Eczema is a non-infectious chronic skin disease that affects up to 10% of the world's population in one form or another. Women are more susceptible to pathology than men. Scientists have not established the exact reason for this statistics, but it is possible that the appearance of this disease is influenced by changes in hormonal levels after childbirth and frequent use of aggressive detergents in everyday life. Eczema is not contagious and only causes discomfort to the patient. There are several types of disease. All of them are characterized by severe itching, peeling and redness of the skin.
Causes of eczema
Among the main causes of this disease, doctors call a violation of the barrier function, when the outer layer of the epidermis fails to protect the skin from the aggressive effects of various external factors. On the other hand, through a broken barrier, the body loses a large amount of water, which leads to dehydration and even greater skin vulnerability.
In a large number of cases, the tendency to eczema is hereditary. Depending on the type of eczema, provoking factors may include:
- Aggressive skin care: washing with soap, using harsh cosmetics with sulfates, excessively long water procedures and hot water. All this leads to the washing away of the protective sebaceous film from the surface of the epidermis; accordingly, the surface of the body loses water and protection from external influences.
- Dry air, stay in a hot climate, bath.
- Allergens of various origins: food, pollen, mold, dander and animal hair.
- Contact allergens: nickel, latex,
- Stress.
How to avoid worsening dermatitis in winter
In winter, exacerbation of dermatitis is common. Even healthy skin can have a hard time coping with temperature changes and dry indoor air. The following will help you get rid of the symptoms of the disease even in the frosty months:
- cold compresses,
- warm baths with oatmeal or baking soda,
- creams or ointments for the body with a high concentration of oils in the composition (apply the cream immediately after a bath or shower).
In winter, it is especially important to try not to irritate the skin, do not rub it with a towel, avoid scratches, and do not use cosmetics with fragrances (Fig. 4). When cleaning, be sure to wear gloves and goggles when using aerosol cleaners. In clothing, preference should be given to soft, natural fabrics, such as cotton. Thus, during the cold season, the daily routine should be even more gentle than usual.
Figure 4. How to care for skin with eczema in winter. Illustration: MedPortal
Types of eczema
Eczema is manifested by skin rashes and a number of other general symptoms, but according to the origin and characteristics of the course, several types of this disease can be distinguished:
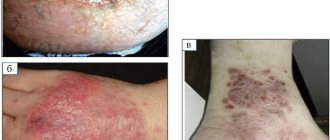
- Atopic dermatitis affects adults and children, and is associated with dehydration of the skin, which cannot withstand the harmful effects of the environment and allergens entering the body. In young children, symptoms occur on the cheeks, in older children - in the bends of the elbows and knees, on the neck, but in general the location can be anywhere.
- Contact dermatitis is a reaction to local exposure to an allergen or irritant. It occurs precisely at the point of contact. Contact allergens include some metals (nickel, cobalt), latex, the juice of certain plants, as well as many components of household chemicals and cosmetics.
- Seborrheic dermatitis is also associated with dysregulation of the sebaceous glands, and affects the scalp, less often the forehead, the area behind the ears, the wings of the nose and the upper back. Appears as fatty, dense crusts or scales, and in infants the condition is known as gneiss.
How to live with dermatitis
Atopic dermatitis in adults can become chronic, and then you will have to fight it all your life. There is no cure for eczema, but the good news is that the disease can be controlled by keeping symptoms to a minimum. To do this you need 18:
- know and exclude contacts with triggers that provoke inflammation,
- take good care of your skin,
- use medications prescribed by a specialist.
It is very important to individually select the type and form of the drug so that the therapy is effective and comfortable for the patient. This also applies to topical steroids. In addition, you need to constantly monitor the development of the disease and be under the supervision of a specialist. Long-term remission may be a reason to gradually discontinue medications or switch to small doses of the drug. If symptoms increase, the specialist will help adjust the treatment plan by selecting a new therapy.
Unfortunately, sometimes eczema is unpredictable. It can flare up suddenly, and sometimes it can be difficult to understand why it has returned. The cause of its manifestation may be stress, anxiety, climate change or the quality of tap water. Living with eczema, you always need to be on guard. But even if the disease makes itself felt at the most inopportune moment, you should not perceive it as a disaster. Since our emotional state is closely related to the manifestations of eczema, we can overcome the disease only by accepting our skin as it is. There is no need to hide dermatitis, it needs to be treated, and then the skin will definitely reciprocate the love shown.
Is eczema contagious?
Eczema has skin symptoms such as rashes and peeling that are noticeable to others, which is why people often wonder if the condition is transferable to others.
This question of whether eczema is contagious is very important, since the appearance of the skin is unpleasant to contemplate and often repels others, which leads to stigmatization, social isolation and various psychological problems, from neurosis to depression. In many countries, the psychological aspects of this disease are studied very deeply because it greatly affects the quality of life. Both the patient himself and loved ones must have a good understanding of the nature of the disease, be confident in their own safety, and that eczema can be cured.
How is coin-shaped eczema diagnosed?
A dermatologist may suspect coin-shaped eczema based on external signs. To confirm, standard tests are prescribed, including a general analysis of urine and blood, and a biochemical blood test. The patient may need to consult a neurologist, gastroenterologist, allergist and endocrinologist.
Coin-shaped eczema must be distinguished from other types of dermatitis, psoriasis, scabies and dermatomycosis. For this purpose, an enzyme immunoassay test of blood for antibodies is performed. To identify an infection, a microbiological examination of a smear from the site of inflammation is carried out. It also helps determine antibiotic sensitivity and prescribe the correct treatment.
Is eczema inherited from person to person?
Research in recent years has shed light on the cause and mechanisms of development of the disease. Thus, its hereditary nature has been deeply studied. Observations of identical twins have shown that if one of them has this problem, there is a greater than 80 percent chance that the other will develop it too. This confirms that eczema is inherited. A number of genes have been discovered that are found in patients, but often various combinations of genes are to blame for the disease, as well as the interaction of genetic predisposition with environmental conditions and other external factors. There is no single mutation that is present in all patients and leads to pathology.
The CARD11 gene encodes a protein that plays a key role in the signal transmission mechanism in the receptors of T-lymphocytes, immune cells, and when mutated, these cells can no longer work correctly. Mutation of this gene occurs in patients with atopic dermatitis. To understand the mechanisms through which changes in the CARD11 protein lead to skin damage, the scientists conducted several experiments on cell cultures and also observed patients with a family history of dermatitis. In each of the four families, mutations were detected in different parts of the CARD11 gene, but the disturbances in the functioning of the receptors were very similar to each other. The number of T-lymphocytes remains the same, but these cells function incorrectly and react incorrectly when foreign bacteria and fungi enter the body. This leads to decreased immunity and frequent infections. This probably reduces the barrier function of the skin, which is why it is damaged. In this separate, hereditary form of atopic dermatitis, a tendency to bacterial and fungal diseases is combined with a rash and dryness of the body. The autosomal dominant pattern of inheritance characteristic of this gene means that the disease appears in every generation, regardless of gender, and one copy of the mutant DNA is enough to cause symptoms of eczema.
A mutation in the FLG gene occurs in 30% of patients with atopy. This gene contains the profilaggrin protein, which is necessary for the formation of the correct structure of the outermost layer of the epithelium. Proteins formed from profilaggrin help create a strong barrier that keeps water inside and prevents foreign substances such as toxins, bacteria and allergens from penetrating the skin. These proteins are also natural moisturizing factors that help maintain the elasticity of the outer layer of the skin. Changes in the FLG gene can cause damage and rashes. Not all carriers of this mutation develop atopic dermatitis, however, when exposed to any external triggering factors, the risk increases significantly. Research shows that this exposure triggers epigenetic changes in DNA. In this case, the DNA sequence itself remains the same, but the regulatory mechanisms associated with this gene change. The activity of the gene changes, this affects the synthesis of the proteins encoded in it. In predisposed people, this provokes allergic reactions. The FLG mutation is also inherited in an autosomal dominant manner, but due to epigenetic influences, not all carriers become affected.
Sources
- National Center for Health Statistics, National Health Interview Survey, 2014.
- National Eczema Association website. Eczema causes and triggers.
- Thomas N. Helm and all. What is the role of neomycin in the etiology of allergic contact dermatitis? Medscape. -2020
- Susana Vilaça and all. Simultaneous contact allergy to neomycin, bacitracin, polymyxin, and dexamethasone: An often unrecognized cause of allergic contact dermatitis in patients using topical antibiotics. Journal of the American Academy of Dermatology. -2012, -V. 6, -I. 4, -S. 1, -P. AB74. https://doi.org/10.1016/j.jaad.2011.11.316
- A. C. de Groot, A. Herxheimer. Isothiazolinone preservative: cause of a continuing epidemic of cosmetic dermatitis. Lancet. -1989. DOI: 10.1016/s0140-6736(89)91318-4
- Atopic Dermatitis 101 for Adults. National eczema association. -2017
- JI Silverberg and all. Symptoms and diagnosis of anxiety and depression in atopic dermatitis in US adults. British Journal of Dermatology. -2019. https://doi.org/10.1111/bjd.17683
- A. Wollenberg and all. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part IJ Eur. Acad. Dermatol. Venereol. -2018. DOI: 10.1111/jdv.14891
- John Elflein. Global use of prescription topical treatments and phototherapy for eczema 2022. -2020
- C. Fookes. Topical Steroids. Drugs.com. -2018
- A. Roeder and all. Safety and efficacy of fluticasone propionate in the topical treatment of skin diseases. Skin Pharmacol. Physiol. -2005. DOI: 10.1159/000081680
- NHS. Topical corticosteroids
- Give Topical Steroids the Fingertip. National eczema association
- Instructions for the medical use of the drugs FeniVate cream RU P N012556/01 dated 07/15/2009 and FeniVate ointment RU P N012556/02 dated 07/16/2009.
- New, sales start in June 2022.
- Katsambas A.D., Lotti T.M. European treatment guidelines in dermatology. 2014, MEDpress-inform LLC, 3rd ed., trans. from English, 736 p.
- Ellie Choi and all. Efficacy of targeted education in reducing topical steroid phobia: A randomized clinical trial. Journal of the American Academy of Dermatology. -2020. -V. 83, -I. 6. -P. 1681-1687. https://doi.org/10.1016/j.jaad.2020.02.079
- NIAID. Eczema (Atopic Dermatitis) Treatment
Does eczema spread through contact with a sick person?
Through direct contact, diseases that belong to the group of infectious diseases are transmitted. These diseases are caused by bacteria, viruses or fungi. The transfer of these microorganisms to another person upon contact, through household objects, with drops of saliva during coughing, leads to the spread of pathology. This property is called contagiousness. The vast majority of types of eczema are not infectious, which means they are not contagious. Pathology cannot pass from sick to healthy, so it doesn’t matter whether you touch the affected skin or use a shared towel, eczema cannot appear from this.
In rare cases, when the affected skin becomes infected with bacteria, it can spread through contact with another person, and if they also have eczema, there is a possibility of infection. So, if you already have this skin condition, you may get the organism from someone else and your eczema will become more complicated by infection. However, this is a very unlikely scenario, and bacterial inflammation is more likely to occur if personal hygiene is not followed.
Eczema and sex
Infections caused by viruses, bacteria or protozoa are transmitted sexually. Eczema is not an infection; this skin disease does not belong to the group of sexually transmitted diseases. Therefore, it is impossible to catch this condition from your partner during sex.
If you have symptoms similar to eczema after sexual intercourse, and your partner has the same symptoms, you should immediately consult a doctor. This means that the rash is not caused by eczema, but by an infection, and if you do not get a diagnosis and treatment in time, there is a high risk of complications associated with both sexual function and infertility, and with the general well-being of the body. Thus, the herpes simplex virus causes a rash that can be confused with eczema. However, this disease must be treated with antiviral drugs. Without treatment, it brings a lot of unpleasant sensations, and if the body weakens, it can lead to a severe form of encephalitis. Herpes is also dangerous during pregnancy, for the fetus (unlike eczema).
Eczema and blood transfusion
When asked whether eczema can be contracted through a blood transfusion, doctors have a clear answer. No, this disease is not transmitted from person to person through blood. It is known that a number of genes may be responsible for the symptoms of eczema. When a blood transfusion occurs, blood cells that carry the genetic material of another person enter the body. Therefore, doubts may arise: whether the eczema gene will be passed on in this way. The fact is that blood cells are mature and formed. They do not participate in further division and are not sources for subsequent generations of red and white blood cells. They serve for a certain time, performing their functions, and then are disposed of in the spleen. New cells are supplied by the bone marrow. When a person requires a transfusion, his own bone marrow does not have time to grow the required number of cells (for example, during bleeding). Then he is helped by injecting the blood of another person. Even if these new cells have a hereditary defect, they will work out before causing symptoms of atopic dermatitis, and they will be replaced by healthy own cells that the bone marrow has grown in a calm environment.
Signs of the disease
Manifestations of the disease depend on its form.
True eczema
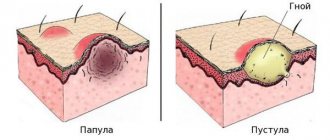
An area of redness appears on the skin, in the area of which there is itching. Then a large number of small bubbles form on it. They open very quickly, leaving shallow skin defects (erosions) in their place, and weeping occurs. When erosions and weeping dry out, crusts form in their place and peeling is noted. Typically, skin lesions occur symmetrically, on the right and left.
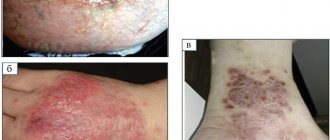
Microbial eczema
Skin lesions occur around chronic foci of infection. The picture is similar to that of true eczema, but the crusts may be purulent in nature. A type of disease is nummular eczema, in which the lesions are small, round, and have the shape of coins.
Varicose eczema
Lesions form in the area of varicose veins as a result of impaired blood supply to the skin, trauma, or increased sensitivity to drugs used to treat varicose veins.
Varicose eczema
Seborrheic eczema
Lesions appear on the scalp, face, chest, and ear area. Red plaques form, on the surface of which there is peeling and small yellowish-brown pimples. Nearby lesions can merge with each other, forming larger ones.
Dyshidrotic eczema
It is believed that the main reasons for the development of this form of the disease are dysfunction of the endocrine and nervous systems, autonomic dysfunction, and genetic predisposition. Lesions form on the palms and soles. There is almost no redness or swelling; small blisters predominate. Over time, they can open up to form erosions and crusts, or merge into larger ones. With a long course, the lesion spreads to the back of the hands and feet, where in appearance it more closely resembles true eczema. In some cases, changes in the nail plates are observed.
Callous (tilotic, horny) eczema
With prolonged eczema, calloused thickenings form on the palms and soles.
Childhood eczema
In children, eczema is often accompanied by severe swelling. Often an infection occurs, which significantly aggravates the course of the disease.
Treatment of eczema
In treatment, a number of drugs are used that affect the mechanism of the disease and eliminate symptoms.
- Glucocorticoids. These hormonal drugs are prescribed locally in the form of ointments or creams. They regulate the functioning of immune cells, thus eliminating all symptoms of inflammation. They are effective against rashes, itching, and redness. Depending on the severity of the process, prevalence and localization, hormones of varying strengths are prescribed.
- Calcineurin inhibitors act similarly to hormonal agents, blocking the process of inflammation, but are free from the side effects of glucocorticoids and are better tolerated.
- Antihistamine tablets are effective against itching.
- Combined nonspecific drugs are good for treating mild forms or in combination with specific therapy. This is a wide range of products that contain emollients, oils, antiseptics, substances that affect inflammation and regeneration.
Gene therapy is not used in the treatment of eczema, since there is no one specific gene that needs to be changed to get rid of this disease. At this stage of medical development, it is impossible to come up with a genetic technology that would help in the fight against dermatitis.
How to escape from dermatitis?
Atopic dermatitis cannot be completely cured, but it is possible to reduce the severity of its symptoms or even achieve stable remission. The three steps to healthy skin are cleansing, moisturizing and drug therapy. Patients with eczema may be prescribed:
- local steroid drugs,
- steroid injections,
- immunosuppressants, which suppress the body's immune response,
- antihistamines,
- antibiotics in case of infections,
- phototherapy - treatment with ultraviolet light.
At the same time, topical steroids - ointments, creams and gels - remain the most widely used remedy against eczema and the “gold standard” of treatment.8
In 2022, 55% of eczema patients were actively using topical corticosteroids.9
What is the secret of their popularity? The thing is that glucocorticosteroids in such creams act directly on the cells of the epidermis, providing an anti-inflammatory effect on damaged areas of the skin. Being synthetic analogues of human steroid hormones, they attach to cellular receptors and trigger a cascade of chemical transformations in cells. Thanks to corticosteroids, the production of inflammatory mediators responsible for pain and swelling in the tissue is reduced. In addition, corticosteroids (fluticasone propionate, betamethasone dipropionate, clobetasol propionate, etc.) help to narrow capillaries and reduce allergic and immune reactions, which make atopic skin so sensitive.10
The great advantage of the latest generation of topical steroids, such as fluticasone propionate11, is their safety profile. They tend to clear faster and have less impact on the body's immune and hormonal systems compared to first-generation corticosteroids.
Important! Many topical steroids are available without a prescription, but consultation with a specialist is required before using them. Drugs in this group have contraindications, and their long-term, uncontrolled use can lead to thinning of the skin, the appearance of acne, addiction and other side effects.12
Who needs topical corticosteroids
Topical corticosteroids are the second step in the treatment of eczema, which is resorted to if the disease worsens even after following all the usual recommendations of specialists. Sometimes patients regularly moisturize their skin, take warm baths and avoid any contact with irritants, but still suffer from itching, redness and pain.
In this case, topical steroids are an excellent way to relieve inflammation and overcome symptoms where other means are powerless. A properly selected cream can quickly alleviate the condition, playing the role of an “ambulance”, allowing the skin to recover and speed up healing.
Important! Before using a cream containing glucocorticosteroids, be sure to read the instructions. Schemes for using different creams may differ. As a rule, the cream is recommended to be used after taking a bath, applied to the affected areas in the direction of hair growth. The thighs and crease areas may need a little more cream than other areas.13 You can apply a moisturizer on top of the steroid cream.
What should a new generation cream be like?
When choosing a cream based on corticosteroids, you should pay attention to its composition. The latest generation of corticosteroids, such as fluticasone propionate,11 are potent and have a low risk of cutaneous and systemic side effects. In addition, the cream should have caring properties (Fig. 3) and be comfortable: absorb quickly, not leave a film, and not have a strong odor. If the disease causes severe dry skin, it is better to choose an ointment, and in case of weeping rashes, light cream-like textures are suitable.
Figure 3. What qualities should a cream based on glucocorticosteroids have? Illustration: MedPortal
One example of a modern remedy against dermatitis is the new product FeniVate - a drug of the latest generation with a pronounced anti-inflammatory effect in the form of ointment and cream.14-16
FeniVate is created using a special micronization technology, which promotes better penetration of the active substance into the epidermis. The drug works at the cellular level, has a targeted effect on the source of inflammation and helps not only to cope with the symptoms of allergic dermatitis, but also to suppress the inflammatory reaction on the skin.14
Why is it so important to overcome steroid phobia?
Topical steroids help quickly relieve eczema symptoms and control the progression of the disease. However, many patients refuse to resort to them for fear of encountering side effects from taking hormonal drugs. Today, experts call steroid phobia one of the main reasons for the development of complications of atopic dermatitis: pustular skin lesions, inflammation of the eyelids and conjunctivitis.17
Don't let fear affect your quality of life. Local steroids have a moderate effect on systemic processes in the body.12 And to reduce the risk of unwanted side effects to a minimum, you should regularly visit a specialist and adjust therapy in a timely manner if it becomes ineffective or causes discomfort.