Last update: 02/21/2021
A type of chronic eczematous dermatitis, accompanied by symptoms of dyshidrosis (dehydration) of the skin, is called dyshidrotic eczema. The disease most often affects the hands and feet and occurs in both adults and children. Its manifestations are in many ways similar to other types of dermatitis, as well as fungal skin infections.
Causes
The exact mechanism of occurrence of this disease is not yet known. Until recently, it was believed that the main reason for its development was a malfunction of the sweat glands, but recent studies show that the occurrence of didyshidrotic eczema is possible even with their normal functioning. Among the factors that provoke the onset of symptoms of the disease are the following:
- nervous and physical stress
- contact with household chemicals and other substances that cause skin irritation
- hyperhidrosis - extremely intense sweating
- inherited predisposition to atopic dermatitis, bronchial asthma and other allergic diseases
- food and household allergens
Also of great importance are disturbances in the functioning of the immune and endocrine systems, nervous system, and metabolic disorders.
Symptoms of dyshidrotic eczema
The most characteristic manifestation of dyshidrotic eczema on the hands and other parts of the body is a vesicular rash - a rash consisting of many blisters with a diameter of up to 4-5 millimeters, filled with liquid contents. In this form of the disease, the blisters are located deep inside the epidermis and, as a result, cause severe itching. In some cases, it precedes the formation of bulk elements. The palms, backs of the hands, soles of the feet, and sides of the fingers are the most common sites for the rash.
Some time after the appearance, the vesicles burst, the contents flow out, and areas of ulceration appear at the site of the rash. When several bubbles are opened, erosions can combine. Gradually, the ulcers heal and become covered with yellowish or brown crusts. The process of formation of new rash elements, their opening and healing can last up to 3 weeks; after healing, an area of hyperpigmentation (darkening) remains at the site of erosion.
With a long course of the disease, a constant, chronic change in the structure and appearance of the skin occurs. The skin turns red and thickens, deep cracks form on it, and areas of peeling appear. Dyshidrotic eczema is also characterized by the formation of areas of dry, dehydrated skin, resembling wax paper in appearance.
The entry of pathogenic microorganisms (for example, streptococci) into cracks and ulcers causes secondary infection. At the same time, the symptoms also change: most often, pustules with purulent contents form on the surface of the skin, and purulent inflammation of the skin occurs. Soreness, swelling and redness occur, symptoms of general intoxication appear - headache, fever, in some cases - nausea, appetite and sleep disorders, enlarged lymph nodes (axillary, elbow, inguinal, popliteal).
Despite the fact that there are acute forms of the disease, most often didyshidrotic eczema occurs in a chronic form with relapses occurring from time to time. Remissions can last up to several months. Exacerbations do not always occur upon contact with allergens or irritating substances and can occur against the background of complete health.
Features of dyshidrosis in children
The cause of the development of dyshidrosis in childhood is considered to be burdened heredity and excessive mental stress, leading to a breakdown of the immune system. If dyshidrosis occurs in a breastfed child, the cause is poor nutrition of the mother. She needs to exclude from her diet foods that cause allergies (citrus fruits, confectionery, red berries, chocolate, etc.).
In children, true dyshidrosis and dyshidrotic eczema occur. The clinical picture of the disease is the same as in adults. It is worth paying attention to the fact that the child may scratch the itchy rash. This promotes the penetration of pathogenic microflora into the wound and increases the risk of developing infectious complications.
Diagnostics
Currently, there are no specific methods to accurately determine the disease. Its main signs are characteristic external manifestations; Dyshidrotic eczema is also indicated by the chronic nature of the disease. Among the diseases to exclude which differential diagnosis is carried out are contact dermatitis, fungal infections and palmoplantar psoriasis.
The main laboratory method of differential diagnosis is the examination of scrapings for the presence of pathogenic fungi. The contents of blisters and scrapings from areas of erosion are also used for research. This makes it possible to confirm the non-infectious origin of the disease, and in the presence of a secondary infection, to accurately select antibiotics to combat its causative agents.
Prevention and treatment of dyshidrotic eczema
When the first symptoms of the disease appear, you should immediately contact a dermatologist. Primary measures to combat eczema include following a hypoallergenic diet, from which the following components should be excluded:
- citrus
- chocolate
- nuts
- honey
- strawberry
- fish and other seafood
Of great importance is the elimination of contact with substances that irritate the skin - household chemicals, pollen,
wool, dust and other allergens. Tight shoes and synthetic socks for dyshidrotic foot eczema can also influence the development of the disease.
During the active period of the disease, which is accompanied by increased skin sensitivity and severe itching, lotions with 1% tannin solution, 2% boric acid solution, 0.25% silver nitrate solution, baths with 0.01-0.1% potassium permanganate solution are used, cindol solution 1-2 times a day for 4-7 days. The duration of local baths is from 15 to 25 minutes.
Drug therapy includes the use of the following:
- antihistamines and sedatives to relieve itching and swelling - Tavegil, Zyrtec, Suprastin
- ointments and other preparations based on corticosteroids - in severe cases of the disease to eliminate external symptoms; Long-term use of corticosteroids is not recommended due to the high risk of dependence and complications
- antiseptics - disinfectant solutions eliminate the risk of secondary infection
- antibiotics - used to prevent and treat fungal and bacterial infections in the form of ointments, tablets or injections
Some physiotherapeutic methods also have a beneficial effect on dyshidrotic eczema: laser, magnetic, cryotherapy, ultraphonophoresis, darsonvalization, ultraviolet irradiation, electrosleep, acupuncture.
Complications
The most common complication of dyshidrosis is skin infection. This occurs due to bacterial (usually staphylococcal) or fungal microflora entering open wounds formed due to scratching or opening of blisters. If treatment is not started on time, a more severe complication may develop - cellulitis. This is an inflammation of the subcutaneous fatty tissue involving regional lymph nodes.
The spread of infection is accompanied by:
- Rising body temperature.
- Signs of general intoxication (weakness, loss of appetite, body aches).
- Significant swelling and redness of the skin at the site of the lesion is detected.
- The pain intensifies.
Untreated cellulitis can lead to sepsis (general blood infection). If there are any signs of infection, you should immediately consult a doctor.
La-Cri remedies for dyshidrotic eczema on the hands and feet
La-Cri cosmetics based on medicinal plant extracts are widely used to eliminate the symptoms of the disease. They do not cause allergies and can be used for daily care even for children's skin. The range includes cleansers that remove impurities and reduce the risk of infection, as well as emulsions and creams that nourish and strengthen dry and damaged skin, reduce redness and itching, and promote accelerated healing of damaged skin.
Clinical researches
TM La-Cri products are recommended by the Union of Pediatricians of Russia. Clinical studies conducted by specialists have proven the high efficiency, safety and tolerability of products, including for daily skin care of children with mild and moderate forms of atopic dermatitis and during remission, accompanied by a decrease in the quality of life of patients. As a result of therapy, a decrease in the activity of the inflammatory process, a decrease in dryness, itching and flaking was noted.
Sources:
- Molochkova Yulia Vladimirovna, Dermatology. Brief reference book, publishing house: GEOTAR-Media, 2017
- Baumann Leslie, Cosmetic Dermatology. Principles and practice, publishing house: MEDpress-inform, 2016
- Ratner Desiri, Avram M.R., Avram M.M., Procedures in Dermatology. Clinical cosmetology, Publishing house: GEOTAR-Media, 2019
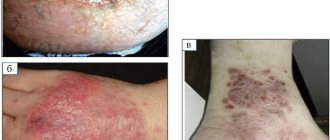
Photos of eczema
Photo album on the disease
Eczema is a widespread acute or chronic recurrent inflammatory skin disease, characterized by the appearance of vesicles on an erythematous background and developing with changes in skin reactivity. Eczema is the most common dermatological disease, the prevalence of which in different countries is about 5–20% of all calls for complaints about skin conditions.
One of the clinical variants of eczema is dyshidrotic, localized on the palmar surface of the hands, the lateral surface of the fingers and the plantar surface of the feet. The disease got its name because it was previously assumed to be associated with obstruction of the sweat glands, but it has now been proven that the sweat glands function normally in dyshidrotic eczema. Dyshidrotic eczema is mainly observed in young people, more often in women (age varies from 20 to 40 years) and develops, as a rule, in the puberty and postpartum periods.
Dyshidrotic eczema is characterized by the presence of a nonspecific pathological reaction of the skin, manifested by inflammation in the epidermis and dermis, which is typically characterized by the presence of focal swelling of the spinous layer of the epidermis - spongiosis. This reaction is traditionally called eczematous and takes part in the formation of the clinical picture of many non-infectious skin diseases. As a result of intensive scratching in dyshidrotic eczema, a secondary infection caused by bacterial and/or mycotic flora may occur.
In cases where, after eliminating the etiological factor, the manifestations of the disease resolve completely, they speak of allergic contact dermatitis. Factors that can provoke an exacerbation of allergic dermatitis are foci of chronic infection (including microbial contamination of the skin), dry skin or, conversely, excessive sweating, stress, adverse environmental factors (including inhaled, food and drug allergens), contact irritants. Most often, contact reactions are caused by metal ions (nickel, chromium, cobalt), ointment components (lanolin, local anesthetics, fragrances, parabens), paints, rubber, and occupational allergens. In most cases, after eliminating the allergen, the manifestations of the disease resolve. With prolonged and frequent exposure to the provoking factor, the symptoms of the disease do not go away completely, and the nature of its course becomes chronically recurrent. In the future, various factors acting both directly on the skin and on the body as a whole act as provoking exacerbations of the disease. In such cases, in Russia it is customary to talk about eczema as an independent nosological unit. However, abroad, eczema is usually considered as a synonym for the term “dermatitis”. This approach is reflected, in particular, in clinical dermatology guidelines, as well as in reference books for practicing physicians.
There is no common understanding of the term “hand eczema”. The disease is described as a chronic lesion of the skin of the hands, manifested by an eczematous reaction, which is characterized by polyvalent sensitivity, i.e. the development of relapses and exacerbations of the disease is associated with various effects both directly on the skin and on the body as a whole. However, the etiological and pathogenetic aspects of the development of eczema, covered in modern scientific publications, remain incompletely studied.
According to A.A. Kubanova et al., eczema is a multifactorial disease that develops on the basis of genetic predisposition, sensitization to various allergens, altered skin structure, immunological abnormalities and with the participation of endogenous and exogenous triggers. However, the mechanisms of development of immune abnormalities in the body as a whole and directly in the skin of patients during the development of various forms of eczema have not yet been definitively determined. Therefore, an integrated approach to studying the pathogenesis of eczema is necessary.
In the period from 1988 to 1999, the leading mechanisms for the development of dyshidrotic eczema were considered to be changes in cell membranes, metabolism, immune status, hemostasis and microcirculation. Imbalances in the balance of the body's pro- and antioxidant systems are closely related to the pathology of cell membranes and play a critical role in the pathogenesis of inflammatory skin diseases (Schmidt-Schonbein H., 1997). They have a pronounced effect on the rheological properties of blood, lead to pathological changes in the aggregation and deformability of cells and reduce their resistance to osmotic stress. Strengthening the processes of lipid peroxidation leads to the activation of factors of the prothrombin complex and inhibition of fibrin formation and fibrinolysis, disruption of the usefulness of the structure of the fibrin clot. The described processes cause hypercoagulable changes in the blood, which is an important factor in the pathogenesis of eczema. Along with the imbalance between lipid peroxidation and the activity of the antioxidant system in patients with eczema, changes in the microvasculature have been described (Prokhorenkov V.I., 1988). In patients, dilation and tortuosity of capillaries, venules, and slowing of blood flow in them were revealed; decreased circulation of tissue fluid between the epidermis and dermis; drop in filtration of tissue fluid from the interstitial space of the dermis into the blood and lymphatic capillaries.
A significant role in the development of hand eczema is currently attributed to disruption of the skin barrier, which is confirmed, in particular, by the positive results of using basic skin care products. During inflammation in the skin, the production and secretion of lipids by keratinocytes is disrupted. The consequence of this is an increase in intercellular spaces, a decrease in the elasticity of keratinocytes, which leads to an increase in the permeability of the skin barrier and the penetration of both allergens and irritants into the skin, further increasing inflammation. The emerging “vicious circle” ensures that the skin process becomes chronic.
Genetic factors are also important for the development of this dermatosis. In 50% of patients it is possible to identify a hereditary predisposition to allergic diseases. A positive association of histocompatibility system (HLA) antigens B22 and CW1 was established in patients with true eczema[/fn].
A significant role in the pathogenesis of eczema is played by changes in the state of prostaglandins and cyclic nucleotides, which occupy a central place in intracellular regulatory mechanisms, mediate neuroendocrine information, transform it into a specific cell response and implement normal and pathological reactions of the body. In patients with eczema, an increase in the concentration of prostaglandin F2a in the blood plasma was found. Prostaglandin F2a stimulates the synthesis of cGMP, which activates the production of histamine, serotonin and other allergy mediators, promotes the development of allergic and inflammatory reactions, and increases vascular permeability. The lack of prostaglandin E1 content, a violation of its ratio with the content of prostaglandin F2a leads to insufficient stimulation of the synthesis of cyclic adenosine monophosphate, which suppresses the formation of allergic and inflammatory reactions, the production of allergy mediators.
There are indications in the literature of exacerbation of dyshidrotic eczema of the hands after intravenous therapy with immunoglobulin G, which may be associated both with a reaction to the rapid increase in the level of immunoglobulin G in the blood, and with a reaction to the fillers and preservatives contained in the drug.
Along with the state of immune deficiency in patients with eczema, functional changes in the activity of the central nervous system, the predominance of the activity of unconditioned reflexes over the activity of conditioned reflexes, imbalances between the activities of the sympathetic and parasympathetic parts of the autonomic nervous system, changes in the functional state of skin receptors in the form of dissociation of skin sensitivity are noted. One of the main risk factors for the manifestation and exacerbation of eczema is a psychogenic effect, in which the stress-induced production of regulatory neuropeptides is included in the immune-inflammatory response, which ultimately leads to disruption of cytokine production and an imbalance in the cellular immune system, provoking immune inflammation.
One of the modern views on the pathogenesis of hand eczema is immunological. According to various authors, dyshidrotic eczema of the hands is considered a type of “true eczema”. At the same time, a significant number of patients have indications of manifestations of atopic dermatitis in early childhood and extracutaneous manifestations of atopy (atopic bronchial asthma, allergic rhinitis, hay fever). Apparently, in such cases it is more correct to talk about eczema as a limited variant of the adult form of atopic dermatitis. Often in the international literature, dyshidrotic eczema is called atopic eczema of the hands, and in some patients, during a comprehensive examination and observation, signs and characteristics are revealed that are very close to atopic dermatitis.
At the same time, at present, both among children and adults, there is a subgroup of patients with atopic dermatitis who have clinical manifestations that fit into the classical clinical concepts of this disease, but are not associated with hypersensitivity to allergens and exhibit normal levels of serum IgE antibodies. Their medical history does not indicate other atopic diseases, such as allergic asthma and rhinoconjunctivitis. These differences in the pathogenetic mechanisms leading to the development of atopiform (non-allergic, with a low level of IgE antibodies) and true (allergic, with a high level of IgE antibodies) types of atopic dermatitis remain insufficiently studied.
In general, as a result of numerous studies, the main components of the immunopathogenesis of atopic dermatitis have now been established as a disease with a clearly defined T-helper dependence, characterized in most cases by the dominance of T-helper type 2 and hyperproduction of IgE antibodies (exogenous type). At the same time, however, from the entire mass of patients, those who have an IgE-independent type of immune response (endogenous type) are clearly distinguished. Despite this immunopathogenetic heterogeneity, other characteristics of the disease, such as the main clinical features or, importantly, neuroimmunological relationships, remain poorly differentiated and common to almost all patients and still seem to be leading in the construction of therapeutic programs.
Attempts to classify allergic reactions and diseases that develop as a result of the development of these reactions have been made almost since the advent of the term “allergy” itself. At the moment, four types of allergic reactions are known: IgE-dependent, cytotoxic, immunocomplex and delayed, T-cell. The most fundamental difference between these manifestations of allergies is that only atopic diseases are characterized by a clearly visible hereditary predisposition, while in the case of drug and insect allergies such a connection, as shown by recent studies, does not exist. In addition, atopic diseases manifest themselves at a very early age, and their development is characterized by a certain sequence - the progression of various manifestations of allergies, starting from infancy and beyond, has been called the “allergic march”, and recently the term “allergic marathon” has been proposed, while how IgE-mediated manifestations of drug and insect allergies manifest in adulthood. Thus, there is an urgent need to revise existing approaches to the classification and nomenclature of allergies.
The modern classification and nomenclature of allergies was developed by a group of scientists on behalf of the European Academy of Allergy and Clinical Immunology (EAACI) and later refined with the participation of the World Allergy Organization (WAO, World Allergy Organization). An important point in the nomenclature of allergies is the definition of hypersensitivity, which is understood as manifestations and symptoms that develop when exposed to certain stimuli in doses that do not cause these manifestations in normal individuals. This concept unites all types of hypersensitivity, including allergies mediated by immunological mechanisms, in contrast to non-allergic hypersensitivity (pseudoallergy). In most patients, allergic manifestations are associated with IgE-class antibodies, and therefore they are classified as IgE-mediated allergies. However, not all IgE-mediated reactions develop according to atopic mechanisms. The term “atopy” refers only to the genetic predisposition to develop IgE-mediated sensitization to the most common environmental allergens, upon contact with which the majority of the population does not develop sensitization.
It is emphasized that the diagnosis of atopic eczema can only be made in cases of IgE-mediated sensitization, confirmed by skin tests or determination of IgE antibodies to allergens. In all other cases, a diagnosis of non-atopic eczema is made. Differential diagnosis between these two types of eczema also has important prognostic significance: in children with atopic eczema, the possibility of developing bronchial asthma in adolescence is significantly higher than in patients with non-atopic eczema.
The mechanisms of development of immune abnormalities in the body as a whole and directly in the skin of patients have not yet been definitively determined. Differences in the pathogenetic mechanisms leading to the development of IgE-dependent and IgE-independent types of dyshidrotic eczema remain insufficiently studied, which leads to underestimation or overestimation of atopic factors. A new approach to the classification of atopic conditions is needed to improve diagnosis and treatment.
Thus, it can be noted that at present there is no single generally accepted theory of the occurrence of eczema. Despite a large number of studies, the pathogenesis of dyshidrotic eczema and its place in the structure of skin pathology remain incompletely studied.