A study aimed at detecting the genetic material (DNA) of the human papillomavirus of high carcinogenic risk with genotyping of 16 and 18 types of the virus. 14 HPV genotypes are detected based on the polymerase chain method in real time with multiplex detection (Roche Cobas 4800).
Synonyms Russian
Human papillomavirus of high carcinogenic risk; HPV of high carcinogenic risk; DNA [real-time polymerase chain reaction, Roche Cobas 4800].
English synonyms
Human Papillomavirus; HPV; high carcinogenic risk; DNA.
What biomaterial can be used for research?
A smear mixed from the cervical canal and the surface of the cervix.
General information about the study
Human papillomavirus (HPV or HPV) is a family of DNA viruses that cause various lesions of the skin and mucous membranes of humans. More than 100 types of HPV are known, which can be associated with the appearance of warts, papillomas, genital and flat condylomas, precancerous changes (dysplasias) and cancer of the cervix, vagina, vulva, rectal cancer, penis and neoplasms of some other localizations (for example, oropharyngeal carcinoma). The source of infection is a sick person or a virus carrier. The main route of transmission of infection is sexual intercourse. Infection through common household items and vertical transmission, from an infected woman to a child during pregnancy or childbirth, is also possible.
There are HPV genotypes, infection of which leads to the development of benign processes, and those that have a high risk of malignant degeneration. HPV genotypes 1, 2, 3, 4, 5, 10, 28, 49 are non-oncogenic; genotypes 6, 11, 13, 32, 34, 40, 41, 42, 43, 44 have a low oncogenic risk; genotypes 26, 30, 53, 65 have an average oncogenic risk; genotypes 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 belong to HPV of high carcinogenic risk and 66, 68 belong to types of probable risk for humans. The genome of oncogenic HPV types contains regions responsible for the synthesis of certain proteins. Oncoproteins E6 and E7 suppress the processes of apoptosis (programmed cell death) in cells with altered genetic material. They play a large role in the development of malignant tumor processes. Regions of the genome L1 and L2 are responsible for the synthesis of structural proteins of the capsid shell of the virus.
Infection with highly oncogenic HPV types may be associated with the development of cervical intraepithelial neoplasia (CIN) and cervical cancer in women. Cervical cancer ranks third in the structure of the incidence of malignant neoplasms among women in Russia. In most cases, 90%, the oncological process is represented by squamous cell carcinoma, less often by other histological variants (adenocarcinoma and adenosquamous cell carcinoma). Long-term persistence of the virus and high levels of virus content may be associated with the severity of the disease.
The main method of screening for cervical cancer and precancerous conditions is a Papanicolaou cytology test (Pap smear). According to generally accepted recommendations, it is performed on all women over the age of 21, regardless of the age of onset of sexual activity, with an interval of 3 years until the age of 65. For women aged 30-65 years, an alternative screening program can be used at 5-year intervals, involving simultaneous two tests: Pap cytology and HPV DNA testing using the polymerase chain reaction method. It should be noted that at a young age, HPV can be spontaneously eliminated from the body and cannot be detected using modern methods. Moreover, in 70% of cases during the first year and in 90% of cases two years after infection, self-healing is possible.
The use of combined diagnostics (cytological examination and DNA testing) increases the efficiency of detection of precancerous conditions, grade 2 and 3 CIN, and cervical cancer.
Modern diagnostic methods include the real-time polymerase chain reaction method (real-time PCR). Polymerase chain reaction is a molecular diagnostic method that allows one to identify the genetic material of the pathogen under study. It is characterized by high rates of diagnostic sensitivity and specificity, speed of obtaining the final result and accessibility. A special feature of the method is the ability to detect bacterial DNA even when its content is low in the biological material being studied. The method is based on a multiple increase in the number of copies of a DNA region specific to a given pathogen.
The Roche Cobas 4800 analyzer and test system combines automated sample preparation and detection of 14 HPV genotypes based on real-time PCR with multiplex detection. This allows genotyping and determination of the presence of HPV 16 and HPV 18, as well as a pool of 12 HPV types with high carcinogenic risk (31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68). Human β-globin is used as an internal reaction control. The use of the Roche Cobas 4800 real-time PCR method for screening determination of HPV genotypes with high carcinogenic risk is recommended, tested and clinically proven. The use of this diagnostic method makes it possible to simultaneously genotype the virus for HPV 16 and HPV 18. These types of virus are among the most carcinogenic and are associated with a clinically significant risk of developing grade 3 CIN or cervical cancer. The HPV 16 genotype is more common in squamous cell carcinoma, and HPV 18 in adenocarcinoma. Thus, it is possible to identify HPV genotypes of high carcinogenic risk, predict the risk of developing infection, CIN and cervical cancer, as well as determine tactics, monitor therapy and assess the possibility of relapse after treatment.
What is the research used for?
- To assess the risk of developing processes and diseases associated with HPV: cervical intraepithelial neoplasia (CIN grades 2 and 3) and cervical, vaginal, vulvar cancer, rectal cancer, oropharyngeal carcinoma;
- For screening diagnosis of HPV genotypes of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68);
- For differential diagnosis and genotyping of HPV 16 and 18, with determination of the DNA concentration of these types of virus;
- To monitor HPV infection and predict its course;
- To monitor the effectiveness of treatment of precancerous diseases associated with HPV;
- To determine tactics, monitor therapy and assess the possibility of relapse after treatment
When is the study scheduled?
- With clinical manifestations and suspicion of the development of an oncological process in the anogenital area;
- In the presence of condylomas, warts of the genital tract and other morphological changes in the epithelium of various localizations;
- When screening for cervical cancer in women over 30 years of age as part of a combined diagnosis (cytological examination and DNA testing using the polymerase chain reaction method);
- When HPV of an unspecified genotype is detected;
- When detecting cytological changes in a smear for atypia, during a cytological examination of a Papanicolaou smear, in a histological specimen;
- When monitoring those infected with HPV;
- In the treatment of cancer and precancerous conditions associated with HPV;
- When determining tactics, monitoring therapy and assessing the possibility of relapse after treatment.
What do the results mean?
Reference values
| Reference values | |
| HPV DNA type 16 | Not detected |
| HPV DNA type 18 | Not detected |
| HPV DNA types 31-68 | Not detected |
Reasons for the positive result:
- Infection with HPV of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 genotypes);
- Increased concentration of HPV DNA of 16 and/or 18 genotypes.
Reasons for negative results:
- Absence of infection and genetic material of HPV of high carcinogenic risk in the studied biomaterial.
Human papillomavirus type 18, HPV DNA 18 t.
Human papillomavirus type 18, HPV 18
— qualitative detection of human papillomavirus of high oncogenic risk in scrapings of the urogenital tract using the polymerase chain reaction method with real-time detection. The PCR method with real-time detection of results allows you to determine the amount of DNA of clinically significant HPV types in a sample.
Human papillomavirus (HPV)
is a widespread infectious disease of the genitourinary organs, which can cause cervical cancer in women and squamous cell carcinoma in men.
Different types of HPV cause the development of:
- cervical, vulval, vaginal dysplasia of the cervix;
- pre-invasive and invasive cancer of the cervix, cancer of the vagina and perianal area;
- genital warts, urinary tract;
- genital warts.
Routes of spread of infection
The main route of transmission of HPV is sexual, but cases of household transmission of infection have been described. Women and men are infected at the same rate. In approximately 70% of those examined, HPV is detected in both sexual partners. Intrauterine infection is possible.
According to some researchers, the frequency of infection with the virus is directly proportional to the number of sexual partners: with one partner, HPV is detected in 17-20% of women, with 5 or more partners - in 70-80%.
Incubation period
The incubation period can last from 2 months to 2–10 years. HPV is characterized by a latent course of the disease, in which there are no clinical manifestations and no changes are detected during colposcopic, cytological and histological examination. In 30% of cases, the virus can be cleared within 6–12 months. Diagnosis of latent HPV infection is carried out only by PCR.
Clinical manifestations
HPV can affect the epithelium in different ways: contribute to the emergence of benign formations (papillomas, condylomas) or the combination of papillomavirus DNA with the cell gene, which leads to dysplasia and neoplasia, and subsequently to cancer. The most common area of cancer localization is the transition zone of the cervix to the cervical canal.
Clinical forms of human papillomavirus infection are found in 40–60% of men who are sexual partners of infected women. Their lesions are caused by the same types of HPV as women. In 2/3 of cases, characteristic rashes appear on the skin and mucous membranes of the genital organs.
HPV type 18 can cause cancer. HPV 18 causes cancer of the cervix, external genitalia, vagina, anal area, and flat condylomas. The danger of the disease is that its manifestations appear only a couple of months after infection. At the same time, type 18 develops and infects the body faster than type 16 virus.
Indications for the study:
- persons being tested for other STIs;
- women with a burdened obstetric and gynecological history - manifestations of transforming dysplasia to varying degrees;
- men according to clinical indications;
- weakened immunity;
- preventive screening studies.
With timely examination and proper treatment, the risk of degeneration of high-risk HPV cancer can be minimized. Preparation Men
Before taking a urogenital scraping, it is recommended to refrain from urinating for 1.5–2 hours.
Women
Submitting scrapings is not allowed on menstrual days. Avoid taking antibiotics for two weeks, and vaginal suppositories, tampons, spermicides three days before collection. One day before the test, you should not have sexual intercourse. You should not douche on the eve of the examination. After an ultrasound using a transvaginal probe, at least 48 hours must pass.
Interpretation of results
The format for issuing the result of HPV type 18 is detected/not detected.
Reasons for the positive result:
- the presence of HPV genotype 18 in the test material, which is associated with a high risk of developing cervical cancer and other neoplasms of the anogenital area.
Reasons for negative results:
- the absence of HPV genotype 18 in the test material, which does not exclude the possibility of infection with HPV of other genotypes.
What can influence the result?
- A false negative result is possible if the material is collected and stored incorrectly, as well as if the virus content in the material is below a detectable level.
- A false positive result may be due to contamination of the material.
Important Notes
- HPV infection does not always lead to cervical cancer.
- Simultaneous infection with several HPV genotypes is possible.
- The result of the analysis must be interpreted taking into account the conclusions of cytological and histological studies.
Human papillomavirus, HPV, human papillomavirus, HPV
PVI (human papillomavirus infection) is an infection caused by the human papillomavirus (HPV, human papillomavirus). It is one of the sexually transmitted infections. Infection is possible through sexual contact (vaginal, anal, oral sex), direct skin contact with affected organs. Children can become infected from an infected mother transplacentally or during childbirth (perinatal route of infection). Damage to trophoblast cells can lead to spontaneous abortion. Transmission of the virus from mother to fetus may result in laryngeal papillomatosis in the child.
The most common route of infection with HPV is sexually transmitted. Persons of both sexes are equally susceptible to infection. However, HPV causes the most serious damage in women. Men in most cases are asymptomatic carriers of the infection. In this case, the urethra, seminal fluid and prostate gland can serve as a reservoir for HPV. The probability of transmitting the virus during a single sexual contact reaches 80%. The peak of infection occurs in the age group of people from 16 to 30 years old, where the highest rates of HPV infection are recorded. Important epidemiological factors in the prevalence of this infection among young, sexually active people are the early onset of sexual activity and frequent changes of sexual partners.
Clinically, human papillomavirus infection is characterized by various lesions of the mucous membrane of the urogenital tract, causing the appearance on the skin and mucous membranes of the external genitalia, urethra, vagina, cervix and perianal area of exophytic (condylomas and genital warts, anogenital warts) or endophytic growths (lesions in the form of spots, intraepithelial neoplasia), being the main cause of malignant neoplasms. It has been proven that PVI underlies the pathogenesis of cervical cancer (CC) and anogenital cancer. On average, it takes up to 20 years from HPV infection to the development of precancer and cervical cancer.
A feature of human papillomavirus infection is its frequent course in a latent (latent) form. Moreover, this phenomenon does not depend on the gender of the patient. The incubation period can range from 2 months to 2-10 years. Clinical manifestations of human papillomavirus infection may be masked by symptoms of other sexually transmitted infections (STIs). According to WHO, 50-80% of the population is infected with HPV, but only 1-2% of individuals have clinical manifestations of human papillomavirus infection.
Infection with the papilloma virus itself is not a disease. The human body's immunological defense mechanisms can influence the course of the infectious process, and in most cases the immune system can cope with the virus within a year without any treatment. In such cases, spontaneous elimination of the virus and self-healing occurs. However, long-term consequences of HPV infection can include cervical cancer, vaginal and vulvar cancer, anal cancer, penile cancer and, less commonly, other types of cancer.
Human papillomavirus (HPV) is a DNA virus that has oncogenic potential and selectively affects the epithelium of the skin and mucous membranes. The main target of exposure is the basal epithelial cells in the transformation zone of the cervix (transition zone of the cervix). The virus multiplies in the nuclei of infected cells and integrates into the cellular genome, causing its instability. As a result of infection, the normal process of differentiation in epithelial cells is disrupted, resulting in dysplastic changes, the progressive development of which leads to cancer.
HPV types. To date, more than 300 different types of papillomaviruses are known. That is, this is a widespread heterogeneous group of viruses that differ in their oncogenic potential. Some of them have a predominantly productive effect on epithelial cells and are called low oncogenic risk types . For example, HPV types 6 and HPV 11 cause genital warts (genital warts) and are rarely associated with cervical tumors. Types of high oncogenic risk , for example, HPV 16, 18, 31, 33, 35, 39, 45, 52, 58, 59, 67, have a transforming effect on epithelial cells, leading to the development of precancer (moderate and high-grade dysplasia H-SIL or CIN 2.3) and cancer.
Diagnosis of HPV. Since CC is a possible long-term result of a viral infection, and the danger comes only from a virus that exists in the body for a long time (more than a year), the basis of prevention is regular testing for HPV. Such an examination usually includes an examination of a cytological smear (Pap test, liquid cytology) in order to identify possible dysplastic changes in cells, as well as direct detection of the virus - an HPV test.
An HPV test is the detection of viral DNA in clinical material using a molecular biological research method - PCR diagnostics . The study allows us to identify a wide range of HPV genotypes associated with the development of cancer pathology and is carried out in two main formats. The first is a qualitative determination of HPV DNA with the result “detected” or “not detected.” The second is a quantitative HPV test - determining the exact amount of viral DNA in a scraping of epithelial cells with an assessment of the clinically significant amount of virus.
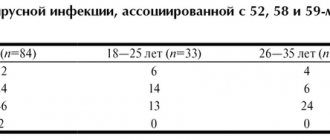
00513 HPV, HPV (Human Papillomavirus, human papillomavirus), types of high oncogenic risk: 16,18 with type indication, 16,18,31,33,35,39,45,52,67,58,59 without type indication (definition in material using PCR method)
00680 HPV (Human Papillomavirus, human papillomavirus), determination of phylogenetic groups of the virus (16,18,31,33,35,39,45,51,52,56,58 59 types), quantitative determination of DNA (determination in the material by PCR)
00681 HPV (Human Papillomavirus, human papillomavirus), type 16/18, quantitative determination of DNA (determination in the material by PCR)
00218 HPV, HPV (Human Papillomavirus, human papillomavirus), types 16 and 18 (determination in the material by PCR)
Indications for the purpose of analysis: primary screening method in conjunction with cytological research methods; to resolve questionable results of a cytological smear; for monitoring the treatment of precancerous pathology of the cervix.
Material for research: scraping of epithelial cells of the mucous membrane of the cervix and cervical canal, scraping of epithelial cells from the surface of growths and ulcerations, scraping from the urethra.
Preparation for the study: it is advisable to take biomaterial before carrying out any diagnostic and therapeutic procedures, before taking antiviral and/or immunomodulatory drugs of synthetic or plant origin.
Women are recommended to take the test outside the menstrual cycle or 1-2 days after the end of menstruation. Within 24 hours before the examination, you should not use topical medications or douching. Before taking a scraping from the urethra, men are advised not to urinate for 1.5-2 hours before the procedure.
Research method: polymerase chain reaction (PCR) method.
Units of measurement: qualitative method:
positive/negative.
Quantitative method:
lg (HPV per 100 thousand cells).
Positive result:
DNA fragments specific to the human papillomavirus were found in the analyzed sample of biological material.
Negative result:
DNA fragments specific to human papillomavirus were not found in the analyzed sample of biological material. Important: a negative PCR result cannot exclude the presence of HPV infection.
Tags:
HPV, HPV, anogenital warts, dysplasia, cervical cancer (CC), clinical examination, condylomas, Pap smear, human papillomavirus, HPV types, HPV infection, Human Papillomavirus
Back to section