Rubella disease in adults
Rubella belongs to the Togavirus family. Transmission occurs through airborne droplets exclusively from an infected person. Transplacental transmission during pregnancy is also possible. The virus is unstable in the environment and quickly dies when exposed to ultraviolet radiation.
Despite the fact that the pathology belongs to the category of children, adults can still become infected. Moreover, in this case, the disease passes with complications, causing intense signs of manifestation and a significant deterioration in the patient’s well-being. The disease poses a particular danger to women during pregnancy.
After contact with an infected person, the disease makes itself felt after 2–3 weeks, and the first symptoms resemble a common acute respiratory infection.
An infected person begins to spread pathological microorganisms already from the 5th day of the incubation period.
During the autumn-winter period, the body's protective functions are most susceptible to various pathologies. Therefore, this is the time when the greatest number of requests for medical help from patients with rubella symptoms occurs.
Adults encounter the rubella virus much less often than children, but the disease is severe and has complications.
Symptoms of rubella in adults
The rubella virus can appear in an atypical (erased) or manifest form. The first is characterized by a mild course of the disease, without severe symptoms. With a typical infection, signs of the virus of varying severity are observed.
In adults, the following symptoms of rubella infection appear:
- Temperature increase. Fever appears in the first days of the disease. The patient's health deteriorates as if he were suffering from an acute respiratory disease. In some cases, the temperature reaches 40°, and it is quite difficult to bring it down in adults.
- Enlarged lymph nodes. The symptom is typical for the first day of the pathology. The process of inflammation can affect any group of lymph nodes (axillary, inguinal), doctors have not established a clear sequence.
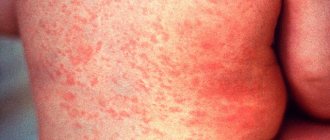
- Rash on the skin. This is the main sign of rubella, by which an experienced specialist can distinguish it from ailments with similar clinical manifestations. If in children the rashes appear in the form of red dots, then adults suffer from whole spots that merge to form erythema. The lesion begins from the behind-the-ear region, gradually covering the lower and upper limbs, back, and buttocks. In almost every case it occurs on the inner surface of the cheeks, the mucous membrane of the palate. In adults, the rash lasts longer than in children and begins to go away only after 5–7 days.
- Headache. With rubella, migraine cannot be eliminated with the help of medications and annoys the patient during the first days of the disease. The symptom significantly worsens your health.
- Painful sensations in muscles and joints. The symptom occurs at the beginning of the disease and resembles the condition of the flu. Therefore, it is difficult to diagnose rubella in the first days without consulting a doctor.
- Tearing. Another special symptom of rubella in adults. Discomfort occurs in daylight and artificial lighting. The patient feels better in a room with dim light.
- Conjunctivitis. Discharge of pus begins 3-4 days after the onset of the disease, usually at night. In the morning the patient can hardly open his eyes.
- Sore throat, runny nose, cough. This “bouquet” is typical for ARVI, but with rubella in an adult it manifests itself to the fullest.
Rubella in adults is characterized by a clear manifestation of symptoms, in contrast to the clinical picture of the disease in childhood.
Why is rubella dangerous during pregnancy?
- The developing fetus during the first trimester of pregnancy is most vulnerable to rubella viruses if the pregnant woman does not have immunity to the disease. Viruses can enter the fetal blood through the placenta and cause many serious developmental defects.
- Rubella in pregnant women causes miscarriages and stillbirths in 15% of cases.
- With congenital rubella, the viruses in the child’s body persist for 1 to 2 years, and therefore the newborn poses an epidemic danger to others even if there are protective antibodies in the blood.
How dangerous is the rubella virus during pregnancy?
The rubella virus is transmitted to pregnant women in two ways: from a sick person and from a sick pregnant woman to the fetus.
- Viruses are transmitted by airborne droplets, which contributes to the rapid spread of infection in organized groups. The disease occurs only with close and prolonged contact, unlike chickenpox and measles.
- Rubella viruses during pregnancy are able to penetrate through the placenta into the blood of the fetus, damaging its genetic apparatus and destroying cells. In women who suffered from rubella while in the 3rd to 4th week of pregnancy, from 50 to 85% of cases of birth of children with congenital deformities are registered.
- Rubella viruses in newborns who have had the disease in utero are released into the external environment through nasopharyngeal mucus, feces and urine for many months. The child poses a great epidemiological danger to others.
- Rubella viruses during pregnancy begin to be released into the external environment from the patient several days before the appearance of the rash and continue to be released for a week after its appearance.
Rice. 2. Rubella during pregnancy in the first trimester poses a great danger to the fetus.
Be careful - rubella is dangerous during pregnancy!
Rubella is considered to be a mild disease.
However, this definition is valid for the course of this infection only in children, since rubella in pregnant women is fraught with serious consequences for the unborn child.
The danger of the rubella virus is that it is almost always transmitted from the mother to the fetus, freely passes through the placental barrier - since it is a virus - (a particle smaller than a blood cell) and damages it. Depending on the stage of pregnancy at which infection occurs, the fetus has a different probability of developing malformations.
Yes, the disease in children is very mild, the body itself copes with the pathogen (rubella virus), most often you can get by with a limited regimen, plenty of fluids and vitamins. This is true. But! During pregnancy, the fetus develops congenital rubella syndrome (cataracts, damage to the inner ear, heart defects, microcephaly).
In many countries, acute rubella is a medical indication for termination of pregnancy because the syndrome occurs in the fetus in almost all cases when the mother becomes ill with rubella in the first months of pregnancy. If a girl was not vaccinated in childhood, if she did not have rubella, there remains a danger of contracting rubella as an adult. 15-30% of women of childbearing age do not have such protection.
So, what is rubella?
- Why is it dangerous?
- Who needs to be examined and when?
- How to determine whether there is a danger to the baby and what to do?
Rubella is an infectious disease of a viral nature, which is highly contagious, manifested by a rash on the skin that tends to spread quickly, enlarged lymph nodes (occipital group) and a slight increase in temperature. There are periodic increases in incidence with an interval of 5-7 years, in addition, there is an autumn-spring seasonality. The rubella virus is transmitted by airborne droplets. In addition, there is transmission of the virus from mother to fetus through the placenta during pregnancy (transplacental transmission).
- The source of the virus is often children, especially those who attend kindergarten, sports section or school. Therefore, a woman who does not have immunity to rubella and is pregnant with her second child has a greater chance of becoming infected with the rubella virus. The insidiousness of rubella is that the incubation period, that is, the period between infection and the appearance of the first symptoms of the disease, lasts approximately 2-3 weeks.
- Moreover, during the last week of the incubation period, the patient already releases the virus and poses a danger of infection to others, despite the fact that he himself feels great and may not know about his disease.
- Rubella is considered contagious 7 days before the rash appears and another 7-10 days after it disappears.
- In addition, very often (50-90% of cases) rubella is asymptomatic, but the person also releases the virus and can infect others. In general, the disease is mild and complications are rare.
- The most serious complication is rubella encephalitis, which, fortunately, is quite rare (1:5000-1:6000).
In adolescents and adults, rubella is much more severe than in children. However, most patients do not require special treatment. Medicines are used to treat symptoms and complications that alleviate the general condition. After an illness, lifelong immunity develops, but its intensity may decrease with age and under the influence of various circumstances. Thus, a history of rubella in childhood cannot serve as a 100% guarantee against recurrent disease.
What is the danger to the fetus?
Rubella is considered to be a mild disease. However, this definition is valid for the course of this infection only in children, since rubella in pregnant women is fraught with serious consequences for the unborn child.
The danger of the rubella virus is that it is almost always transmitted from the mother to the fetus and damages it.
Depending on the stage of pregnancy at which infection occurs, the fetus has a varying probability (in the first trimester the probability reaches 90%, in the second - up to 75%, in the third - 50%) multiple malformations are formed. The most typical are damage to the organ of vision (cataracts, glaucoma, corneal opacities), the organ of hearing (deafness), and the heart (congenital defects).
Congenital rubella syndrome also includes defects in the formation of the bones of the skull, brain (small brain size, mental retardation), internal organs (jaundice, enlarged liver, myocarditis, etc.) and bones (areas of rarefied bone tissue of long tubular bones). In 15% of cases, rubella in pregnant women leads to miscarriage or stillbirth.
If rubella is detected, an artificial termination of pregnancy is always carried out.
What methods are used to diagnose rubella?
The most widely used methods in diagnosing rubella are serological methods, in particular the enzyme-linked immunosorbent assay (ELISA) .
- The immunological marker of primary infection is IgM to the rubella virus. IgM begins to be produced in the first days of the disease, reaches its maximum level at 2-3 weeks and disappears after 1-2 months. But the period of circulation of IgM antibodies can vary significantly depending on the infectious pathogen and the individual characteristics of the body’s immune response.
- When infected with rubella, trace amounts of IgM antibodies to the rubella virus are detected in some cases for 1-2 years or more. Thus, their presence in the blood of a pregnant woman does not always confirm primary infection during pregnancy. In addition, the specificity of even the best commercial test systems for detecting IgM antibodies is not absolute. In some situations, as a consequence of the very high sensitivity of the tests, nonspecific false-positive results are possible. IgG is detected 2-3 days later than IgM, increases to a maximum by a month from the onset of the disease and persists throughout life. In an infected fetus, anti-rubella IgM begins to be produced from 16-24 weeks and can persist for a long time (up to a year or longer). Until 6 months of age, maternal IgG circulates in the newborn, and then specific IgG begins to be produced in a child with congenital rubella during the first year of life.
- Since the risk of pathology of fetal development during acute primary infection with the rubella virus during pregnancy is significant, in order to confirm or exclude the fact of recent infection with the rubella virus in a pregnant woman, PCR testing of biological fluids for the presence of rubella virus RNA and a blood test using ELISA for the avidity of IgG to the rubella virus are used.
For the purpose of early diagnosis of rubella in a pregnant woman or intrauterine infection, the following can be used to detect rubella virus RNA by PCR:
- blood from the mother's vein,
- umbilical cord blood obtained by cordocentesis,
- amniotic fluid,
- chorionic villi obtained from infected pregnant women by transabdominal amniocentesis.
- Detection of high-avidity IgG antibodies in the blood (IgG avidity ≥70%) allows one to exclude recent primary infection.
Low-avidity IgG antibodies (IgG avidity ≤ 50%), on average, are detected within 3-5 months from the onset of infection (this may depend to some extent on the method of determination), but are sometimes developed over a longer period. In itself, the detection of low-avidity IgG antibodies is not an unconditional confirmation of the fact of fresh infection, but serves as additional confirmatory evidence among other serological tests.
Who needs to be examined?
Laboratory diagnosis of rubella is especially important in the following categories of subjects:
- Women who are planning a pregnancy or pregnant women in order to identify risk groups. If a woman has not previously had rubella, is not sure that she has had it, or does not know for sure about it, it is necessary to study the level of specific IgG using the ELISA method. If the result is positive, there is no risk of fetal infection. In case of a negative result, vaccination is recommended. In this case, the planned pregnancy must be postponed for three months!!!
- Pregnant women with suspected rubella virus infection and adults with severe cases or complications of rubella. It is necessary to determine specific IgM and IgG and interpret test results from an infectious disease specialist to select further tactics.
In general, the diagnostic algorithm looks like this:
- IgM - not detected, IgG - not detected, or their concentration is not sufficient to protect against infection. It is recommended: exclude contact with patients with rubella, repeat the examination after 2 weeks, during which medical observation of the pregnant woman is carried out. If the result is negative again, conduct a third serological examination, continuing medical observation. If the test is negative in the third study, stop observation and warn the pregnant woman that she is susceptible to rubella infection.
- IgM – not detected, IgG – detected, their concentration corresponds to the protective level. During the initial examination of a pregnant woman in the early stages of pregnancy, further observation for rubella infection is not indicated.
- Specific IgM antibodies to the rubella pathogen were detected. In this case, IgG antibodies are either detected or not detected. There is a risk of congenital pathology of the fetus.
A repeat serological test is indicated after 2 weeks, with further consultation with an infectious disease specialist. To exclude cross-reaction and the influence of rheumatoid factor, confirm/exclude the diagnosis, it is recommended to do an IgG avidity test, conduct a quantitative analysis for IgM and PCR testing of the mother's blood for the presence of rubella virus RNA.
Newborns with signs of congenital rubella.
If intrauterine infection with the rubella virus is suspected in a newborn, it is necessary to examine the level of IgM in the newborn's blood serum. A positive test result indicates an acute infection. The diagnosis can be confirmed if a positive IgM titer is also detected in the mother's blood. In cases where infection occurred in the first or second trimester of pregnancy, IgM may not be detected. Then the presence of infection can be judged by the dynamics of IgG. In the presence of infection, the level of IgG increases in the first months of a newborn's life.
In the absence of infection, IgG in the blood of the newborn is either not detected (the mother is seronegative) or decreases (elimination of maternal antibodies).
The presence of specific IgG in a child older than 6 months indicates intrauterine infection.
What should a pregnant woman do if she finds herself in a rubella outbreak?
If a pregnant woman who has not had rubella, has not been vaccinated and has not had immunity to the rubella virus determined, finds herself in a focus of rubella infection (contact with a person who has rubella), she must immediately contact an infectious disease specialist!
As mentioned above, the danger of infection of pregnant women through contact with a person with rubella exists only for those women who are susceptible to the rubella virus due to the lack of protective immunity. The presence of specific antibodies (IgG to the rubella virus) indicates the patient's immunity.
It is very important to begin testing as early as possible after exposure. If antibodies to the rubella virus are found in protective concentrations in a woman in the first 6 days after contact, then these antibodies are a consequence of long-term rubella. In this case, the woman is not susceptible to the rubella virus, and contact does not pose a danger to her. The absence of antibodies or a weakly positive result in the early stages of the examination indicates that the woman is not protected against rubella, and there is a risk of infection.
But you shouldn’t despair in advance, since it is known that susceptible women who have been in contact with people with rubella may not get sick.
To exclude infection, it is necessary to conduct a repeated serological examination over time 2-4 weeks after contact.
Serological monitoring of contacted women must be carried out until the end of the 2nd trimester of pregnancy.
If a woman comes late after contact (a week or more after contact with a sick person), it is necessary to detect IgG, IgM and IgG avidity to the rubella virus using ELISA, and examine the blood for rubella virus RNA using PCR.
In addition to a visit to an infectious disease specialist, a woman must contact a gynecologist, who will prescribe the necessary tests to determine the condition of the fetus (detailed ultrasound, screening studies of the 2nd and 3rd trimesters). If these tests indicate any problems in the child’s development, an amniocentesis procedure may be prescribed.
Further, based on the results of all examinations and tests, the issue of the presence of congenital defects and termination of pregnancy is decided. In many countries, rubella detected in the first trimester of pregnancy is an indication for termination of pregnancy. If pregnancy is complicated by rubella at 14-16 weeks, the issue of recommendations for maintaining pregnancy is decided at a consultation of doctors. If it is impossible to abort a pregnant woman, immunoglobulin is administered intramuscularly in a dose of 20–30 ml intramuscularly. In the future, preventive measures are taken to protect the fetus, treatment of placental insufficiency, prevention and treatment of miscarriage.
Prevention of rubella in pregnant women.
To prevent congenital rubella syndrome, WHO (World Health Organization) recommends combining three principle approaches to the elimination of rubella and congenital rubella syndrome:
- vaccination of children,
- vaccination of teenage girls
- vaccination of women of childbearing age planning to have children.
According to statistics, 11-30% of women of childbearing age are not protected from rubella .
If a girl or young woman has not had rubella and is not vaccinated, then before planning a pregnancy, she herself needs to think about the appropriate vaccination.
- You need to donate blood for rubella antibodies.
- If there are no antibodies, it is necessary to get vaccinated against rubella 3 months before the expected pregnancy. Vaccination protects almost 100%; immunity after a single vaccination lasts for an average of 15-20 years, then immunization can be repeated.
It must be remembered that after the administration of the rubella vaccine, it is not recommended to become pregnant for 3 months.
But !!! If pregnancy occurred earlier than this period or a woman already expecting a child was vaccinated, this is not an indication for termination of pregnancy.
In conclusion, I would like to remind you that there are no hopeless situations! They appear only if you allow them to enter your life. Having a healthy baby is not only necessary, but also possible!
If you are planning a pregnancy, diagnose your immunity to the rubella virus, and then get pregnant,
wear it calmly, give birth easily and raise a healthy baby! Good luck to you!
Articles on the topic 10 reasons why you shouldn’t be nervous... What you need to know about intrauterine... Treatment with the Andro-Gyn device... Pregnancy calendar Preparing for pregnancy or... Step-by-step instructions for happy... Cervical erosion during pregnancy
Rubella in pregnant women: symptoms of the disease
Rubella during pregnancy occurs in typical, atypical (without rash) and inapparent (asymptomatic) forms. Asymptomatic forms account for up to 90% of all cases of the disease. The only way to detect it is to carry out serological tests, when an increase in antibody levels can be detected.
Currently, there is an increase in the number of cases of the disease in adults, in whom rubella in its typical course has a number of features.
Symptoms of rubella in pregnant women:
- The incubation period for the disease lasts 11 - 24 days. During this period, viruses that have entered the body multiply intensively in the cells of the mucous membranes of the upper respiratory tract and lymph nodes, which enlarge towards the end of the prodromal period (usually occipital). With rubella, the groups of occipital and posterior cervical lymph nodes most often enlarge. Their size reaches a large pea or more, they are of medium density, painful on palpation. As the rash disappears, the lymph nodes decrease in size.
- Rubella in pregnant women is often severe, with high (up to 39°C) body temperature, severe headache, severe muscle and joint pain, and lack of appetite.
- Catarrhal phenomena of the upper respiratory tract and inflammation of the conjunctiva of the eyes are significantly expressed.
- Rash in pregnant women tends to merge. When merging, extensive spots are formed.
- The most common complication in pregnant women is polyarthritis.
Rice. 3. The photo shows rubella during pregnancy. A rash and enlarged lymph nodes are the main symptoms of rubella in pregnant women.
Rubella symptoms
The incubation period for rubella lasts from 10 days to three weeks. The disease can be asymptomatic, manifesting itself on the fifth day - only after the appearance of rashes. After two days, fever may occur with a rise in temperature to subfebrile levels. In some cases, deterioration in health, headache, runny nose, and loss of appetite may occur two days before the onset of the rash.
It is not difficult for a doctor to make the correct diagnosis. It is enough for him to see the rash on the body to understand what kind of infection caused it. If doubts remain, the doctor will refer the patient for testing. This will confirm the diagnosis. The patient will need to donate blood, which will be sent for ELISA.
The most characteristic symptom of rubella in adults - a rash - is usually more pronounced than in children; individual elements of the rash can merge with each other, forming larger erythematous spots.
Small pink spots first appear behind the ears and on the nose, after which they spread to the arms and torso, eventually moving to the lower extremities. When merging, the color of the spots becomes darker, which lasts 1.5 weeks. At the same time, adults experience general malaise, body temperature rises, and patients are bothered by headaches, pain in joints and muscles. In most cases, the disease is accompanied by a profuse runny nose and sore throat.
In addition to the appearance of a rash, a person’s lymph nodes increase in size. This is due to the accumulation of a large number of viruses in them. The nodes located on the back of the head swell especially intensively. This symptom helps confirm the diagnosis.
From the moment of infection until the first symptoms appear, about 10-25 days pass. A person will begin to spread the infection 1 day before the first elements of the rash appear. It remains contagious for 7 days after its onset.
Rubella during pregnancy: consequences
- In women who suffered from rubella while in the 3rd to 4th week of pregnancy, from 50 to 85% of cases of birth of children with congenital deformities are registered.
- Long-term suppression of the immune system during illness leads to the development of sore throats, otitis media, bronchitis and pneumonia.
- Sometimes arthritis or arthralgia are recorded. The joints of the fingers and wrist become inflamed more often. Sometimes the knee joints become inflamed. Arthritis and arthralgia last no more than a month after the rash appears.
- Encephalitis and meningitis develop very rarely.
Of particular danger is the development of rubella in the fetus in the case of an involuntary (asymptomatic) form of the disease in a pregnant woman.
Rice. 4. The photo shows congenital rubella. Deafness is one of the common manifestations of SLE.
Treatment of rubella
Treatment of rubella in adults must be carried out under the supervision of a specialist: therapy should not be delayed or delayed visiting a doctor. Serious consequences threaten patients in the absence of timely medical care.
The most effective preventive measure for people who did not have rubella in childhood is vaccination.
Author of the article:
Mochalov Pavel Alexandrovich |
Doctor of Medical Sciences therapist Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”. Our authors
How does intrauterine infection of the fetus develop?
The rubella virus during pregnancy affects embryonic tissue in the early stages of pregnancy, when the active formation of organs and systems of the fetus occurs. Fetal growth slows down and normal organ formation is disrupted.
In 10 - 40% of cases, pregnancy ends in spontaneous abortion, in 20% - in stillbirth, in 10 - 25% - in the death of the newborn.
Viruses penetrate from mother to fetus during the period of viremia (release of viruses into the blood). This period begins a week before the rash appears and continues for some time after the rash appears. There is an assumption that rubella viruses first infect the epithelium covering the chorionic villi and capillaries of the placenta. They then enter the fetal circulatory system. The resulting chronic infection causes the development of congenital deformities.
- Viruses inhibit the miotic activity of cells. Organ cell populations slow down in growth. They become incapable of differentiation, which interferes with the proper development of organs.
- The ability of rubella viruses to destroy cells manifests itself only in the cochlea of the inner ear and the lens of the eye, causing congenital deafness and cataracts.
Rice. 5. The outer part of the fetal membrane of the embryo is called the chorion (6th week of pregnancy in the photo).
Viruses cause maximum harm to the fetus when infected in the first trimester of pregnancy (first 12 weeks). At the 13th week and later, fetal development defects develop less frequently. The danger persists until the 3rd trimester.
Rice. 6. The photo shows the fetus (6th and 10th weeks of pregnancy).
Rubella (rubeola). Clinical picture. Treatment. Prevention.
Rubella (“German measles”) is an anthroponotic viral infection with generalized lymphadenopathy and small-spotted exanthema.
Brief historical information
The clinical differences between rubella and scarlet fever and measles were first described by I. Wagner (1829); Since 1881, rubella has been considered an independent nosology. The viral nature of the infection was proven by Hiro and Tasaka (1938). The pathogen was isolated by P.D. Parkman, E.H. Weller and F.A. Neva (1961). The teratogenic effect was established by N.M. Gregg (1941), R.A. Kantorowicz et al. (1973), O.G. Andzhaparidze and T.I. Chervonsky (1975).
Etiology
The causative agent is an RNA genomic virus of the genus Rubivirus
family
Togaviridae.
All known strains belong to the same serotype. In the external environment, the virus is quickly inactivated under the influence of ultraviolet rays, disinfectants and heat. At room temperature, the virus persists for several hours and tolerates freezing well. It exhibits teratogenic activity.
Epidemiology
Reservoir and source of infection -
a person with a clinically pronounced or erased form of rubella. The patient releases the virus into the external environment 1 week before the rash appears and for 5-7 days after the rash appears. Children with congenital rubella are of great epidemiological importance. With the latter, the pathogen is detected in the mucus of the nasopharynx and urine (less often in feces) for several weeks, sometimes up to 12-20 months.
Transmission mechanism
- aerosol,
transmission route -
airborne droplets. For infection, longer and closer contact with the patient is necessary than with measles and chickenpox. There is a vertical route of transmission (transplacental transmission of the virus), especially in the first 3 months of pregnancy. Hands and care items are not of epidemiological significance. The exception is toys, which can be used to transmit the virus from mouth to mouth among young children.
Natural susceptibility to infection
high. Serological surveys indicate a large percentage (30% or more in some regions of the country) of seronegative women of childbearing age, especially at the age of 20-29 years. The results of a serological examination of pregnant women indicate a high susceptibility of women of childbearing age to the rubella virus, especially in the age group of 20-29 years (from 8 to 30% seronegative were identified in different years).
Basic epidemiological signs.
Rubella is one of the infections that can be eliminated in the near future, according to the WHO program. In a number of countries (USA, Sweden, etc.) it is detected at an extremely low level. Given the health significance of congenital rubella syndrome, the 48th session of the WHO Regional Committee for Europe (1998) included rubella among the infections that will determine the goals of the Health for All in the 21st Century program. By 2010, the incidence of congenital rubella syndrome should be reduced to less than 0.01 per 1000 births.
In the pre-vaccination period, rubella with a high incidence was recorded everywhere. Due to the absence to date of a widespread immunization program for the population in Ukraine, a tendency towards an increase in morbidity is noted. According to WHO, of all rubella cases registered in Europe, 83% occur in the CIS countries. Rubella is characterized by periodic increases in incidence: moderate (every 3-5 years) and more intense (every 10-12 years). In recent years, there has been a shift in incidence to older ages: mainly schoolchildren and women of childbearing age are affected. They note a high incidence in organized preschool and school groups, among students of secondary and higher educational institutions. The incidence increases significantly in spring and summer.
Rubella is considered to be a mild disease. However, this definition is valid for the course of this infection in children. The disease in adults is characterized by a more severe course (often accompanied by prolonged fever, articular syndrome, and the development of organ pathology). Congenital rubella poses a particular problem. When pregnant women are infected, it can cause serious complications and the birth of a child with various severe developmental defects. According to various authors, the risk of developing congenital defects (vision, hearing, cardiovascular system, etc.) ranges from 12 to 70%, or 10% of the total number of congenital anomalies. When infected in the first 3 months of pregnancy, fetal infection develops in 90% of cases. In addition, it has been established that with congenital rubella, late complications (panencephalitis, diabetes mellitus, thyroiditis) can also develop. The adverse effect of rubella infection on the fetus is also manifested by spontaneous abortions (10-40%), stillbirth (20%) and death in the neonatal period (10-25%). Of particular concern is the steady increase in the incidence of morbidity in women of childbearing age, resulting in an increase in the number of cases of congenital rubella syndrome, which manifests itself as congenital deformities. The number of cases of congenital rubella syndrome averages 0.13% of all diseases. According to WHO, rubella kills only about 300,000 children every year. The cost of treating and maintaining a child with congenital rubella syndrome is, according to conservative estimates, about $200,000.
Pathogenesis
Due to the lack of an experimental model for reproducing rubella, the pathogenesis of the disease has been little studied. Infection occurs through the mucous membranes of the upper respiratory tract, infection through the skin is possible. Following this, the virus penetrates the regional lymph nodes, where it reproduces and accumulates, which is accompanied by the development of lymphadenopathy. Subsequent viremia with hematogenous dissemination throughout the body occurs during the incubation period. The pathogen, having a tropism for the epithelium of the skin and lymphatic tissue, settles on the epithelium of the skin and in the lymph nodes. Viremia usually ends with the appearance of exanthema. At this time, virus-neutralizing antibodies are already detected in the blood of patients; subsequently, their concentration increases, and the developing immune reactions lead to the elimination of the pathogen from the body and recovery. After an illness, antibodies remain for life, which ensures the stability of post-infectious immunity.
When rubella develops in pregnant women during the period of viremia, the pathogen with the blood of the pregnant woman easily overcomes the placental barrier and infects the fetus. At the same time, due to viral damage to the endothelium of the blood vessels of the placenta, the nutrition of the fetus is disrupted. By damaging the genetic apparatus of cells, the virus selectively suppresses the mitotic activity of individual cell populations of the embryo and, possibly, has a direct cytopathogenic effect on them. This leads to slower growth and disruption of the normal formation of fetal organs with the subsequent development of congenital defects. The impact of the virus on embryonic tissues at different stages of pregnancy is ambiguous; it turns out to be most pronounced in relation to organs and systems that are at the stage of infection in the process of active formation.
Therefore, the widest range of fetal malformations occurs when infected in the early stages of pregnancy.
Clinical picture
Incubation period
is the same in children and adults and lasts 10-25 days.
The subsequent catarrhal period
in children, as a rule, is not expressed; in these cases, the diagnosis of rubella can often be established only after the appearance of exanthema. In adults, during this period there may be an increase in body temperature (in severe cases up to high numbers), malaise, headache, myalgia, and loss of appetite. Catarrhal phenomena can be expressed in the form of a slight runny nose and dry cough, a sore throat, photophobia and lacrimation. On examination, some patients are found to have conjunctivitis and redness of the mucous membrane of the pharynx. Enlargement and tenderness of the lymph nodes, especially the occipital and posterior cervical ones, are equally characteristic of both children and adults, but this symptom is not found in all patients. Subsequently, lymphadenopathy persists for quite a long time (up to 2-3 weeks). The duration of the catarrhal period is 1-3 days.
Then comes the period of exanthema;
manifestations of this main syndrome develop in 75-90% of patients already on the first day of illness, while rashes are more often observed in children. The rash elements are round or oval pink or red small spots with smooth edges. They are located on unchanged skin and do not rise above its surface. In adults, the rashes tend to merge; in children they rarely merge. Sometimes the appearance of a rash is preceded by itchy skin. Initially (but not always), elements of the rash appear on the face and neck, behind the ears and on the scalp. Then, during the day, they spread to various parts of the body without a specific pattern. The location of the rash is especially typical on the back, buttocks and on the extensor surfaces of the upper and lower extremities. There is no exanthema on the soles and palms. In some cases, simultaneously with exanthema, the appearance of enanthema on the mucous membranes of the oral cavity in the form of small single spots (Forchheimer spots) can be noted. In adult patients, the exanthema is more abundant and longer lasting; its elements can merge, forming erythematous fields. The confluent nature of the rash, as well as its absence in some patients (in 20-30% of cases, according to the literature) make it extremely difficult to make a clinical diagnosis.
During exanthema, body temperature may remain normal or rise slightly. Enlarged and moderately painful peripheral lymph nodes are clearly visible in all areas accessible to palpation, but especially in the occipital, parotid and posterior cervical areas. Some patients complain of joint and muscle pain. In some patients, dyspeptic symptoms, enlargement of the liver and spleen are noted, and in women - signs of polyarthritis. Typically, manifestations of exanthema last no more than 4 days. The rash can fade quickly and disappear without a trace.
Rubella in pregnant women: consequences for the child
In 1941, the Austrian researcher N. Gregg described anomalies in newborns whose mothers had rubella during pregnancy. Cataracts, deafness and heart defects are called Congenital Rubella Syndrome (CRU). Subsequently, the list of these vices expanded significantly.
Congenital rubella syndrome: timing and frequency of development
- Between 3 and 11 weeks of pregnancy, defects of the central nervous system develop. At 4–7 weeks of pregnancy, defects of the heart and visual organs develop. The incidence of malformations in the 3rd - 4th week of pregnancy is 60%.
- Between 7 and 12 weeks, hearing defects develop. The incidence of malformations during this period is 15%.
- The incidence of malformations at 13–16 weeks of pregnancy is 7%.
Rice. 7. Congenital rubella. Eye cataract.
Congenital rubella: list of fetal development defects
Congenital rubella syndrome today usually includes:
- Malformations of the heart, which manifest themselves in the form of patent ductus arteriosus, ventricular septal defect, pulmonary stenosis.
- Eye malformations manifest as corneal opacities, chorioretinitis, cataracts, microphthalmia, glaucoma and retinopathy.
- Deafness is one of the most common birth defects.
- Malformations of the central nervous system manifest themselves in the form of defects in the formation of the skull and brain (microcephaly), accompanied by mental retardation.
- Hypotrophy and intrauterine growth retardation.
- Malformations of internal organs: bone damage, enlarged liver and spleen, myocarditis, interstitial pneumonia, thrombocytopenic purpura, hemolytic anemia, dermatitis, etc.
Late malformations include thyroiditis, diabetes mellitus and progressive subacute panencephalitis.
More rare malformations include malformations of the skull, bone skeleton, genitourinary organs and digestive system.
Defects such as deafness, pathology of the heart and visual organs (congenital glaucoma, high degree of myopia) are difficult to recognize during the newborn period.
Chronic meningoencephalitis is difficult to recognize in a newborn. Lethargy, drowsiness or increased excitability and convulsions are its main symptoms.
It is difficult to recognize thyroiditis and diabetes mellitus in a newborn.
Rice. 8. Deafness, cataracts and heart defects make up the classic congenital rubella syndrome.
Tests for rubella during pregnancy
Modern diagnostics of rubella allows you to quickly make the correct diagnosis and prescribe adequate treatment, which can significantly alleviate the patient’s condition and carry out timely preventive measures, preventing infection of others and contact persons. The causative agents of the disease (viruses) contain substances (antigens) that can cause an immune response in the body of an infected person (the formation of antibodies). Antibodies and antigens are detected and studied using serological reactions. They are based on the body's immune reactions.
Testing for rubella during pregnancy using a serological research method is fundamental in diagnosing the disease and in identifying the level of protective antibodies in the blood that appear after vaccination in the past.
Antibodies to rubella during pregnancy are detected using the neutralization reaction (RN), complement fixation (RSF), hemagglutination inhibition (HAI), latex agglutination, radial hemolysis reaction (RHR), immunoblotting technique and “trap” ELISA. All of the above methods are inexpensive, sensitive and reliable.
Rice. 9. Set of reagents “BioScreen-Rubella-IgG”, which is used for the quantitative determination of specific antibodies (immunoglobulins).
How to distinguish a rubella rash from rashes of other diseases?
There are many diseases that are accompanied by the appearance of skin rashes.
However, there are some distinctive features of dermal damage that you need to focus on:
| Rubella | It focuses on the elbows, knees, face, shoulders and buttocks. The rash has a pale pink tint. |
| Measles | It covers the feet, face and upper body. The rash is bright, has a rich red color, and looks like tubercles. |
| Chickenpox | It is located on the scalp and is distributed throughout the body. The rash looks like spots that transform into blisters and fill with liquid. |
| Scarlet fever | Rashes appear on the body in the area of folds, on the face in the area of the nasolabial triangle. The elements of the rash themselves are small and bright. The patient's tongue takes on a crimson color. |
| Mononucleosis | Elements of the rash appear on the face, but they are also present on the torso. Sometimes the disease occurs without a rash at all. |
Most often, rubella is confused with measles. While scarlet fever is easier to differentiate from these diseases, since not only the skin, but also the tonsils suffer.
With rubella, the rash spreads quickly throughout the body. It can occupy the entire surface of the body in a few hours. With measles, this process is extended over 2-3 days. Measles rash tends to coalesce. This does not happen with rubella. The rash goes away quickly and leaves no traces behind. The root elements first become pale, peel off, and dark areas may remain in their place.
With roseola, the rash looks like papules, that is, tubercles that rise above the skin. In addition, body temperature rises greatly. There are no catarrhal symptoms.
In any case, the appearance of a skin rash is a reason to consult a doctor. Only a doctor can make the correct diagnosis and prescribe treatment.
Antibodies to rubella during pregnancy
Antibodies formed as a result of vaccination or after previously suffering from rubella penetrate the placenta and with mother's milk, protecting the fetus from infection and rubella during the first year of the unborn child's life. If a pregnant woman unprotected from rubella comes into contact with a patient, a disease may develop in which viruses can penetrate the fetus and cause the development of many malformations. Antibodies to rubella during pregnancy are determined using serological tests.
If a woman planning a pregnancy does not remember whether or not she was previously vaccinated against rubella, it is necessary to do an immunological test for the presence of anti-rubella antibodies in the blood.
Tests for rubella in pregnant women and their interpretation
- The “Anti-Rubella-IgM positive during pregnancy” test means that the pregnant woman has rubella. Antibodies - class M immunoglobulins are produced in the body of a pregnant woman during illness within 1 - 3 days.
- “Anti-Rubella-IgG positive during pregnancy” in a patient with rubella appears 3 to 4 weeks after the disease or their titer increases. This analysis helps to retrospectively assess the situation. An increase in antibody titer by four times or more indicates the severity of the disease.
Tests for rubella when planning pregnancy and their interpretation
- “Anti-Rubella-IgG positive during pregnancy” in a healthy woman means that anti-rubella antibodies are present in the blood. A positive test confirms a previous history of rubella or previous vaccination against the disease.
- If the level of anti-Rubella-IgG is less than 10 U/ml, this means that the amount of antibodies in a person’s blood is insufficient to protect against the disease. When the concentration of anti-Rubella-IgG is more than 10 U/ml, we can talk about the presence of immunity to infection.
- “Anti Rubella-IgG negative in pregnancy” means the absence of IgG antibodies. In this case, vaccination is indicated 2 months before the planned pregnancy.
Rice. 10. Cataract is one of the most common congenital defects associated with rubella.
Rubella rash
There are many diseases that are accompanied by the appearance of a rash on the body. Therefore, you need to know what features the rashes characteristic of rubella have.
The rash appears approximately 14 days after the infection occurs. It stays on the skin for about 5 days. The exact timing depends on the individual characteristics of the person’s immune system. If the defenses are fully activated, the rash may disappear after 2-3 days.
Distinctive characteristics of the rubella rash:
- First of all, the rash appears in the oral cavity. It looks like pink spots.
- Then rashes appear behind the ears, on the cheeks, near the lips, near the nose.
- After a few hours, the rash spreads throughout the body. It involves the buttocks, shoulders, elbows, hips and knees.
- The rash on the body will be more saturated in color than on the face.
- Sometimes there is no rash on the face at all, it appears only on the body.
- The size of the spots is kept within 5 mm. At first the spots will be flat, and then they will begin to rise above the surface of the skin.
- The elements of the rash are single, they do not merge with each other.
- If you press on the spot and then remove your finger, the rash will disappear, after which it will appear again.
- Rubella rashes do not affect the skin of the palms, soles and groin.
- The spots may be itchy, although for some patients they do not cause any discomfort.
- When the rash goes away, no traces of its presence remain on the skin.
- Sometimes rubella is asymptomatic. In this case, a rash does not appear on the body. A correct diagnosis can only be made through a blood test.
Measures to take if a pregnant woman comes into contact with a person with rubella
If a pregnant woman comes into contact with a patient, a serological blood test is performed to determine antibodies to Rubella virus.
- Antibodies to rubella of the IgG class are always present in the blood of a person who has previously had the disease or has been vaccinated. They provide protection to the body from re-infection. The absence of antibodies means that the pregnant woman is not protected from the disease and there is a risk of infection if she comes into contact with a sick person.
- In case of contact with a patient and in the absence of IgG antibodies in the blood of the pregnant woman, the test is repeated after 4 - 5 weeks. In case of a positive result (“Anti Rubella-IgG positive” during pregnancy), it is recommended to terminate the pregnancy. In case of a negative analysis, the test is repeated after 1 month. A negative test (“Anti Rubella-IgG negative” during pregnancy) indicates that the pregnant woman’s body did not become infected upon contact with the patient and the pregnancy can be saved.
- If, after contact with a patient, 2-4 weeks later, IgM antibodies and low-avidity IgG are detected in the blood of a pregnant woman, this indicates that infection has occurred. If infected in the first trimester, the pregnancy must be terminated. If infected at 14-16 weeks of pregnancy, the issue of terminating or continuing the pregnancy is decided at a medical consultation.
The absence of symptoms of rubella in a pregnant woman after contact with a sick person does not exclude the absence of the disease. The asymptomatic form of rubella poses the same danger to the fetus as the manifest form.
Rice. 11. Malformations of the central nervous system in congenital rubella manifest themselves in the form of defects in the formation of the skull and brain (microcephaly), accompanied by mental retardation.
Dear patients!
Measles is an acute viral disease transmitted by airborne droplets (by talking, coughing and sneezing). It is characterized by high body temperature (39.0 degrees C and above), a general severe condition, cough, runny nose, inflammation of the mucous membrane of the eyes (conjunctivitis) and rash.
The measles virus easily spreads over long distances - into neighboring rooms, through corridors, through the ventilation system. 95-96% of children who were in contact with sick people become infected. In the first 3-6 days, the disease looks like an acute respiratory viral infection, but already during this period you can see rashes characteristic of measles on the mucous membrane of the cheeks in the form of white dots. Over time, unlike ARVI, the temperature rises again and a rash gradually appears on the skin (it covers the face, neck, upper and then lower body, including arms and legs), going down from top to bottom within 4- 7 days. The rashes also disappear gradually (within 3-4 days), leaving pigmentation at the sites where they appeared, which also goes away after a few days. Children under one year old rarely get measles, since they are protected by antibodies - protective proteins produced by the mother after she suffered an illness or vaccination. By 9-12 months. During the first year of life, maternal antibodies disappear from the baby’s blood, and he remains defenseless against this disease. If a small child falls ill, especially one weakened by previous diseases or having a congenital pathology, death is possible. Death is recorded in 1 out of 2000-3000 sick children under 3 years of age (in developing countries this figure is 3-10% of sick children). This disease is very severe in adults.
Measles is dangerous due to its complications: such as otitis (ear inflammation; observed in 1 out of 20 cases), pneumonia (in 1 out of 25 cases), blood damage (thrombocytopenia - a reduced number of platelets, which is dangerous for bleeding; observed in 1 out of 3000 cases) , convulsions that develop against the background of high body temperature (in 1 out of 200 cases), as well as inflammation of the brain, encephalitis; in 1 out of 1000 cases).
In addition, after measles, the person who has recovered from the disease temporarily develops a state of immunodeficiency (decreased protection against other infections), which contributes to the accumulation of severe bacterial infections.
Rubella is an acute viral infection transmitted by airborne droplets. In children, as a rule, it occurs mildly or in the form of a disease of moderate severity. People usually get sick 11-21 (rarely 23 days) after contact with a sick person. The first 1-5 days of the illness are characterized by a rise in temperature to 38 degrees C, malaise, headache, enlarged lymph nodes, especially on the back of the head, behind the ears, and sometimes conjunctivitis. A finely spotted rash appears on the skin, which is located mainly on the lateral surfaces of the torso and limbs, and lasts up to 5 days. In general, the duration of the disease is 1-2 weeks. Complications are very rare, but the development of encephalitis (inflammation of the brain) is possible in 1 in 1000 patients.
Rubella is most dangerous for pregnant women, because this virus is capable of infecting all tissues of the fetus. If a woman gets rubella in the first half of pregnancy, especially in the first 3 months, the result may be a miscarriage or a stillborn baby. It is also possible that a baby will be born with congenital rubella syndrome (CRS), which includes a triad of developmental defects: - congenital heart disease, blindness (cataracts) and deafness. In addition, SHS is characterized by brain damage, including mental retardation, as well as damage to the liver, spleen, platelets and other congenital disorders.
A woman can get over rubella unnoticed: if she feels normal, a minor rash appears for 1-2 days, which is sometimes ignored. And the virus, circulating in the blood of a pregnant woman, passes through the placenta to the fetus. Therefore, if a pregnant woman is suspected of being infected with rubella, it is necessary to conduct a special study (the blood is tested twice for the content of anti-rubella antibodies, and if their number increases significantly, which indicates a history of rubella, the question of terminating the pregnancy arises in the early stages, since there is a high risk of giving birth to a child with deformities).
11-30% of women of childbearing age are not protected from rubella.
If a girl or young woman has not had rubella and is not vaccinated, then before planning a pregnancy she herself needs to think about the appropriate vaccination. Vaccination protects almost 100%, immunity after a single vaccination lasts on average 15-20 years, then immunization can be repeated .
It must be remembered that after the administration of the rubella vaccine, it is not recommended to become pregnant for 3 months. If pregnancy occurred earlier than this period or a woman already expecting a child was vaccinated, this is not an indication for termination of pregnancy.
Mumps (“mumps”) is an acute viral infection transmitted by airborne droplets and affecting the parotid and submandibular salivary glands. They swell, causing the face to become rounded (hence the name “mumps”). This virus does not spread as widely in the environment as measles and rubella. If a sick child is isolated in a room, then children and adults who are not in direct contact with him do not become infected.
The disease begins with low fever and malaise, and after 1-3 days one or both salivary glands enlarge, making it painful to chew and swallow.
When examining the buccal mucosa, an inflamed papilla of the excretory duct of the salivary gland is visible on the affected side. In addition to the salivary glands, in approximately 4% of cases, the mumps virus can cause inflammation of the pancreas (pancreatitis), as well as the membranes of the brain (meningitis) in 1 out of 200-5000 cases, very rarely (1 in 10,000 cases) it is involved in the process brain tissue, then meningoencephalitis develops (inflammation of the membranes and substance of the brain).
Mumps is dangerous due to complications. In 20-30% of sick teenage boys and men, the testicles become inflamed (orchitis); in 5% of girls and women, the mumps virus affects the ovaries (oophoritis). Both of these processes can cause infertility. Possible fatalities 1:10,000 cases.
All three infections (measles, rubella, mumps) are caused by viruses and do not have specific antiviral therapy. That is, there are no drugs that would prevent the severe course of the disease and complications. Therefore, the main means of preventing these infections is immunization.
Susanna Kharit, pediatrician, head of the immunoprophylaxis department of the Research Institute of Children's Infections of the Ministry of Health of the Russian Federation, Doctor of Medical Sciences.
Rubella vaccine before pregnancy
If there are no IgG antibodies in the blood, the woman is vaccinated two months before the planned pregnancy. In the Russian Federation, the monovaccine Rudivax (France) and Rubella vaccines (India and Croatia) are used for these purposes.
- Before pregnancy, the rubella vaccine is administered intramuscularly into the shoulder area in a volume of 0.5 ml.
- Immunity after vaccination develops after 15-20 days and lasts for 15-25 years.
Rice. 13. Vaccination against rubella before pregnancy will prevent the birth of a sick child.
Vaccination against rubella during pregnancy
Despite the fact that accidental rubella vaccination during pregnancy does not have a negative effect on the fetus, pregnancy today is a contraindication for vaccination.
According to the latest data (more than 1000 pregnant women were studied), when pregnant women who denied pregnancy were vaccinated, infection of the fetus with vaccine viruses was quite often observed, but this did not in any way affect its development. Occasional rubella vaccination during pregnancy is not an indication for termination of pregnancy.
Consequences of the rubella vaccine
Rubella vaccination before pregnancy: consequences
- Reactions to rubella vaccination are rarely recorded.
- It may manifest as local tenderness, fever, and enlarged occipital lymph nodes.
- Transient acute arthritis and arthralgia appear 1 to 3 weeks after vaccination. More often the knee and wrist joints are involved in the process. The complication is registered in girls and young women.
- Vaccine reactions such as anaphylactic reaction and thrombocytopenia have been reported rarely.
- A reaction to a vaccine can develop as a result of errors that occur during immunization: administration of an increased dose of the vaccine, violation of the route of administration of the drug, violation of antiseptic rules.
Rubella vaccination during pregnancy: consequences
According to the latest data (more than 1000 pregnant women were studied), when vaccinating pregnant women who denied pregnancy, infection of the fetus was quite often observed, but this did not in any way affect its development.