarcoptes scabies, Pediculus humanus, Demodex folliculorum and Cheyletiella spr.) [22]. Foreign studies recommend using ivermectin systemically or topically in the form of a 1% cream. Studies have proven that ivermectin has antiparasitic and anti-inflammatory effects. Clinical improvement with topical 1% ivermectin cream was observed after 12 weeks of therapy [27]. The drug is administered orally at a dose of 200 mg/kg body weight twice with a break of 7 days [28]. However, in Russia this drug is used only for the treatment of demodicosis in animals. The use of 1% lindane also raises many doubts due to its neurotoxicity, therefore the drug is banned in a number of countries, and in some its use is limited [21]. As for the drug crotamiton 10%, it is applied to the skin at night for two to three days and is quite often used in pediatric practice [20, 34].
Among physiotherapeutic techniques, it is recommended to use the properties of narrow-band blue light (405–420 nm). The wavelengths of blue light are slightly longer than those of ultraviolet radiation, so narrow-band blue light reaches the reticular layer of the dermis, penetrating to a depth of 2.5 mm, corresponding to the location of the sebaceous glands. Single observations indicate the high effectiveness of this method in the treatment of acne complicated by demodicosis [10]. Some studies have proven the positive effect of using intense pulsed light (IPL - Intensive Pulse Light), discovered in 1992 and having a wavelength from 515 to 1200 nm [25]. IPL radiation suppresses the secretion of the sebaceous glands with their subsequent involution, which leads to the resorption of lymphocytic infiltrates and the death of mites [36].
Cryotherapy has an antidemodic effect, and to achieve a more lasting therapeutic effect, it is recommended to use cryotherapy in combination with external preparations containing metronidazole [1, 19].
Despite the fact that, according to various authors, the current “gold” standard and most effective method of treating demodicosis is the systemic use of the antiparasitic drug metronidazole, the drug itself has many side effects and has a number of contraindications. Since the search for new therapeutic agents that have the least negative effect on the body remains a pressing topic in medicine, we assessed the effectiveness of external therapy for demodicosis in comparison with the systemic use of drugs.
The purpose of this study: to compare the traditional treatment regimen for demodicosis of the facial skin (250 mg metronidazole orally 2 times a day; topically - 1% metronidazole cream once a day for 20 days) with the effectiveness of topical therapy (7% metronidazole cream topically for 20 days).
Material and methods
The study included 64 patients with acne and rosacea complicated by demodicosis. The diagnosis of acne and rosacea was made at the initial appointment based on the clinical picture of the diseases. At the same time, the main complaints of patients were taken into account, divided into the following groups: rashes, pain, burning, redness, itching, pigmentation, the presence of crusts/excoriations, telangiectasia, oily sheen. When assessing the local status (status localis), the following primary and secondary morphological elements were identified: papules, pustules, open comedones, milia, telangiectasia, crusts, redness, pigmentation, oily sheen. Each morphological element was counted and the clinical picture as a whole was assessed for the presence of perifocal erythema and oily sheen of the facial skin in patients before and after treatment. All patients included in the study were examined for the presence of Demodex mites by scraping the facial skin and squeezing out the contents of the sebaceous glands before and after treatment. The diagnosis of demodicosis was established when more than 5 mites per 1 cm2 were detected. The study included men and women over 18 years of age with no somatic complications and upon signing informed consent to participate in the study.
All patients were divided into two equal groups depending on the chosen treatment method. Patients of the first group (n=32) received 250 mg of metronidazole orally 2 times a day, externally - 1% metronidazole once a day for 20 days, patients of the second group (n=32) received 7% metronidazole externally in within 20 days. The treatment method was chosen randomly.
Statistical data processing was performed using the SPSS-21 software package. The relationship between categorical indicators was determined by Fisher's exact method. Fisher's exact test is a test of statistical significance used in the analysis of categorical data when sample sizes are small. To assess the significance of differences in follicle sizes, one-way analysis of variance with pairwise comparisons was used.
Research results
Of all the patients included in the study, 38 (59.37%) had acne and 26 (40.62%) had rosacea. The distribution by gender, age and diagnosis is presented in Table. 1.
The patients' return visit took place after 20 days of continuous therapy. Subjectively, both treatment regimens were well tolerated by the patients, no side effects were noted, and none of the patients were excluded from the observation group. Evaluation of the effectiveness of therapy was based on patient complaints and clinical picture. As can be seen from table. 2, after treatment there was a statistically significant decrease in patient complaints of rashes, burning, pain, itching, and redness. Moreover, in patients of the second group, complaints about oily skin decreased, which is an additional advantage of topical therapy.
Analysis of clinical manifestations after therapy showed that the number of the following morphological elements in patients of the first and second groups significantly decreased: papules, pustules, perifocal erythema, excoriations (p = 0.005) compared to the initial data (Fig. 1, 2).
When repeated scraping for the presence of Demodeх mites in two groups, the following data were obtained: in the first group, mites were found in 19 (30%) patients, in the second - in 20 (32%), i.e. mites of the genus Demodex after treatment in the two groups were found in approximately equal numbers of cases.
Thus, assessing the results of treatment, we can state that the effectiveness of therapy in both groups was the same. Analysis of the clinical picture showed a positive dynamics of therapy, which was manifested in a significant decrease in the number of morphological elements characterizing the severity of inflammation. The effectiveness of therapy was confirmed by a decrease in subjective complaints of patients after treatment, and in patients who received only external therapy, complaints about oily skin decreased, which is an additional advantage. Thus, clinical observations have demonstrated the lack of superiority in systemic therapy of demodicosis compared to external therapy using a drug containing 7% metronidazole in the form of a cream or cream-gel, which was confirmed by the results of statistical analysis.
conclusions
Our study showed that the use of a topical product containing 7% metronidazole for 20 days by patients with demodicosis is comparable in effectiveness to systemic treatment with metronidazole 250 mg orally for 20 days. External use of 7% metronidazole makes it possible to avoid polypharmacy and systemic administration of the drug, which reduces the risk of developing side effects of therapy.
Demodicosis - drugs for treatment
Today, finding effective remedies for demodicosis will not be a problem. The specialists of our medical center select medications in the optimal form on an individual basis, thereby speeding up the healing process. The most popular and effective remedies are described below.
Soap
- Demolan Forte and Stop Demodex demodex.by are especially popular among patients. For demodicosis of the eyelids, the treatment regimen often includes these drugs, as they show excellent results due to the presence in the composition:
- Glycerin - absorbs moisture, holding it on the skin. This helps prevent drying, promotes hydration and improves elasticity;
- Octopirox is an antimicrobial component that inhibits the activity of ticks. It gently exfoliates the top layer of the epidermis, normalizing the process of formation of new cells;
- Propylene glycol - helps normalize microflora, moisturizes the stratum corneum;
- Diazolidinyl urea - provides an antimicrobial effect.
Lotion
Demolan Forte and Stop Demodex lotions are prescribed for constant facial skin care and for cleansing damaged skin areas (even demodicosis on the back) before using the gel. They are often used for eyelid hygiene (for blepharitis), as they deeply cleanse the pores and facilitate the penetration of the active substances of subsequent medications. With their help, it is possible to soften the epidermis and normalize fat metabolism without resorting to tapping the skin. As a result of their regular use, mites are deprived of their nutrient medium, and the tissue is regenerated at an accelerated rate without the formation of scars.
Balm
Therapeutic and prophylactic balm Stop Demodex significantly increases the effectiveness of the main therapy. With its regular use, a visible therapeutic effect is observed after 2-3 days. It has the following properties:
- Anti-inflammatory and bactericidal;
- Moisturizing the skin;
- Promotes rapid tissue regeneration and healing;
- Improves local metabolism;
- Penetrates the cell membrane of the epidermis, replenishes the lack of microelements.
Eye gel
When diagnosing eye demodex, it is strongly recommended to use Demolan Forte and Stop Demodex gels. The presence of peppermint extract in the composition guarantees local anesthesia and inhibition of inflammation. They have a calming and refreshing effect, due to which the patient’s well-being noticeably improves. The presence of metronidazole provides effective antiprotozoal and antibacterial effects, while hyaluronic acid helps improve skin elasticity and firmness. These demodicosis preparations are perfectly absorbed, do not clog pores and do not disrupt cellular metabolism. They accelerate tissue regeneration and prevent the formation of scars.
Cream
An effective cream for demodicosis, Stop Demodex, with constant use, makes it possible to stabilize the normal secretion of the sebaceous glands, restore the skin microflora, eliminate the uncontrolled proliferation of parasites of the Demodex genus and noticeably cleanse the skin from foci of inflammation. It does not contain antibiotics, perfectly nourishes, increases tissue firmness and elasticity, and does not have a comedogenic effect.
Mask
For demodicosis infection, it is strongly recommended to buy a Stop Demodex treatment mask. It contains the active Cutipure complex and white clay, which promotes deep cleansing of pores and reduces the proliferation of pathogenic mites. It has anti-inflammatory, antibacterial and keratolytic effects. Its use allows you to normalize sebum production, tone the skin, improve metabolic processes in cells and accelerate tissue regeneration. Moreover, with its help it is possible to remove toxic molecules.
Shampoo
Using Stop Demodex shampoo for demodicosis of the head, you can significantly reduce itching, eliminate dandruff and stop the active reproduction of parasites. It has a strong anti-inflammatory and regenerating effect, fights mites and helps eliminate the consequences of the disease. Its effect is aimed at preventing ticks from sucking nutrients, disrupting their DNA replication and protein synthesis in the cell. The drug inhibits tissue respiration, which is vital for parasitic life.
Description of the drug
Trichopolum is an antimicrobial drug with antiparasitic activity, but is not an antibiotic.
The main component in all types of the drug is metronidazole. Available in the form:
- Tablets for internal use. They contain a chemical substance in a dosage of 250 mg, as well as: magnesium stearate, molasses, starch and gelatin. Packaged in cardboard packages of 20 tablets along with instructions.
- Solution for intravenous administration. It contains: sodium chloride, water, citric acid monohydrate and sodium hydrogen phosphate. In pharmacies you can find ampoules with a dosage of 100 mg per 20 ml and bottles with a dosage of 500 mg per 100 ml.
- Vaginal tablets. Additionally contain: cellulose, crospovidone, silicon dioxide, povidone and stearic acid. The concentration of metronidazole is 500 mg, packaged in 5 or 10 pieces per package.
The effect of the drug is to penetrate the cell of a microorganism and disrupt its vital functions, followed by death. It has shown effectiveness in the fight against protozoa, anaerobic bacteria and some gram-negative and gram-positive organisms, for example, lamblia, trichomonas, gardnerella.
It is stored for three years from the date of issue at a temperature of no more than 25 °C.
Prevention
Demodicosis of eyelashes and other parts of the body can be prevented. To do this, it is enough to follow simple preventive rules. This:
- Maintaining personal hygiene (regular showering, thoroughly washing your face, washing your hair and hair);
- Eat a varied, rational and healthy diet (include fish, vegetables and fruits in your diet);
- Increased immune defense;
- Correct selection of decorative and skincare cosmetics;
- Do not use other people's cosmetics and personal hygiene products.
How is demodicosis of the eye transmitted?
Demodectic mange of the eyes can be contracted at home - by sharing hygiene items, towels, bed linen, and cosmetics with the patient.
To prevent re-infection, you need to change your pillowcase and towel (or use paper towels) daily, and throw away contaminated cosmetics.
To treat each eyelid, you must use a separate (new each time) cotton swab.
1 Diagnosis and treatment of demodicosis
2 Diagnosis and treatment of demodicosis
3 Treatment of demodicosis
Demodicosis in children
- In childhood, this pathology rarely develops (due to the low activity of the sebaceous glands), but its course is much more complicated than in adults. As a rule, in children this disease is chronic, and relapses occur in the off-season. The main signs of the problem are:
- Swelling of the eyelids;
- Loss of eyelashes and hair;
- Severe eye fatigue;
- The appearance of spots on the skin;
- Itching, worse at night and on contact with water;
- Decreased appetite, moody behavior, decreased physical activity;
- Pain in the eyes.
The treatment regimen for democosis of the face and other parts of the body in children is practically the same as therapy for adults. It also includes diet, medication and rehabilitation aimed at healing the tissue and preventing scarring. The fundamental difference in the treatment method is only the dosage of medications, which will be lower in childhood.
Analogs
| Name | Active substance | Maximum therapeutic effect, hours | Price per package, rub. |
| Metrogil | metronidazole | 2 | 23-185 |
| Rozamet | metronidazole | 3 | 191-210 |
| Metroseptol | metronidazole | 2 | 160 |
| Efloran | metronidazole | 2-3 | 801 |
Substitutes are used in cases where the patient is allergic to the components that make up Trichopolum. In any case, therapy is prescribed by the attending physician.
Demodicosis in men
Demodectic mange infection occurs in both women and men, regardless of age or race. It has no distinctive features in its course, prognosis, symptoms and causes of development. Therapy is prescribed on an individual basis, but is usually the same for all genders. Differences may only relate to the dosage of medications.
According to statistics, women suffer from demodicosis 4 times more often than men. There is no scientific explanation for this information, but many are inclined to the hormonal theory. It is based on the fact that due to a regular surge of hormones (menstrual cycle, pregnancy), female representatives are more prone to stress and immunodeficiency states. The clinical picture of the disease is standard and includes:
- Skin rash of varying severity;
- Itching, pain and discomfort in the damaged area;
- Increased sebum production;
- Pain in the eyes, sensation of a foreign body.
The treatment regimen for demodicosis for women is standard. It consists of a diet, long-term medication and the use of special care products (oils, lotions, creams, etc.) to prevent relapse and consolidate the therapeutic result.
Analogs and price
A similar composition has: Gravagin, Metrogyl, Metronidazole, Efloran, Flagyl.
The price of Tripohol varies depending on the dosage form. Tablets cost from 66 rubles, vaginal suppositories - from 285 rubles, the solution is not available for free sale.
Thus, this drug has a wide spectrum of action, low price and proven effectiveness. However, it is not without side effects in the form of a bitter taste and a negative effect on the intestinal microflora.
Questions and answers on the disease
Can a sick person infect others?
Yes, you can become infected with demodicosis through contact and household contact. Kissing, hugging, contact with contaminated things of a patient (towel, bed linen, clothes and much more) can be dangerous for a healthy person. But this does not guarantee the manifestation of symptoms of the disease. Ticks of the genus Demodex are representatives of the opportunistic microflora of the skin. They are found in almost all people, but most of them are simply carriers. For the development of a pathological process, the presence of certain factors is necessary (for example, reduced immune defense against the background of an active or past disease).
Can you get infected from animals?
Animals, like humans, suffer from the activity of Demodex mites. But pathogens come in different types - and each of them survives exclusively in the body of its host. When exposed to other conditions, the parasite immediately dies. Therefore, it is impossible to become infected with demodicosis from a pet or wild animal.