Etiology of the disease
- The causative agent of skin tuberculosis is Mycobacterium tuberculosis, which was first discovered by R. Koch in 1882.
- The tuberculosis bacillus belongs to the family of radiant fungi, the genus of mycobacteria, which, in addition to it, includes the causative agents of leprosy, scleroma and more than 150 species of atypical mycobacteria.
- Mycobacteria reproduce by division and budding. This process lasts 24 hours.
- MBT exhibit significant stability in the external environment. They cannot be frozen out. They remain viable in boiling water for up to 15 minutes. They live in manure for up to 15 years, and up to 1 year in wastewater. When dried, the pathogen remains viable for 3 years.
- Mycobacteria are resistant to phagocytosis (macrophages cannot destroy the mycobacterium, although they begin to fight it - incomplete phagocytosis).
- There are human, bovine and intermediate types of MBT.
- The pathogen has the appearance of an elongated rod of a rather complex structure: a three-layer cell wall and intracellular membrane contain polysaccharides, lipoprotein complexes and proteins. Proteins are responsible for antigenic properties (tuberculin). Polysaccharides play a role in antibody detection. Lipid fractions help MBT resist acids and alkalis.
Rice. 2. Mycobacterium tuberculosis.
Ways of spreading skin tuberculosis
- Patients with tuberculosis spread the infection through sputum, urine, through fistulas and household items. The source of infection is also sick animals and food products contaminated with MBT from sick animals. During the formation of immunity, primary skin tuberculosis occurs (tuberculous chancre, lichenoid tuberculosis of the skin).
- There are a number of diseases that are associated with tuberculosis not directly, but indirectly. These are allergic vasculitis, resulting from allergic immune (“paraspecific”) inflammation in response to infection with mycobacteria (rosacea-like Lewandowski tuberculide).
Rice. 3. The photo shows tuberculosis of the skin of the face and neck.
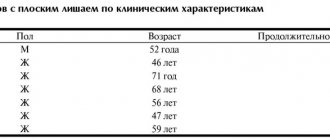
Combination of lichenoid and colliquative tuberculosis of the skin (scrofuloderma)
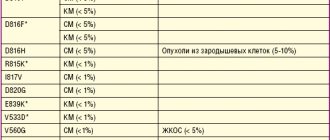
Tuberculosis (from the Latin tuberculum - tubercle, English tuberculosis) is an infectious disease caused by Mycobacterium tuberculosis, characterized by pronounced clinical heterogeneity and the development of a specific inflammatory reaction in the organs and tissues of the human body [1]. The threat of a pandemic, a high mortality rate, an increase in cases of multidrug-resistant tuberculosis and the economic damage caused by the disease make the incidence of tuberculosis one of the most important problems in global health [2, 3]. The most common active form of tuberculosis affects people of working age from 18 to 44 years (in 2014 - 62.3% of the total number of patients) [4]. According to the World Health Organization, tuberculosis has the highest morbidity and mortality rates, with 8 million new cases of tuberculosis and 3 million deaths associated with tuberculosis reported annually [5]. In the Russian Federation in the 21st century. the peak incidence was observed in 2008. However, by 2014, the decrease in the incidence of tuberculosis compared to 2008 was 30.1% (85.1 per 100,000 population) [4]. According to the literature, the mortality rate from tuberculosis in the Russian Federation in 2014 decreased by more than half due to an increase in the mortality rate of patients with co-infection with HIV and tuberculosis [4]. It should also be noted that multidrug-resistant tuberculosis is increasing worldwide [5]. The Russian Federation still ranks first in identifying cases of multidrug-resistant tuberculosis: 24.2 per 100,000 population in 2013 and 24.8 per 100,000 population in 2014 [4]. In connection with the actualization of the problem of tuberculosis in general, interest in its extrapulmonary form has increased in recent years [6, 7], including cutaneous tuberculosis (STB). However, due to less contagiousness and pathogenesis, incidence rates of extrapulmonary tuberculosis are at a significantly lower level compared to respiratory tuberculosis [2]. There is no convincing data on an increase in the number of cases of TC [6, 7]. There is no generally accepted classification of TC. According to the National Guidelines for Phthisiology 2014, cutaneous tuberculosis is divided into 2 main groups (Table 1) [1]: • true cutaneous tuberculosis (localized, granulomatous or bacterial); • skin lesions as a result of allergic immune (paraspecific) inflammation, mainly in the form of allergic vasculitis, called disseminated, hyperergic cutaneous tuberculosis and classified by Daria as “tuberculides”.
In the 2013 National Guidelines for Dermatovenereology, miliary tuberculosis and lichenoid tuberculosis are classified as disseminated forms [8]. According to the literature, TB ranks 5th among all locations of extrapulmonary tuberculosis (osseous-articular, genitourinary and digestive systems, lymph nodes) [9]. This distribution is associated with the fact that in the vast majority of cases, TB is secondary to tuberculosis of internal organs [1], which suggests the possibility of pathomorphism of tuberculosis infection and the appearance of erased and atypical, difficult to diagnose forms of skin lesions [6, 7, 10]. Thus, according to the literature, patients with undiagnosed TC have been treated for a long time for chronic pyoderma, allergic vasculitis, lupus erythematosus, perioral dermatitis, lichen planus, pruritus, eczema, Beck’s sarcoidosis, rubrophytosis, Dühring’s dermatitis herpetiformis, migratory thrombophlebitis [10] . Complicating the diagnostic search are the so-called paraspecific tissue reactions or “masks” of tuberculosis that occur in response to tuberculosis infection and are characterized by various nonspecific changes in organs and tissues. Lesions of the skin and mucous membranes are often represented by erythema nodosum and keratoconjunctivitis, rarely by hemorrhagic vasculitis and panniculitis. This phenomenon is observed mainly in primary and disseminated tuberculosis [11]. There have also been changes in the general structure of TC incidence. So, in the middle of the twentieth century. the most common were tuberculous lupus and colliquative TC; currently, on the contrary, predominantly disseminated forms of TC are recorded [3, 10]. Based on materials from the clinic of skin diseases of the First Moscow State Medical University named after. THEM. Sechenov analyzed the dynamics of clinical forms of tuberculosis over 70 years, from 1895 to 1964, and found that during this period there were 525 patients with various forms of skin tuberculosis in the clinic. Of these, 70.2% suffered from lupus vulgaris, 5.3% from scrofuloderma, 10.2% from papulonecrotic tuberculosis, 11.6% from erythema induratum, and other forms accounted for 2.7% [12]. From 1991 to 2000, the clinic recorded only 2 TB patients, one of whom was a resident of the Far East. After a long period of absence of patients with both TC and paraspecific tissue reactions for 6 months. In 2015, the clinic recorded 5 cases of TC, of which 1 case was scrofuloderma, 1 case was papulonecrotic tuberculosis associated with pulmonary tuberculosis, 2 cases were erythema induratum, 1 case was TC associated with kidney tuberculosis as a complication of immunosuppressive therapy. cyclosporine therapy; in 1 – lupus vulgaris. The patient with papulonecrotic skin tuberculosis is a resident of Dagestan, the patient with erythema induratum is a resident of Astrakhan, the other 3 patients live in Moscow. Thus, the problem of TC remains relevant and requires further study. Causative agents of skin tuberculosis: M. tuberculosis, M. bovis, in rare cases - bacilli Calmette-Guerin (BCG). TC is transmitted through the skin - primary infection, and also spreading through the lymphogenous or hematogenous route when internal organs are damaged - secondary infection. The most contagious form of TC is scrofuloderma (colliquatic TC). The term "scrofuloderma" was first introduced by Jadasson. French authors called this disease "gommes scrophuleuses" or "gommes tuberculeux". A feature of this pathology is the development of gummous nodes in the subcutaneous tissue, which undergo caseous softening and ulceration resulting in a bridge-shaped scar. There are two clinical varieties: primary, characterized by the initial formation of tuberculous granulomas in the skin, and secondary, as a result of the spread of the pathological process from regional lymph nodes [6, 7]. Primary scrofuloderma can be localized on any part of the skin, secondary - mainly in the parotid, submandibular and supraclavicular areas, on the lateral surfaces of the neck [6, 7]. The rashes are initially presented as small, dense, mobile, painless bumps the color of normal skin, which, quickly increasing in volume, turn into sharply demarcated nodes that are not fused with the surrounding tissues. Gradually, the nodes acquire a bluish tint, soften, and the skin over them loses mobility. They can remain in this state for a long time, forming “cold abscesses,” or open with the formation of deep ulcers, the release of purulent-necrotic contents, and the formation of fistulas and pockets. The elements resolve into bridge-shaped disfiguring scars [8, 9], along the periphery of which new tubercles and nodes form, as a result of which the lesion takes on a serpentine character. There is a pronounced evolutionary polymorphism [6, 7]. The pathomorphology of primary and secondary scrofuloderma is similar. The epidermis is intact, in the upper parts of the dermis the changes are nonspecific: foci of necrobiosis, infiltrate of mononuclear cells, in the lower parts of the dermis and subcutaneous fatty tissue - tuberculoid granulomas consisting of epithelioid, giant cells and lymphocytes, with caseous necrosis in the center, when stained according to Romanovsky - Giemsa detects mycobacteria [9, 13, 14]. To confirm tuberculosis lesions, the latest diagnostic methods are used, such as the Diaskin test, ultrasound examination of soft tissues, epiluminescence dermatoscopy, polymerase chain reaction, and immunohistochemical detection of Mycobacterium tuberculosis antigens [2]. Treatment of TB is carried out together with TB specialists with specific anti-tuberculosis drugs, the prognosis is favorable. A feature of this form of tuberculous skin lesions is a long-term chronic relapsing course with a tendency to spontaneous scarring of ulcers [9]. Differential diagnosis of TC is carried out with sarcoidosis, papulonecrotic angiitis, secondary and tertiary syphilis, lymphocytoma, B-cell lymphoma of the skin, leprosy, discoid lupus erythematosus, deep mycoses, leishmaniasis and other dermatoses, depending on the clinical form of TC. The prognosis is relatively favorable in the absence of resistance to anti-tuberculosis therapy [9]. Considering the rarity of the pathology, we present our own clinical observation of a case of colliquative tuberculosis of the skin.
Clinical case
Patient B., 67 years old, was in the Moscow City Scientific and Practical Center for Combating Tuberculosis with complaints of rashes on the skin of the upper body, moderate general weakness, accompanied by an increase in body temperature in the evening to 37.5 ° C, loss of appetite.
Over the past 2 years, the patient notes a weight loss of 22 kg. From the life history
it is known that before retiring she worked in a hot shop and had contact with acids and dust.
Concomitant diseases: varicose veins of the saphenous veins of both lower extremities, chronic venous insufficiency of II–III degree; bilateral retinal angiopathy, initial cataract, chronic blepharoconjunctivitis; chronic iron deficiency anemia; vascular (toxic) hypoacusia; hypertension stage II, degree I, risk of degree 2. From the medical history.
About 3 years ago, the patient first noticed the appearance of a tumor-like formation in the supraclavicular region on the left.
The local surgeon assessed the formation as an abscess and opened it. No scarring of the ulcer was observed. Subsequently, at the site of the opened nodes, the appearance of deep ulcerative defects like fistulas was noted in the axillary region on the left, on the anterior chest wall on the left. Antibacterial therapy was carried out periodically. 1.5 years after the onset of the disease, a computed tomography scan of the chest organs was performed, which revealed exudate in the left pleural cavity and destruction of the second rib on the left. She was consulted at the Moscow City Scientific and Practical Center for the Fight against Tuberculosis at the State Budgetary Healthcare Institution of the Department of Healthcare of the City of Health, and a diagnostic and treatment puncture of the left pleural cavity was performed, during which the process could not be identified, and no growth of secondary flora was obtained. An abscess of the anterior chest wall was punctured and acid-fast mycobacteria were detected using fluorescent microscopy. Objectively
.
The consciousness is clear, the physique is asthenic. Body temperature rises in the evening to 37.5° C. The skin outside the lesions is pale; visible mucous membranes are pale pink and clean. The state of the muscular system corresponds to age. Active and passive movements in the joints are fully preserved. On auscultation over the right lung, breathing is harsh, on the left it is weakened mainly in the lower parts, there is no wheezing. Percussion sound with a boxy tint in the lower sections on the right, on the left - shortening of the percussion sound in the lower sections. Respiration rate – 20 per minute. Heart sounds are clear, rhythmic, no murmurs; heart rate - 72 beats per minute. Blood pressure – 120/80 mm Hg. The abdomen is soft and painless. The liver protrudes 1 cm from under the edge of the costal arch. The spleen is not palpable. Kidneys: Pasternatsky’s sign is negative on both sides. Urination is free and painless. No focal neurological symptoms were identified. Local status.
The skin process is chronic inflammatory in nature. The rashes are multiple, localized mainly on the skin of the trunk and limbs. They are represented by brownish-pink dense lichenoid tubercles, with clear boundaries, scalloped outlines, arranged in the form of arcs or rings, leaving the central area unaffected. At the site of regressed rashes there is pigmentation with superficial atrophy, there are no scars. On the left anterior chest wall, in the area of attachment of the third rib to the sternum, a spherical node with a diameter of 2 cm, dense consistency, mobile, painless, the skin over it is not changed. In the supraclavicular region on the left, in the left axillary region and on the anterior chest wall on the left there are numerous retracted bridge-shaped scars up to 3 cm in length and deep ulcerative defects with scanty thick discharge. The peripheral groups of lymph nodes are enlarged, the nodes are not fused to the skin, and are mobile. Particularly large conglomerates are identified in the left axillary region. The nail plates of the hands and feet are not changed. There are no subjective sensations (Fig. 1). Preliminary diagnosis: a combination of lichenoid and colliquative TC. In order to verify the diagnosis, a histological examination of the affected area of the skin was carried out, as well as an examination to identify concomitant pathologies. The results of histological examination demonstrated the following changes: in the dermis there were multiple, locally confluent macrophage-giant cell granulomas without necrosis. The morphology fits into the picture of granulomatous inflammation (Fig. 2).
As a result of laboratory tests, no gross pathology was identified. An electrocardiogram and results of a study of pulmonary function were unremarkable. X-ray
. In the left pleural cavity there is a shadow of exudate up to the anterior segment of the IV rib, enveloping the entire lung; at the level of the II rib there is a thickening of the pleura of a homogeneous structure, up to 15 mm thick; local pneumosclerosis in S1-2 on the left and S4-5 on the right; There is an increase in intrathoracic lymph nodes. Computed tomography of the chest: CT signs of nodular formation? Ultrasound examination of the thyroid gland reveals diffuse changes in thyroid tissue and lymphadenopathy. A comprehensive examination made it possible to diagnose a combination of lichenoid and colliquative TC (secondary scrofuloderma). Thus, it was revealed that patient B. had primary pulmonary TB in the past, as evidenced by local pneumosclerosis in S1-2 on the left and S4-5 on the right. Such indurative areas, as a manifestation of previous pulmonary TB, are biologically active. It is known that such residual tuberculous changes, the diameter of which is more than 1 cm and the number of which exceeds 5, and the hilar localization of the process are potentially dangerous, especially in people over 60 years of age [15, 16]. This is due to the fact that typical and modified variants of mycobacteria, especially the L-form, persist in these indurative areas [17]. At the age of 67 years, patient B. experienced endogenous reactivation of tuberculosis infection in a favorable epidemiological situation; acute progressive pulmonary tuberculosis arose with damage to the lymph nodes, pleuropneumonia and lymphohematogenous generalization of the disease to the skin. In the skin, the process is characterized by a combination of lichenoid and colliquative skin tuberculosis (secondary scrofuloderma).
Pathomorphology
With tuberculosis, a tubercle (tuberculum) appears around the embedded tuberculosis bacilli, the components of which are:
- inside the tubercle there are phenomena of caseous necrosis (damage) of tissues and Mycobacterium tuberculosis (a component inherent only in tuberculosis);
- surrounded by MBT cells specific for any granulomatous disease - lymphocytes, epithelioid cells and Pirogov-Langhans cells (cell proliferation);
- the outer layer (exudative component) is represented by cells macrophages, neutrophils, eosinophils (nonspecific component).
Rice. 4. Histological preparation of a tuberculous tubercle.
With tuberculous skin lesions, tubercular structures with a nonspecific inflammatory infiltrate are more common (there are few or no MBTs in the tubercle). Tuberculous granulomas are characteristic of tuberculous lupus. With allergic vasculitis that occurs in response to exposure to mycobacteria and their decay products, diffuse forms of skin tuberculosis occur. In this case, the vessels of the skin and subcutaneous tissue are affected.
Tuberculosis skin disease (clinical case)
The article presents a clinical case of skin tuberculosis in patients aged 5 and 17 years. Literature data on the incidence and characteristics of skin tuberculosis, medical history data, including anamnesis, and illustrative material are provided. The peculiarity of this case is the rarity of the clinical form of this disease.
Key words: skin tuberculosis, maintenance phase, intensive phase, ulcerative-necrotic form, papulo-necrotic form.
Relevance : Tuberculous skin disease is a rare form of tuberculosis, which includes lesions caused by Mycobacterium tuberculosis (MBT) that vary in clinical picture, pathomorphology and pathogenesis. [3]
The incidence of skin tuberculosis in Russia is annually detected on average 0.43 patients with skin tuberculosis per 100,000 population (in the areas of supervision of St. Petersburg Research Institute of Physics from 0–0.6), which is 5.6% of all extrapulmonary tuberculosis. Skin lesions are observed in 7% of patients with tuberculosis.
Skin tuberculosis most often affects women (about 70% of patients) aged 20 to 40 years. The risk group primarily includes people in contact with tuberculosis patients, butchers and farmers, diabetics, people in contact with sick animals, HIV-infected people, drug addicts, alcohol abusers, homeless people, prisoners, seasonal workers, immigrants. In children, as well as in adolescents, sclerofuloderma is more common. Infants often develop primary and miliary tuberculosis of the skin. The predominant development of tuberculous-allergic vasculitis occurs in middle-aged people in the presence of high specific reactivity of the vascular wall. [1,4]
Skin tuberculosis in the vast majority of cases (almost 70%) is secondary tuberculosis and develops only in individual patients with active tuberculosis of the lymph nodes, bones, and internal organs. MBT enter the skin by hematogenous, less often lymphogenous, route. But direct spread into the skin by contact is also possible. [4]
Classification of skin tuberculosis:
I. Chronically current primary tuberculosis:
1) collicative tuberculosis: primary scrofuloderma, secondary scrofuloderma, fungal tuberculosis;
2) diffuse forms of skin tuberculosis: papulonecrotic tuberculosis, indurated erythema, lichen scrofulus.
II. Secondary tuberculosis:
1) tuberculous lupus (flat, ulcerative, hypertrophic, papillomatous);
2) warty skin tuberculosis;
3) miliary ulcerative tuberculosis of the skin. [2,3]
Due to the rarity of occurrence of this disease and the difficulty of differential diagnosis, we present the described clinical cases of skin tuberculosis of the ulcerative-necrotic and papulo-necrotic form in children B. and K., aged 5 and 17 years, who were in the children's and adolescent department of the Regional State Clinical Hospital anti-tuberculosis dispensary" (OPTD) in Karaganda.
Clinical case no.1
Fig.1. Child B. Skin tuberculosis. Ulcerative-necrotic form
Complaints upon admission: skin rashes in the form of purulent crusts, redness and irritation of the skin around the rashes.
Medical history : Identified upon treatment. Referred to DO No. 3. Tuberculosis contact with mother, who has multidrug-resistant tuberculosis since July 2014. Bacillus Calmette-Gerin (BCG) scar 5 mm. Mantoux reaction with 2 TE from 01/09/2015. - 15 mm. Diaskin test dated 02/03/2015. — 8mm. The child suffered from tuberculosis for the first time in 2012. She was hospitalized in the children's department from May 28, 2012. until September 27, 2012 09/04/2012 surgery - lymphadenectomy of the cervical lymph nodes on both sides. Histological report dated 09/04/2012. No. 1778–85 - tuberculous lymphadenitis. Alternative productive tissue reaction. She received treatment in category 1. Outcome - treatment is completed. Complaints of skin rashes under the wings of the nose appeared in April 2014. I have repeatedly received treatment from a dermatologist and ENT doctor, without effect. After the result of a histological examination at the National Center for Tuberculosis Problems of the Republic of Kazakhstan (NCPT RK) dated 07/01/2015. No. 1821 (06.26.2015 - open biopsy of the facial skin) - tuberculous inflammation of the skin, ulcerative-necrotic form, the child was sent to the children's and adolescent department of the OPTD.
Central Medical Control Commission (CMCC) dated July 24, 2015. d/z Skin tuberculosis. Ulcerative-necrotic form. Active stage. Mycobacterium tuberculosis (MBT) - Type D (MBT relapse-). 4 category from tubes. exposure to MDR-TB. Intensive phase in category 4 180 doses from July 24, 2015. until January 19, 2016 CVCC dated January 20, 2016 - the same diagnosis. Considering the positive dynamics, she was transferred to the maintenance phase for 12 months. Support phase for category 4 from January 20, 2016.
Life history: 2nd child in the family. Vaccinated according to the calendar. He is not registered with specialists at the dispensary. The food is complete. 7 people live in a 3-room apartment. Allergy history: calm.
General condition on admission: Condition of moderate severity due to symptoms of intoxication. The state of health is disturbed. Consciousness is clear. The physique is asthenic. Reduced nutrition. Soft tissue turgor is reduced. The skin is pale pink, on the skin of the face the lesion is located in the nasal, subnasal, upper lip areas and buccal area on the left, the lesion is hyperemic, there is also an extensive ulcerative surface, ulcers up to 0.4 mm with an uneven bottom covered with purulent crusts, the edges of the ulcers are raised in the form roller In the nasal region there are areas minus tissue, in the buccal region there are areas plus tissue.
Visible mucous membranes are clean, physiological in color, and somewhat dry. Peripheral lymph nodes: submandibular, inguinal, axillary up to size 1, tightly elastic, mobile, painless, unfused. Nasal breathing is free. Zev is calm. On auscultation, breathing in the lungs is vesicular, there are no wheezes. Heart sounds are loud and rhythmic. The abdomen is soft and painless on palpation. The liver is not enlarged. The spleen is not enlarged. The effleurage symptom is negative on both sides. Urination is free and painless. The chair is formed, 1 time per day.
X-ray of the lungs: The lung fields are clean, the roots are structural. The diaphragm dome is smooth. The sinuses of the pleura are free. The boundaries of the heart are normal. Conclusion: there is no evidence of active tuberculosis in the lungs.
Anti-tuberculosis treatment: Intensive phase in category 4 from July 24, 2015. until 01/19/2016 - Levofloxacin -0.125 Capreomycin -0.4 Pro - 0.25 Cycloserine -0.75 Pyrazinamide -0.5 Ethambutol -1.2 Pas-1.0 Maintenance phase from 01/20/2016 until January 24, 2016 Levofloxacin -0.125 Pro - 0.25 Cycloserine -0.75 Ethambutol -1.2 Pas-1.0
Pathogenetic and symptomatic treatment : vitamins B1, B6, Hepadif, detoxification therapy.
Results and discussions: After the result of histological examination at the National Center for Traumatology and Therapy of the Republic of Kazakhstan dated July 1, 2015. No. 1821 (06/26/2015 – open biopsy of facial skin), the following clinical diagnosis was established: Skin tuberculosis. Ulcerative-necrotic form. Active stage. MBT-Type D (Relapse of MBT-). 4 category from tubes. exposure to MDR-TB.
Clinical case no.2
Fig.2. Teenager K. Skin tuberculosis. Papulo-necrotic form
Upon admission, complaints of rashes on the skin of the back.
History of the disease: The patient was identified upon presentation. No tuberculosis contact has been established. BCG scars 5 and 6 mm. Mantoux test with 2 TE dated June 22, 2015. - 14 mm. For the first time, rashes in the form of nodules without itching appeared on the skin of the back in 2014. I did not go to the doctor, I self-medicated. In June 2015, we consulted a dermatologist, who referred the patient to a phthisiatrician. On an outpatient basis to the patient on June 29, 2015. A biopsy of the skin and subcutaneous tissue was performed. A histological study was carried out at the OPTD in Karaganda - Conclusion No. 1384–85 dated 07/07/2015: The sent material contains skin tissue, under the epidermis there are areas of lymphoid infiltration with an admixture of epithelioid cells and Pirogov-Langhans cells. Specific inflammation of the skin of tuberculous etiology, exudative tissue reaction. 07/27/2015 glass preparations were transferred to Almaty to the NCPT of the Republic of Kazakhstan to confirm the histological conclusion. A conclusion was issued - tuberculosis of the skin and subcutaneous tissue. The girl was sent for inpatient treatment to the children's and adolescent department of the Regional Anti-TB Dispensary in Karaganda, where she had been receiving treatment since July 17, 2015. CVKK dated 07/18/2015 A clinical diagnosis was made - skin tuberculosis. Papulo-necrotic form. Active stage. MBT-I category. New case 1A group D-registration. Received first-line drugs: intensive phase from July 18, 2015. until September 15, 2015 60 doses - isoniazid 0.3, rifampicin 0.6, pyrazinamide 2.0, ethambutol 1.2. The maintenance phase ended on April 20, 2016. received isoniazid 0.3 and rafampicin 0.6.
Life history: 2nd child in the family. She grew up and developed according to her age. Not on D-registration. Social conditions are satisfactory. Parents and older brother undergo fluorography annually. Allergy history : according to the mother, without any peculiarities.
General condition upon admission: moderate severity due to symptoms of intoxication. Sleep is calm, appetite is reduced. On the skin of the back and partly on the chest, there are widespread rashes in the form of bluish-red nodules, in some places merging into continuous lesions with ulcerations and cicatricial changes. Itching is moderate. Visible mucous membranes are clean and pale. Peripheral lymph nodes: axillary up to 1-2 sizes, dense-elastic consistency, painless, mobile. Nasal breathing is free. Percussion-pulmonary tone. On auscultation, breathing in the lungs is vesicular, there are no wheezes. Heart sounds are loud and rhythmic. The abdomen is soft, painless on palpation, not swollen. The liver and spleen are not enlarged. Stool and urine output are normal.
X-ray of the lungs: The lung fields are clean, the roots are structural. The diaphragm dome is smooth. The sinuses of the pleura are free. The boundaries of the heart are normal. Conclusion: there is no evidence of active tuberculosis in the lungs.
Anti-tuberculosis treatment: Received first-line drugs: intensive phase from July 18, 2015. until September 15, 2015 60 doses - isoniazid 0.3, rifampicin 0.6, pyrazinamide 2.0, ethambutol 1.2.
Maintenance phase from September 16, 2015. until April 20, 2016, received isoniazid 0.3 and rafampicin 0.6 (received 153 doses). Pathogenetic and symptomatic treatment: Vitamins B1 and B6, detoxification therapy, enzymes.
Results and discussions: After the result of histological examination in the NCPT RK No. 1384–85 dated 07/07/2015. The following clinical diagnosis was established: Skin tuberculosis. Papulo-necrotic form. Resorption stage. MBT-I category. New case. 1A group D-accounting.
Both patients were discharged in satisfactory condition. With positive clinical dynamics, under the supervision of a local phthisiatrician.
Conclusions:
- Skin tuberculosis is a rare form of the disease, is one of the manifestations of tuberculosis infection and often accompanies tuberculosis of the lungs, lymph nodes and other organs, which served as a basis for discussing these clinical cases.
- The reason for the late detection of skin tuberculosis is the difficulty of diagnosis; vigilance is needed for doctors in the general medical network in order to diagnose this disease in a timely manner.
- The diagnosis is confirmed by histological and bacteriological studies of a biopsy specimen from the affected area of the skin.
- A thorough study of the epidemic history, infection, vaccination of children with BCG, and X-ray examination of children and adolescents will help reduce the late diagnosis of extrapulmonary skin tuberculosis.
Literature:
- Skin tuberculosis / M.K. Egizbaev // Bulletin of the South Kazakhstan Medical Academy. - 2006. - N2(28). — P.266.
- Journal "Emergency Medicine" 2012 Skin tuberculosis - Authors: Poteyko P. I., Krutko V. S., Khodosh E. M. - Kharkov Medical Academy of Postgraduate Education; Shevchenko O. S. – Kharkov National Medical University
- Phthisiology: Textbook. — 3rd ed., revised. And additional / Edited by: Perelman M.I., Koryakin V.A., Bogadelnikova I.V. - M.: OJSC Publishing House "Medicine", 2004. - 384p
- Guide to pulmonary and extrapulmonary tuberculosis. Edited by member. corr. RAMS, prof. Yu. N. Levasheva, prof. Yu. M. Repina. - St. Petersburg: ELBI-SPb. - 2008. - 544 p.
Primary cutaneous tuberculosis
This form of the disease is extremely rare. The disease develops during the development of primary tuberculosis. Children under 10 years of age are most often affected. Initially, a papule appears reddish-brownish in color. Next, an ulcer (tuberculosis chancre) appears in the center of the papule. Peripheral lymph nodes increase in size. Often ulcerate. Ulcers take a long time to heal. In their place, thin scars appear. With a weakened immune system, the disease returns again, disfiguring the body with scars and scars.
Secondary tuberculosis of the skin
The disease is represented by a variety of localized and disseminated forms that appear in previously infected people. Tuberculous lupus accounts for up to 75% of all cases.
In the last 10 years, there has been a predominance of disseminated forms of cutaneous tuberculosis.
Ordinary or vulgar tuberculous lupus (Lupus vulgaris)
In the recent past, lupus was the most common form of cutaneous tuberculosis. Today, disseminated forms are more often recorded. MBT penetrate into the skin from regional lymph nodes through the lymphatic tract and hematogenously (with the bloodstream). The disease often occurs in childhood, lasts a long time, with periodic exacerbations, and spreads slowly.
Symptoms of the disease
The disease affects the skin of the nose, face, neck, red border of the lips, mucous membranes of the mouth and eyes. The skin of the extremities is rarely affected. Tuberculous tubercles merge and form lupomas. Their color is yellowish-rusty. Size – up to 0.75 mm. At first, the lupomas are located deep, and then they begin to protrude above the skin.
The shape of the lupoma is round, the consistency is soft, with significant pressure from the probe, the elements of the lupoma rupture, causing pain and bleeding. Lupomas often merge. Their surface is smooth and shiny. If you press a glass slide onto the affected area, the lupomas become the color of “apple jelly” (apple jelly symptom). With a favorable outcome, resorption begins in the center of the tubercles and replacement of the damage with thin skin in the form of tissue paper.
Rice. 5. Photo of lupoma.
Rice. 6. Symptom of “apple jelly” in tuberculous lupus
Rice. 7. Lupus vulgaris.
Rice. 8. Consequences of Lupus vulgaris.
Forms of tuberculous lupus
Tuberculous lupus of the mucous membranes
The most severe form of Lupus vulgaris. The disease affects the mucous membranes of the nose, eyes and mouth. Initially, red-yellow formations (plaques) appear on them. Their surface has a grainy appearance, reminiscent of fish eggs. Over time, the process affects the cartilage of the nose and ears. Next comes spontaneous rejection of damaged dead tissue, which ends in permanent facial disfigurement.
Rice. 9. The photo shows a lesion of the tongue due to tuberculous lupus.
Rice. 10. Damage to the oral mucosa.
Tumor form of tuberculous lupus
Tuberculous tubercles merge, forming a tumor-like formation up to 3 cm in diameter. As the process progresses, a breakdown of the underlying tissue appears, accompanied by damage to the cartilage and lymph nodes.
Rice. 11. The photo shows a tumor form of tuberculous lupus.
Flat form of tuberculous lupus
Tuberculosis foci merge, but the affected area does not protrude above the level of the skin. As the disease progresses, ulcers appear with uneven edges and a granular bottom.
Rice. 12. Flat shape of Lupus vulgaris.
Psoriatic form of tuberculous lupus
Tuberculosis foci merge. The surface of the damage is covered with many small scales.
Rice. 13. Psoriatic form of Lupus vulgaris.
Rice. 14. Psoriatic form of Lupus vulgaris.
Exfoliative (scaly) form of tuberculous lupus
Tuberculosis foci merge. The surface of the damage is covered with many large whitish scales, which adhere tightly to the underlying tissues. The appearance of the lesion resembles a butterfly.
Rice. 15. Exfoliative (scaly) form of Lupus vulgaris.
Rice. 16. Exfoliative (scaly) form of tuberculous lupus.
Rice. 17. Exfoliative (scaly) form of tuberculous lupus.
Sarcoid-like form of tuberculous lupus
Merging, tuberculosis foci form tumor-like formations of a reddish color - lupus carcinoma. The process is prone to malignancy.
Tuberculous lupus is the most common form of cutaneous tuberculosis. It is characterized by a chronic, slow progressive course and a tendency to melt tissue. The disease usually begins in childhood and lasts for years or decades, sometimes throughout life.
Clinical picture
Tuberculous lupus is most often localized on the face, especially on the nose (in 80% of cases), cheeks, upper lip, less often on the neck, torso, extremities, and often on the mucous membranes (70% of patients). Pulmonary tuberculosis is found in 5-10% of lupus patients, and tuberculosis of bones and joints occurs with the same frequency. Skin infection occurs predominantly by hematogenous or lymphogenous route.
The disease begins with the appearance of lumps - tubercles ranging in size from a pinhead to a pea, brown-reddish in color with a yellowish-brown tint, soft, doughy consistency with a smooth, slightly shiny surface. Lupoms are poured out in a group, at first they are located in isolation, then they merge; along their periphery there is always a stagnant-hyperemic zone.
The “apple jelly” phenomenon (diaskopia, obelmus). If you press a glass slide onto the lesion, yellow-brown spots appear. This symptom is explained by the squeezing out of blood from dilated blood capillaries and the transmission through the epidermis of magnifying glass with a granulomatous structure
“Probe” symptom (Pospelov’s sign). If you press a button-shaped probe on the tubercle (lupu), then it is easily immersed into the depths of the tissue. In this case, light bleeding and minor pain occur. The symptom is more pronounced with fresh lupoma. This occurs due to caseous necrosis, accompanied by the death of collagen and elastic fibers.
There are several clinical forms of tuberculous lupus: macular (Lupus planus maculosus), tubercular (Lupus planus tuberculosus), tumorous lupus (Lupus tumidus), erythematous, squamous-hyperkeratotic, verrucous and ulcerative.
- In some cases, destructive ulcerative changes involve deep underlying tissues (cartilage, bones, joints) in the process with the formation of mutilations, fibrous, keloid scars and disfigurement of the nose, ears, fingers, eyelids, limbs (Lupus mutilans).
- When the mucous membranes are affected (Tuberculosis luposa mucosae), small bluish-red tubercles the size of a millet grain are formed, which, due to their close grouping, give the affected area a peculiar granular appearance. Diagnosis is facilitated by the simultaneous presence of manifestations on the skin. When the mucous membranes of the nose are damaged, a soft, lumpy, bluish infiltrate is formed, which disintegrates to form an easily bleeding ulcer.
- Pityriasiform lupus (Lupus vulgaris pityriasiformis) is characterized by pithiarisiform scaling, and lupus psoriasiformis (Lupus vulgaris psoriasiformis) is characterized by silvery-white scales.
- There are other types of the disease: serpiginating, exfoliative, rupioid, crustose, etc.
Tuberculous lupus can be complicated by erysipelas, lymphangitis, pyoderma, and the development of skin cancer (Lupus carcinoma).
Histologically, epitheloid and giant cells surrounded by lymphocytes are detected in the dermis. Giant Langhans cells are located in the central part of the tubercle, in the peripheral zone there are lymphocytes and plasma cells in large numbers; caseous necrosis is poorly expressed. Mycobacterium tuberculosis is detected with difficulty and in small quantities.
Diagnosis and differential diagnosis
Differential diagnosis is carried out with tubercular syphilis, tuberculoid form of leprosy, tuberculoid form of cutaneous leishmaniasis, actinomycosis, discoid form of lupus erythematosus.
Colliquatic cutaneous tuberculosis (scrofuloderma)
After tuberculous lupus, this form of skin tuberculosis is in second place in terms of frequency of the disease. It got its name from the Latin scrofulae - swollen lymph nodes of the neck and colliquescere - to melt. MBT enter the skin from infected lymph nodes through the lymphatic ducts. Cracks and ulcerations appear above the area of enlarged lymph nodes. The process is localized on the lateral parts of the neck, chest and collarbones. Young women are predominantly affected.
Symptoms of the disease
At the beginning of the disease, dense, painless nodules appear, which quickly increase in size, forming nodes tightly fused to the underlying tissues. Their sizes range from 3 to 5 cm. The skin over the lymph nodes acquires a bluish tint. Over time, the node becomes soft and opens. A cold abscess forms (suppuration without any manifestations of an inflammatory reaction). Pus with blood clots and pieces of destroyed (necrotic) tissue begins to be released from the fistula tracts. The ulcer has soft edges. The bottom of the ulcer is covered with a yellowish coating. Numerous granulations are visible. As the ulcer heals, irregularly shaped scars appear, which are connected by jumpers and bridges. The top of the scars is covered with papillary processes.
Rice. 18. Scrofuloderma.
Rice. 19. Scrofuloderma.
Rice. 20. Scrofuloderma.
Journal "Emergency Medicine" 7-8 (46-47) 2012
Skin tuberculosis is one of the manifestations of tuberculosis disease in the body and is caused by mycobacterium tuberculosis of both human (Mycobacterium tuberculosis) and bovine species (Mycobacterium bovis) [1, 3, 4, 7, 8].
Tuberculous skin lesions are a fairly rare phenomenon; in the structure of the incidence of tuberculosis it is less than 0.1% [2, 4, 5, 8].
Skin tuberculosis occurs against the background of altered reactivity and a reduced immunobiological state of the body; spreads predominantly endogenously (hematogenously or lymphohematogenously) from other foci of tuberculosis infection in the body (lungs, lymph nodes, etc.); may be combined with other localizations of the tuberculosis process [1, 4, 6].
Histologically, in tuberculosis, granulomas of epithelioid cells surrounded by lymphocytes are detected in the skin. Characteristically, there are giant Langhans cells and caseous necrosis in the center of the tubercle. Mycobacteria may also be detected.
Dermatological forms of tuberculosis include pathological processes that vary in clinical picture.
Diagnosis of all forms of skin tuberculosis is based on clinical data, the results of an X-ray examination, histological examination of a biopsy specimen, determination of tuberculin allergy, as well as the effectiveness of test therapy [1, 4, 6].
Classification of skin tuberculosis:
I. Chronically current primary tuberculosis:
1) collicative tuberculosis: primary scrofuloderma, secondary scrofuloderma, fungal tuberculosis;
2) diffuse forms of skin tuberculosis: papulonecrotic tuberculosis, indurated erythema, lichen scrofulus.
II. Secondary tuberculosis:
1) tuberculous lupus (flat, ulcerative, hypertrophic, papillomatous);
2) warty skin tuberculosis;
3) miliary ulcerative tuberculosis of the skin.
Colliquatic cutaneous tuberculosis (scrofuloderma) is the second most common form of cutaneous tuberculosis.
The lateral surfaces of the neck are most often affected.
The rashes are initially represented by dense, painless nodules, which, quickly increasing in volume, turn into a node tightly fused to the underlying tissues. The skin above it acquires a bluish tint. Subsequently, the node softens and opens with the release of purulent contents with inclusions of necrotic tissue. At the site of the node, an ulcer forms with soft edges, a yellowish coating and flaccid granulations at the bottom. After its healing, very characteristic ragged scars of irregular shape remain, covered with papillary skin outgrowths and bridges (Fig. 1). The lateral surfaces of the neck are most often affected. Mostly women are affected.
Tuberculosis of the skin is papulonecrotic. Papulonecrotic tuberculosis of the skin most often affects women aged 16 to 40 years, but elderly and senile patients, as well as children, are also found. Persons whose work involves being on their feet for a long time are more susceptible to the disease.
This form of skin tuberculosis is characterized by hemispherical papules the size of a hemp seed, reddish in color with a bluish tint, and dense in consistency. Necrosis occurs in the central part of the papule. Necrotic masses shrink into a tight crust, after removal of which a round ulcer with steep edges is formed (Fig. 2). After its healing, a characteristic depressed, or “stamped” scar remains. The scar itself and the skin around it are hyperpigmented, but depigmentation occurs over time. The evolution of an individual papule lasts about a month.
With papulonecrotic tuberculosis of the skin, any area of the skin is affected, but the favorite localizations are the legs, buttocks, thighs, forearms and shoulders. The largest number of papules is detected in the area of the legs, buttocks, thighs and forearms. Typically, the rash is grouped in the joint area along the extensor surfaces of the limbs (Fig. 3).
Histologically, central necrosis is detected, surrounded by a nonspecific and peripherally granulomatous infiltrate. Vascular changes are evident.
The course of the disease is chronic, worsening in winter and improving in the warm season. However, due to hyperinsolation, exacerbation may occur in summer. Tuberculin tests are positive. Mycobacterium tuberculosis is found in isolated cases. During the outbreak, signs of intoxication may appear with increased body temperature, malaise, and joint pain. The prognosis is favorable. The primary focus (in the lungs, lymph nodes, bones and joints) is often inactive. Between exacerbations, the general condition of patients usually does not change.
Indurated erythema (syn.: erythema induration of Bazin, indurative tuberculosis of the skin). This is one of the most common forms of skin tuberculosis. The basis of the disease is dermohypodermal allergic vasculitis, caused by increased sensitivity to mycobacteria, which enter the skin mainly hematogenously. The disease develops mainly in girls and young women suffering from peripheral circulatory disorders, hormonal dysfunctions, primarily hypofunction of the gonads. The provoking factor is prolonged standing.
Erythema induratum of Bazin is manifested by nodes, usually located in the subcutaneous fatty tissue of the legs, reddened skin over them, mainly in women with inactive tuberculous lesions of the lymph nodes. The nodes resolve spontaneously in the summer and recur in the spring and autumn.
The size of the nodes in most cases reaches the size of a cherry or a small plum, less often - a chicken egg; in some patients, a flat infiltrate is palpable (Fig. 4).
Histologically, a granulomatous, nonspecific, lymphocytic-plasma cell inflammatory reaction, significant vascular changes with swelling and proliferation of the endothelium, thrombosis and obliteration of the lumens are initially detected. Subsequently (after 1.5–2 months), a specific granulomatous reaction is formed. Caseosis is not always observed. A deep biopsy is important for diagnosis, since the main process develops in the subcutaneous tissue.
The prognosis for recovery is favorable, although even with adequate treatment, regression occurs slowly. Late relapses may occur, sometimes several years after clinical recovery. The course is long. Ulceration of the compaction focus is rarely observed, which proceeds torpidly and is resistant to therapy.
Lichen scrofulous (lichenoid tuberculosis of the skin). A very rare form of cutaneous tuberculosis, usually developing in the primary period of the disease, mainly in weakened children and adolescents suffering from other forms of tuberculosis (skin, lymph nodes, bones or, less commonly, lungs). The development of the disease is provoked by acute infections (measles, whooping cough, influenza, etc.), sometimes a tuberculin test, as well as BCG vaccination.
Rashes in the form of lichenoid, follicular or perifollicular elements of a cone-shaped or flat shape, round, less often polygonal in outline, often with horny scales on the surface or penetrated by vellus hair. They are located symmetrically, mainly in the area of the lateral surfaces of the body. Their color is yellowish-brown, reddish or pale pink. Due to grouping and close arrangement, oval or ring-shaped lesions may occur. Less common are erythematous rash, infiltrative foci, elements that seem to be transitional to papulonecrotic tuberculosis, or a combination of these forms. When elements regress, surface scars may remain (Fig. 5).
Histologically, predominantly epithelioid cell granulomas are found, located perifollicularly, with a small lymphocytic reaction and a few giant cells.
The course of the disease is chronic. The prognosis is favorable due to the tendency to spontaneous regression within a few weeks from the moment of onset or the rapid effect of treatment, however, relapses are possible, more often in the fall and spring.
Tuberculous lupus (lupus vulgaris) is the most common form of skin tuberculosis. The pathogen enters the skin mainly lympho- or hematogenously from other foci of tuberculosis infection in the body (lungs, lymph nodes, etc.). Often combined with tuberculosis of peripheral lymph nodes (97%) and osteoarticular tuberculosis (30%).
The main morphological element is a tubercle (lupoma), which is an infectious granuloma. The diameter of the tubercles is 2–7 mm, the consistency is dense-elastic, palpation is painless. The tubercles are prone to peripheral growth, fusion to form solid foci and ulceration. Their peculiarity is resolution with the obligatory formation of a thin, smooth, superficial scar or cicatricial atrophy of the skin. With diascopy, the brownish-pink color of the tubercles disappears; as a result of anemia of the pathological area, tuberculoid infiltrates of a yellowish-brown color become visible (the “apple jelly” phenomenon) (Fig. 6).
When a button-shaped probe is pressed on the lupus tubercles, it easily penetrates the lupoma tissue (probe phenomenon).
There are: flat, ulcerative, psoriasiform, tumor-like, serpiginating, verrucous, disseminated and other forms of tuberculous lupus. A combination of one or more forms (usually flat and ulcerative) in the same patient is possible.
The rash is usually localized on the face, but can also be on the torso and limbs. The mucous membrane of the nasal cavity and mouth is often affected.
More often registered in women. Sometimes it develops after BCG vaccination or some time later at the site of a post-vaccination scar. It is characterized by a sluggish, long-lasting and benign course. Tuberculous lupus usually occurs against the background of a normergic reaction to the Mantoux test with 2 TU.
The most common form of lupus is flat, in which individual tubercles merge with each other, forming a lesion that increases as a result of the appearance of new tubercles along the periphery (Fig. 7).
The ulcerative form of tuberculous lupus occurs due to ulceration of the tubercles. The ulcers are superficial, bleed easily, and may be covered with a small purulent discharge (Fig. 8).
Psoriasiform tuberculous lupus resembles a psoriatic plaque. It is characterized by the presence of silvery-white scales on the surface of the lesions (Fig. 9).
The tumor-like form of tuberculous lupus is formed by the fusion of large tubercles into a continuous infiltrative tumor-like conglomerate of dark brown color, which simultaneously retains all the typical signs of tuberculous tubercles (pastyness, symptoms of “apple jelly” and “probe retraction”) (Fig. 10).
In addition to the skin, tuberculous lupus can often (up to 70% of cases) be observed on the mucous membranes. Most often the nasal cavity and oral cavity are affected (gums, hard and soft palate, pharynx, lips, etc.). This is characterized by the appearance of small, grayish-reddish tubercles that tend to merge to form plaques with an uneven surface. In the process of further evolution, they disintegrate with the formation of ulcers. Ulcers most often have irregular, finely scalloped, uncut edges, surrounded by an edematous-inflammatory rim, on which it is often easy to notice the still undisintegrated (i.e., younger) lupus tubercles. The bottom of the ulcers usually has a granular appearance, is covered with islands of yellowish-gray plaque and bleeds relatively easily.
When the ulcerative process spreads deeper, cartilage and bone tissue may be affected; this often leads to facial deformation (especially the nose, lips, upper jaw, eyelids, ears). If the gums are damaged and the bone part of the alveoli is involved in the pathological process, exposure and even loss of teeth are possible (Fig. 11).
Serpiginating lupus is characterized by the tendency of the process to spread to adjacent healthy areas of the skin; at the same time, a scar is formed on the regressed areas of the lesion, along the periphery of which new lupomas appear (Fig. 12).
The warty (verrucous) form of tuberculous lupus is characterized by the appearance of warty growths on its surface; most often observed on the hands and feet (Fig. 13).
Ordinary tuberculous lupus always ends with the formation of a scar. During relapses of the disease, a characteristic feature of tuberculous lupus is the formation of new lupomas on the scars.
The most severe complication of tuberculous lupus, which develops in most cases as a result of irrational treatment (especially radiation), is lupus-carcinoma, which is more severe than ordinary squamous cell carcinoma (Fig. 14).
Miliary ulcerative cutaneous tuberculosis is a very rare form of cutaneous tuberculosis. It is characterized by the appearance, most often on the face, of small pinkish-brown soft nodules, which can ulcerate and heal with the formation of a scar or resolve without ulceration (Fig. 15).
Clinical examples
Patient P., 25 years old.
At the age of 11 years, the patient developed changes in her skin, for which she was haphazardly treated with antibiotics and immunomodulators without effect (a slight improvement was noted only during treatment with rifampicin). The disease progressed steadily and became generalized, affecting the skin of the abdomen, mammary glands, back, and thighs (Fig. 16).
Biopsy, histological conclusion - skin tuberculosis (Fig. 17).
X-ray examination, including a computed tomogram, revealed a Ghon lesion in S10 of the right lung (Fig. 18).
The reaction to the Mantoux test with 2 TE is positive - papule 16 mm (Fig. 19).
Clinical diagnosis: papulonecrotic tuberculosis of the skin.
The patient was treated with antimycobacterial drugs in category 1 (2 HRZE 4 HR) for 6 months.
As a result of treatment, significant resorption of papular changes on the skin was achieved (Fig. 20).
Patient Ch., 57 years old.
After sunbathing, changes appeared on the skin of the chest in the form of raised ring-shaped papules, like a necklace with stretched rings. I contacted a dermatologist. As a result of examination of scrapings of the affected area of the skin, a fungal infection was rejected. The examination was interrupted. A year later, the rashes increased (Fig. 21).
A biopsy of the affected skin on the right forearm was performed and granulomatous tissue with Pirogov-Langhans cells was identified.
Conclusion: skin tuberculosis (tuberculous lupus, flat form).
Hospitalized in the anti-tuberculosis dispensary.
Clinical analysis of blood and urine is unremarkable.
Sputum analysis: MBT not detected.
Reaction to the Mantoux test with 2 TE: papule 14 mm.
A plain X-ray of the chest organs revealed no pathology (Fig. 22).
A CT scan of the chest revealed calcifications in the intrathoracic and left bronchopulmonary lymph nodes (Fig. 23).
The main course (6 months) of antimycobacterial therapy was carried out with a positive clinical effect in the form of significant resorption of changes on the skin (Fig. 24).
Ulcerative skin tuberculosis (Tuberculosis cutis ulcerosa)
The disease most often affects men who already had tuberculosis of internal organs. Tuberculosis bacilli enter the skin from the urine, feces or sputum of the patient himself, affecting areas of natural external openings: the skin around the anus, glans penis, nose, area around the mouth, mucous membrane of the tongue.
Symptoms of the disease
Merging, tuberculous tubercles form small yellowish nodules. Over time, the nodules suppurate and open with the formation of painful ulcers that make natural acts difficult.
The ulcers have soft, undermined edges. The color of the ulcers is pale red. The size of the ulcers is up to 1.5 cm, the bottom is granular. Javas often bleed. Sharply painful. As the disease progresses, tuberculous tubercles reappear at the bottom of the ulcers and around them. The tissues are destroyed, forming yellowish microabscesses, the so-called “Trel grains”, containing a large amount of MBT. The disease is difficult. Ulcers heal slowly. In their place, thin scars form, located below the skin level (atrophic scars).
Rice. 21. Ulcerative tuberculosis.
Types of skin tuberculosis
Today, there are two forms of skin tuberculosis - disseminated and focal. Each of them differs in course, causes and methods of treatment.
Collicative tuberculosis of the skin
This form appears mainly in people already suffering from tuberculosis of the lymphatic subcutaneous nodes. It is from them that bacteria get under the skin and provoke a secondary disease. With collicvative tuberculosis of the skin (scrofuloderma), symptoms appear on the neck, limbs and jaws. Initially, small and painless nodes appear, which lie in the deep layers of the epidermis and quite quickly increase in size. The skin then takes on a bluish tint and begins to soften right in the center of the spots, forming a continuous bleeding ulcer. In some cases, necrotic tissue departs from the fistula tracts. After the ulcers heal, “ragged” scars remain in their place.
Scrofuloderma is observed only in childhood or adolescence. The prognosis for recovery is favorable, provided that the development of the disease has not reached the ulcerative process. Otherwise, the prognosis may be disappointing. For treatment, special anti-tuberculosis drugs and ultraviolet rays are used.
Miliary ulcerative tuberculosis
Appears against the background of existing tuberculosis of the liver, lungs or intestines. With feces, sputum or urine, bacteria penetrate the skin and infect the mucous membranes. The lesions of this form are localized in the sphincter area, nose, and mouth; it appears most often in women. It is characterized by the appearance of small spherical compactions (papules), merging into single lesions and turning into bleeding ulcers. Ulcers are accompanied by severe pain (especially in cases where they are localized in the anus or genital area).
Due to the successful treatment in recent years of all forms of tuberculosis, ulcerative tuberculosis is very rare. The prognosis is favorable, and treatment is based primarily on the treatment of general tuberculosis. X-ray therapy is used, the lesions are treated with a solution of lactic acid. In isolated cases, surgical removal of the main lesion can be used.
Tuberculous lupus
This form of skin tuberculosis is considered the most common. A characteristic feature is a chronic course with slow progression. There are often cases where the disease began in childhood and continued throughout life. In most cases, lesions are localized on the face: nose, cheeks, lips. Lesions of the trunk, limbs and mucous membranes are also found. The first signs of lupoid tuberculosis of the skin are small brown-red rashes. They are soft and smooth to the touch and only later begin to peel off. Lupomas are most often localized in groups at a distance from each other and can merge only with the course of the disease. If you press on the group with a magnifying glass, blood oozes out of them, and the empty holes have a yellowish tint.
In some cases, lupus tuberculosis may look like a tumor, especially when it is located on the tip of the nose or in the ear area. When the lupa disintegrates, large ulcers may form in their place. The disease can develop over many years with barely noticeable progression. Very often, tuberculous lupus can be complicated by skin cancer and erysipelas.
Treatment of this form is very specific and much depends on the clinical picture of the patient, ranging from light therapy to X-ray irradiation. In especially severe cases, surgical removal of the lesions can be used, but most often either liquid nitrogen or a lactic acid solution is used (when the lesions are located on the mucous membranes). The prognosis for tuberculous lupus is in most cases positive and largely depends on the patient’s body’s resistance, timely treatment and diet. But we must not forget that the disease is characterized by slow development and lack of progression, even in the absence of specialized treatment.
Warty skin tuberculosis
This form most often occurs in adults, predominantly in males. People with a specific profession are at risk:
- Slaughterhouse workers
- Pathologists
- Veterinarians
- Butchers
- Workers of medical institutions where there is direct contact with patients with active phases of tuberculosis.
A characteristic feature of warty tuberculosis is a rash in the form of a blue-red tubercle the size of a pea. The lesions are localized in the back of the bones and on the fingers, and in rare cases on the feet. In some cases, new plaques with warty formations may appear around the main focus, from which droplets of pus are released.
Diagnosis requires certain skills, since the clinical picture can be confused with pyoderma vegetans, blastomycosis and simple warts. Much attention is paid to lesions that have three features: a violet-red border, warty formations and an atrophic area of skin with a bumpy bottom. Treatment is carried out with anti-tuberculosis drugs, irradiation with X-rays, cleaning out lesions with a sharp spoon and cauterization.
Lichenoid tuberculosis of the skin
Most often observed in weakened children suffering from active tuberculosis of the lungs and lymph nodes. It may also develop as a result of treatment for tuberculous lupus. This form appears as rashes of a gray-reddish hue in the form of follicles or papules on the lateral parts of the body, face, buttocks and, in rare cases, on the mucous membranes of the lips. When the rashes are localized in a group, they can be confused with seborrheic eczema. Spontaneous appearance and disappearance are noted. Not accompanied by painful sensations, rough to the touch.
After complete cure of tuberculosis of the internal organs, almost all skin rashes disappear, in rare cases leaving behind small scars in the affected areas. Tuberculin tests are positive, so the diagnosis does not cause any complications. The prognosis is favorable, treatment is the same as for other forms of tuberculosis.
Warty skin tuberculosis (Tuberculosis cutis verrucosa)
Warty skin tuberculosis occurs among veterinarians and slaughterhouse workers who come into contact with the corpses of animals with tuberculosis. This form of the disease is rare. The skin of the back of the hand or feet is affected. The skin of patients is affected by tuberculosis from constant contact with infected sputum.
Symptoms of the disease
First, tubercles appear, the skin above which becomes bluish in color. Gradually, the tubercles merge with each other, forming dense infiltrates of a bluish color. Over time, they become covered with warty growths, dense scales and cracks. The lesion is surrounded by a bluish-red shaft, followed by a zone of shiny skin. During the healing process, the horny masses are rejected, and scars appear at the site of infiltration. The course of the disease is long-term.
Papulonecrotic tuberculosis of the skin (tuberculosis cutis papulo-nectrotica)
Papulonecrotic tuberculosis of the skin is more often recorded in young people. The disease is manifested by the appearance of papules, the size of which does not exceed 3 cm in diameter. The skin of the buttocks, abdomen, extensor surfaces of the limbs and chest is affected. The skin over the papules becomes pinkish-bluish in color. Over time, the papules become ulcerated. At the site of the ulcers, a grayish-white crust appears, which is replaced by a whitish scar.
Rice. 25. Tuberculosis cutis papulo-nectroticа. Multiple bluish-purple infiltrates and nodes on the legs.
Rice. 26. Papulonecrotic tuberculosis of the skin of the legs. Multiple bluish-purple infiltrates and nodes on the legs.
Rosacea-like Lewandowski tuberculosis
This form of the disease occurs as an allergic vasculitis. Erythema (redness) and telangiectasias (numerous dilated small vessels) appear on the skin of the face. Gradually the skin acquires a bluish-reddish tint. Rashes (tuberculids) are dense formations up to half a centimeter in diameter, without necrotic elements. During healing, atrophic scars form at the site of tuberculides.
Rice. 27. The photo shows Lewandowski’s rosacea-like tuberculosis.
Lichenoid tuberculosis of the skin (Tuberculosis cutis lichenoides seu lichen scrofulosorum)
Lichenoid tuberculosis of the skin often develops in weakened children, less often in adults with tuberculosis. The disease is manifested by the appearance of tubercles, which are covered with light gray scales. The tubercles are located symmetrically, most often on the skin of the abdomen and limbs. After healing, pigmentation or small scars remain at the site of the rash.
Rice. 28. The photo shows lichenoid tuberculosis of the skin.
Reasons for appearance
Today there is no clear and specific cause for the appearance of skin tuberculosis, but there are still a number of provoking factors. First, you need to pay attention that healthy skin requires certain conditions for the disease to appear, since it is an unfavorable environment for tuberculosis microbacteria. People with the following problems are at risk:
- Endocrine system dysfunction
- Nervous system disorders
- Disorders of mineral and water metabolism
- Congestion of vascular origin
Social factors also play an important role: living conditions, environmental factors and nutrition. Climatic conditions are no less important - lack of sunlight and dampness can become provoking factors in the development of the disease.
Indurative tuberculosis of the skin (indurated erythema)
This form of the disease manifests itself in 2 varieties - Bazin's erythema nodosum and Hutchinson's ulcerative erythema. The disease often affects patients with tuberculosis of internal organs.
Erythema nodosum of Bazin
The disease is more often registered in women aged 16 to 40 years. Dense nodes or flat, extensive infiltrates that appear on the skin of the legs, thighs, buttocks and upper extremities are bluish-red in color. The size of the seals is 3 – 8 cm. Seals and infiltrates are often located symmetrically, in the deep layers of the skin and subcutaneous fatty tissue. With regression of tuberculous elements, ring-shaped atrophic areas and pigmentation remain.
Hutchinson's ulcerative erythema
Sometimes the lesions merge, forming an extensive lesion with ulcerations in the center and dirty gray granulations. This form is named after the English dermatologist who first described it - Hutchinson's ulcerative erythema. Without treatment it lasts for a long time, sometimes even years. After healing, sunken pigmented scars remain.
Rice. 29. The photo shows indurative tuberculosis of the skin (indurated erythema of Bazin).
Rice. 30. Ulcerative erythema of Hutchinson.
Diagnosis of skin tuberculosis
Rice. 31. View of Mycobacterium tuberculosis in the light of a fluorescent microscope.
The diagnostic process consists of the following components:
- Bacteriological diagnosis (detection of MBT in discharge from ulcers and lymph node punctures).
- Diagnostic biopsy followed by histological examination, which allows to identify the morphological components of the tuberculous tubercle.
- Detection of tuberculosis of internal organs.
- Detection of scars on the skin as a result of a previous tuberculosis lesion.
- Tuberculin diagnostics.
- Trial treatment.
Diagnostic biopsy together with bacteriological examination is the most significant method in diagnosing tuberculosis.
Dermatologists are prescribed to detect skin tuberculosis. Knowledge of risk groups, which include patients in this category, early symptoms of the disease and diagnostic methods helps doctors to detect the disease in a timely manner.
Identification of the pathogen in the early stages of the disease will allow the patient to be successfully cured.
Tuberculosis in children
Early period of primary tuberculosis infection
The initial phase of interaction between the pathogen and the macroorganism lasts from 6 to 12 months from the moment the child is infected with Mycobacterium tuberculosis. During this period, there is an asymptomatic stage (about 6-8 weeks) and a turn of tuberculin tests - the transition of the Mantoux reaction from negative to positive for the first time. A child with severe tuberculin reactions should be referred to a phthisiatrician and monitored by a specialist for a year. In the future, such children remain infected with Mycobacterium tuberculosis or, under unfavorable conditions, develop one or another local form of tuberculosis.
Tuberculosis intoxication in children and adolescents
It is an intermediate form between primary infection and the development of a local tuberculosis process, determined by x-ray and other methods. The clinical course of this form of tuberculosis in children is characterized by nonspecific manifestations: malaise, irritability, loss of appetite, headache, tachycardia, dyspepsia, arrest or weight loss, and a tendency to intercurrent diseases (ARVI, bronchitis).
A long-term causeless low-grade fever is typical, against the background of which temperature candles appear up to 38-39 ° C; There is increased sweating, especially during sleep. Tuberculosis intoxication is accompanied by a specific reaction of the lymph nodes - their multiple enlargement (micropolyadenia).
If signs of tuberculosis intoxication in children persist for more than 1 year, the condition is regarded as chronic.
Primary tuberculosis complex
This form of tuberculosis in children is characterized by a triad of symptoms: the development of a specific inflammatory reaction at the site of infection, lymphangitis and damage to regional lymph nodes. It develops when a combination of massiveness and high virulence of tuberculosis infection with a decrease in the immunobiological properties of the body. The primary tuberculosis complex can be localized in the lung tissue (95%), intestines, and less commonly in the skin, tonsils, nasal mucosa, and middle ear.
The disease can begin acutely or subacutely; masquerade as influenza, acute pneumonia, pleurisy, or be asymptomatic. Clinical manifestations include intoxication syndrome, low-grade fever, cough, shortness of breath. Changes in the primary lesion go through an infiltrative phase, a phase of resorption, compaction and calcification (formation of a Gohn's lesion).
Tuberculous bronchoadenitis
Bronchoadenitis or tuberculosis of the intrathoracic lymph nodes in children occurs with specific changes in the lymph nodes of the root of the lung and mediastinum. The frequency of this clinical form of tuberculosis in children reaches 75-80%.
In addition to low-grade fever and symptoms of intoxication, the child develops pain between the shoulder blades, whooping cough or bitonic cough, expiratory stridor, caused by compression of the enlarged intrathoracic lymph nodes of the trachea and bronchi. Upon examination, attention is drawn to the expansion of the subcutaneous venous network in the upper chest and back.
Complications of tuberculous bronchoadenitis in children may include endobronchitis, atelectasis or pulmonary emphysema. This clinical variant of tuberculosis in children requires differentiation from Beck's sarcoidosis, lymphogranulomatosis, lymphosarcoma, and nonspecific inflammatory adenopathy.