Rubella is an acute, contagious viral infection. While the rubella virus usually causes a mild fever and rash in children and adults, infection of a woman during pregnancy, especially in the first trimester, can lead to miscarriage, fetal death, stillbirth, or congenital malformations in the infant, known as congenital rubella syndrome (CRS). ).
The rubella virus is spread through respiratory droplets when an infected person sneezes or coughs. Humans are the only known carrier of the rubella virus.
Definition of disease
Rubella is a viral infection caused by the Rubella virus. It is extremely contagious, occurs in an acute form, causes fever and the appearance of a red rash on the skin. Children get it more often, but they tolerate the disease more easily compared to adults. The older the infected person, the more severe the symptoms of rubella will be¹.
Rubella and measles: what is the difference
Rubella is often confused with measles. Both diseases are considered “childhood” diseases, have a similar course, and even vaccination against them is carried out simultaneously. The difference is in the causative agent (they are caused by different viruses), as well as in the course of the disease and the level of contagiousness and risk of complications. Compared to measles, rubella is a less dangerous disease, in which the rash is not as severe, passes faster, and the temperature most often rises slightly. Measles is a disease with a severe course, a high risk of complications, and one of the leading causes of child mortality.
What vaccinations are there for measles, rubella and mumps?
All measles, rubella, and mumps vaccines are live attenuated vaccines. This means that the drug contains live viruses grown under artificial conditions and “weakened” in a special way. So that they cannot cause a full-fledged disease, but at the same time they form stable lifelong immunity. Attempts to create inactivated (non-live) vaccines against these infections have been unsuccessful. Such vaccines turned out to be too “weak”, unable to induce lasting immunity.
Among the vaccines are:
— monovaccines. Separately mumps, measles and rubella;
- divaccines. The mumps-measles vaccine is widespread in our country;
- and trivaccines. This group includes the MMP and Priorix vaccines. Such vaccines are preferable because instead of two or three injections, the child receives only one injection.
Rubella symptoms
What the symptoms of infection will be and how severe they will be depend on the age at which the person becomes ill. Children tolerate the disease easily. Their temperature rises slightly and a red rash appears. Teenagers and adults are more severely affected and may feel very unwell.
Rash on the body due to rubella. Source: PHIL CDC
The following symptoms may appear with rubella:
- Fever and chills. The temperature is often low-grade: from 37.0 to 37.5°C, but can rise to 39°C.
- Rash on the body. The rash first appears on the skin of the face and neck, and then spreads throughout the body. The rash may last 1 to 3 days or longer. Appears in most patients (but not in all cases).
- Enlarged lymph nodes. The lymph nodes in the neck and behind the ears may become inflamed 1-3 days before the skin rash appears.
- General malaise. Associated with intoxication due to infection, manifested by weakness, fatigue, headaches, muscle and joint pain, and loss of appetite.
- Respiratory symptoms. Sometimes a slight dry cough, runny or stuffy nose, and sore throat may appear.
- Conjunctivitis. Inflammation of the mucous membrane of the eye, accompanied by redness, lacrimation and photophobia².
How can you tell if a rash is caused by rubella?
With rubella, the rash is small and quickly spreads throughout the body from top to bottom, except on the palms and soles of the feet.
Typical places for a rash are any folds of skin, especially the folds at the elbows and behind the knees. It looks like small pale pink or red spots. The rash may be mildly itchy. The skin at the site of the rash usually does not peel off, and no ulcers, ulcers or pigmentation appear. The rash goes away quickly, without leaving a trace. In addition to skin rashes with rubella, a rash may appear on the palate: redness and the formation of small pale pink spots. Rash on the abdomen due to measles. Photo: Photo: PHIL CDC
In children, a rash is often the first noticeable sign of infection, and only after its appearance do other symptoms appear: fever, swollen lymph nodes, malaise. In adults, with the appearance of rashes, symptoms noticeably intensify and health worsens.
In adolescents and adults, the disease is often severe, and then the following symptoms appear:
- high body temperature (above 39°C) for two days or more;
- severe intoxication (weakness, headaches, muscle, joint pain) that persists for four days or more;
- cough, severe runny nose, nasal congestion;
- severe enlargement, inflammation of the lymph nodes behind the ears and on the neck;
- rashes on the skin in which individual spots merge with each other.
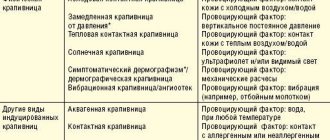
How to distinguish rubella from other diseases?
Some symptoms of rubella are similar to measles, allergic rashes and other diseases. They are treated differently, so it is important to understand. Clinical manifestations of similar diseases:
- Measles: runny nose, sore throat, and conjunctivitis are more pronounced. The rash takes the form of small nodules, merges into spots, and spreads throughout the body more slowly.
- Pseudotuberculosis: absence of runny nose and cough, enlarged lymph nodes. The rash is pinpointed, in the form of papules (small nodules).
- Allergies: The rash appears after contact with an allergen and causes severe itching. However, there are no other symptoms (runny nose, sore throat, conjunctivitis, fever or weakness).
- Scarlet fever: This is a bacterial infection that causes inflammation of the tonsils, high fever, and a coating on the tongue. A characteristic feature is that the rashes are concentrated in areas of natural folds (armpits, groin folds, etc.).
- Infectious mononucleosis: noticeable malaise can persist for up to two months, severe inflammation of the throat mucosa, skin rashes rarely appear.
Figure 1. Location of the rash on the body in various diseases. Source: Artemida-psy / Depositphotos
Couple treatment of male infertility
Infertility in a married couple can be male, female or combined. But even dividing the problem in this way, you should not put the entire burden of treatment on one partner. The fight against infertility is always a mutual process, in which the psychological atmosphere in the family will play a huge role. The feeling of illness and of being “wrong” can cause a feeling of guilt in a family member and create additional stress, which will not have a favorable effect on preparing for the role of a parent. Particular attention should be paid to the situation of joint treatment of female and male infertility. In approximately a third of all cases of this diagnosis, the problem of infertility or simply reduced reproductive functions affects both partners.
The causes of the problem may lie in pathological disorders of the reproductive system of both women and men, which will entail specific diagnoses and treatment strategies, or they may have an unclear etiology, which will lead to a diagnosis of infertility of unknown origin. And as practice shows, even absolutely healthy men and women can actually have problems conceiving a child. According to statistics, such couples account for approximately 20% of couples with general infertility.
Each case of combinations of women's and men's health problems is quite unique, and therefore requires an individual approach and a responsible attitude on the part of the couple. Essentially, when treating female and male infertility, each person fine-tunes their own “reproductive mechanism,” but besides this, it is important to make sure that the partners tune in to each other. Spending time together in special medical sanatoriums can help with this.
Complications of rubella
Complications of congenital and acquired rubella differ. Acquired rubella in children most often resolves without health consequences. Complications are rare and occur mainly in adults and children with immunodeficiency. Possible complications² include:
- Arthritis. Joint pain appears 1-2 days after the rash disappears. The pain persists for up to 5-10 days, and then goes away without consequences.
- Thrombocytopenic purpura. The disease is associated with impaired immunity and is characterized by a decrease in platelets in the peripheral blood, which causes hemorrhagic syndrome - a rash on the skin and mucous membranes, bleeding gums, as well as the appearance of blood in the urine. It can last up to 6 months and usually goes away on its own.
- Encephalitis. A rare complication that can begin five days after the formation of skin rashes. The onset is always acute: fever, severe headaches. Without treatment, symptoms may increase, seizures may occur, and coma may develop. With timely treatment, the prognosis is favorable.
When a child is infected in utero, congenital rubella syndrome (CRS) develops. This is a serious disease for a newborn, so women who contract rubella during pregnancy are advised to terminate it, regardless of the period. Complications of CRS in a newborn are in the nature of congenital malformations:
- heart: pulmonary artery stenosis, damage to the cardiac septum or valve apparatus, patent ductus arteriosus;
- hearing: decreased or deafness
- vision: congenital glaucoma, cataracts, strabismus, nystagmus (trembling of the eyeball), microphthalmia (reduction in the size of the eyeball);
- brain: hydrocephalus (accumulation of cerebrospinal fluid in the ventricles inside the brain and increased pressure on the brain);
- facial skeleton: non-fusion of the hard or soft palate;
- mental retardation;
- neurological disorders⁶.
These conditions can cause disability or threaten the child's life.
Rubella in a newborn. Photo: Indian journal of dermatology / Open-i (CC BY-NC-SA 3.0)
Based on the severity of the disease, there are mild, moderate and severe degrees. Children usually have mild rubella, but moderate and severe rubella are more common in adolescents and adults.
Does rubella in pregnant women always lead to serious consequences?
If a pregnant woman becomes infected with rubella, the risk of transmitting the infection to the fetus is very high. The likelihood of negative consequences depends on at what stage of pregnancy the infection occurred. At an earlier stage, the risk of fetal death or the development of congenital rubella syndrome is higher. If infected before 12 weeks, the risk of developing severe birth defects is 80-90%. If a pregnant woman becomes infected with rubella at 13-15 weeks, the likelihood of developing birth defects for the child is reduced to 15-17%. If infected after the 20th week, the risk of developing a congenital infection remains. The risk of fetal death in the first trimester is 7.2%, in the second trimester - up to 5.6%, in the third trimester - up to 1.7%⁴.
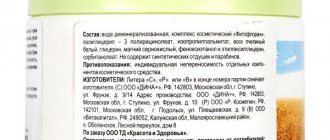
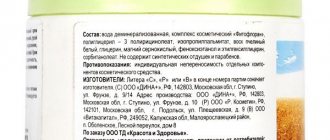
Treatment of rubella
There are no specific medications to treat the rubella virus. Treatment is generally given to relieve symptoms associated with the infection:
- If a rash appears, fever, or malaise, bed rest and drinking plenty of fluids are recommended.
- If you have a runny nose or conjunctivitis, your doctor may recommend taking antihistamines.
- To reduce elevated temperature, antipyretics (paracetamol) are prescribed.
Rubella is not treated with antibiotics.
Therapy is symptomatic; for example, the child may be prescribed antipyretics. Photo: natapetrovich / Depositphotos Also, if indicated, it is possible to prescribe anticonvulsant, anti-edematous, anti-inflammatory drugs⁵.\
Important!
When treating rubella, antibiotics are used only if there are complications in the form of an associated bacterial infection. Antibacterial therapy is not effective against the virus, and its use can be dangerous. Any medications used to treat rubella should be prescribed by a doctor.
If specific complications occur, the attending physician or pediatrician will refer you to a specialized specialist (for example, an infectious disease specialist or neurologist).
Nutrition for rubella
If rubella is moderate or severe, your doctor may recommend a special diet. Usually this is treatment table No. 13 according to Pevzner, used for acute infectious diseases. It has several features:
- diet - 5-6 times a day;
- exclude any fresh bread, butter dough;
- soups should be low-fat, meat or fish, seasoned with cereals or vegetables;
- lean meat and fish, boiled or steamed;
- exclude pasta, legumes, barley, millet, pearl barley, and corn from the diet;
- rolled oats, ground buckwheat or semolina semi-viscous porridge are allowed;
- dairy products are allowed with the exception of cream, full-fat sour cream and whole milk;
- All vegetables and fruits are allowed, except those rich in fiber and having rough skin, as well as cabbage, mushrooms, onions and garlic, radishes, turnips, rutabaga, cucumbers;
- The only sweets you can eat are marmalade;
- Fats allowed include butter and refined vegetable oil;
- Drinks allowed are weak tea and coffee, fruit drinks, diluted juices, and decoctions.
Rubella is a highly contagious disease, so it is important to stop the spread of the virus. If the patient is being treated at home, he must be isolated and contact with non-sick, unvaccinated people should be excluded. If this is not possible, hospitalization in an isolated department (box) of an infectious diseases hospital is recommended.
When rubella requires urgent or emergency hospitalization:
- Children under 5 years of age with a severe course of the disease (refuse to eat or drink, have nausea after every meal or drink, the disease is accompanied by convulsions, loss of consciousness).
- In case of moderate or severe rubella: high temperature, which cannot be reduced with antipyretics, severe intoxication (weakness, nausea, vomiting, dehydration, headaches, muscle and joint pain).
- Concomitant chronic diseases, the course of which may be complicated by the rubella virus.
- The development of complications such as: encephalitis, meningoencephalitis, pneumonia, thrombocytopenic purpura, etc.
Treatment of congenital rubella syndrome
Children with congenital rubella syndrome require constant medical supervision. Treatment of such children is symptomatic and is intended to mitigate the effects of infection⁵.
When organizing medical care for newborns with CRS, it is taken into account that the child secretes virions for a long time and remains infectious. Samples are taken periodically to assess the presence and shedding of the virus. Until these tests come back negative, precautions are taken to prevent the spread of infection.
Treatment of male infertility with hirudotherapy (leeches)
Among the non-traditional methods of treatment, it is worth noting the use of hirudotherapy for male infertility. Under the influence of leeches, blood circulation in the pelvic organs improves, erection and spermatogenesis improve, and congestive and inflammatory processes are eliminated.
Hirudotherapy for male infertility is used as an auxiliary treatment for certain forms of infertility. For example, if it is associated with the inflammatory process of the prostate gland. Hirudotherapy for male infertility can only be recommended by a doctor if he is confident in the effectiveness of this treatment method in your case. The same can be said about herbs for men against infertility, which can be prescribed by a doctor in complex therapy and are most often used in the form of dietary supplements for oligospermia. The effect of this treatment has not been proven.
Routes of infection: acquired and congenital rubella
There are two routes of rubella infection: airborne and transplacental³.
Most often, the infection is transmitted by airborne droplets during prolonged and close contact with an infected person. The incubation period (from infection to the appearance of signs of illness) lasts from 12 to 23 days. In the last week of this period, although there are no symptoms yet, the person becomes contagious and continues to spread the virus for another week after the rash appears.
The transplacental route involves transmission of infection from a pregnant woman to the fetus. As a result, the child may be born with congenital rubella syndrome (CRS). Such children can spread the infection until they are two years old.
Prevention
The following precautions will help reduce the risk of contracting rubella:
- Avoid contact with people with rubella.
- Limit contact with people with fever, runny nose, cough, sore throat, or skin rash.
- Compliance with personal hygiene rules, frequent hand washing, regular ventilation of premises.
When rubella is detected, doctors monitor the patient, as well as those who came into contact with him. To stop the spread of infection, it is necessary to exclude contacts of people without immunity with those who are already sick.
Rubella is highly contagious and spreads quickly. You can become infected with it even from a person who has no symptoms of the disease, for example, if the incubation period has not yet ended or the disease is asymptomatic. Therefore, the only reliable method of prevention is vaccination.
Vaccination
If a pregnant woman has immunity to rubella (after an illness or vaccination), the child also receives it. The baby's immunity lasts up to six months, gradually weakening. Next, to protect the child from infection, vaccination is carried out. Without vaccination, a child’s risk of contracting rubella increases: unvaccinated children aged 2 to 9 years are most likely to get sick. Vaccination with even one dose provides long-lasting immunity in 95% of cases⁶.
The vaccination is done two times:
- at the age of 12 months;
- revaccination at the age of 6 years.
If a person has not been vaccinated at all or has received only one vaccination (without revaccination), and there is no accurate information about vaccinations, an IgG test for the rubella virus does not detect antibodies, you can get vaccinated at any age. This is especially important for women planning pregnancy.
Rubella vaccination: questions and answers
What vaccine is used to prevent rubella?
Children are usually vaccinated with the combined measles, rubella and mumps vaccine.
A cultured live vaccine is used. It contains a weakened virus that is unable to infect cells but produces an immune response. A monocomponent vaccine can also be used - only against rubella. It is used to prevent infection in both children and adults. The monocomponent vaccine can be used for revaccination of young women planning pregnancy.
How is vaccination against rubella carried out?
During vaccination, a subcutaneous injection is given in the shoulder from the outside. The rubella vaccine is combined with other vaccines as follows:
- On the same day, you can vaccinate against rubella and do other vaccinations included in the National Calendar: hepatitis B, polio, tetanus, diphtheria, whooping cough. The injections are given with different syringes and in different areas of the body.
- If there is an interval between vaccinations, it should be at least 1 month.
- If immunoglobulins, plasma and other blood products were administered, the complex vaccine (against measles, rubella and mumps) can be used only after 3 months. If the vaccination has already been done, blood products can only be administered after two weeks. If you need to introduce them earlier, a revaccination will be required three months after their introduction.
- Tuberculin tests can be done only 4-6 months after immunization against rubella.
- When planning a pregnancy, you need to get vaccinated against rubella 1 month before conception or earlier.
How safe is the rubella vaccine?
The rubella vaccine is safe and the risk of complications from its use is minimal. After vaccination, the following reactions may occur:
- slight redness and pain at the injection site;
- slight increase in temperature;
- very rarely - slight inflammation of the lymph nodes or the appearance of a rash;
- In adults, joint pain and muscle pain are possible.
All these reactions manifest themselves in a mild form and pass quickly. No serious complications have been recorded after rubella vaccination.
When should you not be vaccinated against rubella?
Contraindications for rubella vaccination:
- Malignant neoplasms and blood diseases.
- Immunodeficiency conditions, excluding HIV infection. People living with HIV can receive the rubella vaccine.
- With a previous vaccination, there was a strong reaction to the vaccine (temperature above 40°C, severe swelling and redness at the injection site).
- The presence of any acute diseases (not necessarily infectious).
- Exacerbation of chronic diseases.
- Pregnancy.
In case of acute diseases or exacerbations of chronic diseases, vaccination can be done a month after recovery. If a person is undergoing radiation therapy or treatment with immunosuppressants, vaccination can be done no earlier than one year after completion of treatment.
WHO activities
WHO recommends that all countries that have not yet introduced rubella vaccine should consider introducing it as part of existing, sustainable measles immunization programs. To date, the goal of eliminating this preventable cause of birth defects has been set in four WHO regions. In 2015, the WHO Region of the Americas became the first region in the world to be declared free of endemic rubella transmission.
The number of countries using rubella vaccines as part of their national immunization programs is steadily increasing. As of December 2022, rubella vaccination had been introduced in 168 of 194 countries, and the average global rubella vaccination coverage was estimated to be 69%. The number of reported cases of rubella decreased by 97% from 670 894 cases in 102 countries in 2000 to 14 621 cases in 151 countries in 2022. Among WHO regions, the prevalence of CRS is highest in the African and South-East Asia Regions, where Vaccination coverage is at its lowest level.
In April 2012, the Measles Initiative—now known as the Measles and Rubella Initiative—launched the Global Measles and Rubella Strategic Plan, which sets a number of global measles and rubella targets through 2022. gg.
By the end of 2022
- Complete the elimination of measles and rubella in at least 5 WHO regions.
Rubella control is underperforming, according to the 2022 Global Vaccine Action Plan (GVAP) progress report prepared by the WHO Strategic Advisory Group of Experts (SAGE) on Immunization.
For example, 42 countries have not yet introduced rubella vaccination, and two regions (the African Region and the Eastern Mediterranean Region) have not yet set rubella elimination or control targets. To further combat this disease, SAGE recommends that rubella vaccination be included in immunization programs as soon as possible. As a founding member of the Measles and Rubella Initiative, WHO provides technical support to governments and communities to improve routine immunization programs and targeted vaccination campaigns. In addition, the WHO Global Measles and Rubella Laboratory Network provides support for diagnosing cases of rubella and CRS and tracking the spread of rubella viruses.
Diagnosis of rubella
First, the therapist or pediatrician conducts a general examination:
- measuring body temperature;
- examination of the skin for the presence of a rash;
- palpation of the lymph nodes in the neck and behind the ears;
- examination of the throat, pharynx (may be red);
- eye examination (signs of conjunctivitis).
Figure 2. Clinical manifestations of rubella.
Source: kavusta / Depositphotos You need to tell the doctor about your symptoms, for example, a runny nose or cough, weakness, general malaise, headache or other changes in well-being. Be sure to report contact with a person with rubella in the last 11-21 days.
During the examination, great importance is attached to the presence of a rash and the condition of the lymph nodes. With rubella, the lymph nodes in the neck and behind the ears are slightly enlarged (to the size of a bean) and may be painful and sensitive. Typically, the lymph nodes are enlarged before the rash appears and remain that way for some time after the rash has cleared¹.
The rubella rash is red or pinkish and consists of small spots or spots combined with small nodules. The skin, not covered with rashes, does not change (does not become dry, does not peel, there are no signs of inflammation, etc.). The rash first appears on the face and then spreads to the neck and chest, abdomen, arms and legs. Then the rash goes away without a trace, leaving no peeling or pigmentation.
Laboratory tests² for suspected rubella:
- a detailed clinical blood test to identify bacterial complications;
- enzyme-linked immunosorbent test (ELISA) to detect specific antibodies to the rubella virus and change their titer (except for cases of antibody formation after vaccination);
- PCR study to detect RNA of the Rubella virus;
- clinical urine analysis.
Instrumental diagnostics for the development of rubella complications: X-ray or CT of the chest if pneumonia is suspected, as well as CT or MRI of the brain if encephalopathy or seizures develop.
Examination of pregnant women with suspected rubella
Preventive diagnostics are carried out for pregnant women after contact with rubella patients. It is especially important for those who have not been vaccinated and have never had rubella. The examination is carried out by monitoring the state of health, blood tests are prescribed to determine antibodies to rubella of the IgM and IgG classes. The appearance of IgM antibodies in the blood plasma indicates the presence of infection. The presence of IgG antibodies in the blood plasma indicates that there is immunity to the pathogen. Taking this into account, pregnant women undergo enzyme immunoassay of blood plasma.
Further management of pregnancy depends on the results of the study:
- There are no IgM, there is IgG - there is no infection, there is immunity, there is no risk to the fetus. A repeat study is scheduled after 10-14 days to eliminate errors in the analysis.
- IgM and IgG are absent - there is no infection, no immunity. It is necessary to exclude contact with the sick person and conduct another test. Repeated analysis is carried out after 10-14 days. If the result does not change, stop observation. If IgM antibodies and later IgG antibodies are detected, it means that the woman has suffered from the disease and there is a risk of CRS for the fetus.
- There are IgM and IgG - there is immunity and there is an infection. The test is repeated to confirm the result. If it does not change, then the fetus is at risk of CRS.
If test results show that a pregnant woman has suffered from rubella and there is a risk of intrauterine infection for the baby, the doctor will warn about the possible risks and suggest terminating the pregnancy.
Diagnosis of infertility in men
What should you do if you suspect male infertility and how to identify it? It is best to immediately contact an andrologist - a doctor who diagnoses male infertility. Today, in case of an infertile marriage, it is considered economically feasible to first test for infertility in a man, and then examine the woman. Whatever the reasons for male infertility, there will always be changes in the spermogram. The test begins with the man having to undergo a test - submitting sperm for analysis.
Sperm testing allows you to determine the total number and activity of sperm, and the level of acidity. Further, if there are abnormalities in the spermogram, the examination consists of a microbiological examination of sperm, ultrasound and x-ray diagnostics of the pelvic organs.
Ultrasound diagnostics of male infertility can reveal abnormalities in the structure of the testicles, prostate gland and some developmental anomalies.
How to determine infertility in a man if it is associated with the patency of his vas deferens?
In this case, X-ray diagnostics using contrast is used.
Diagnosis also includes hormonal testing. Hormone studies can help establish hormonal infertility. Genetic testing reveals genetic infertility.
An immunological study reveals immunological male infertility. For this purpose, a MAP test of sperm and blood, a postcoital test and a latex agglutination test are performed.
Classification
There are several clinical forms of rubella. They all occur differently and have different risks of complications and health consequences.
Acquired rubella can occur in a typical, atypical or subclinical form:
- In the typical form, the usual signs of the disease appear: a red rash that gradually spreads throughout the body, fever, swollen lymph nodes, and malaise.
- With an atypical or erased form, not all symptoms appear. There is no rash, and the patient is only worried about enlarged lymph nodes, pain, sore throat, slight runny nose, and cough.
- In the subclinical form, the course of the disease is asymptomatic; it has no manifestations at all. It is possible to understand that a person has suffered an infection only if he came into contact with a person with rubella and after that he developed antibodies.
Complications can occur after rubella in a typical or atypical form. If the infection is asymptomatic, it is possible to avoid health consequences after the illness.
Causes of male infertility
Male infertility means the inability of a man to impregnate a woman. This problem can be discussed if a woman does not become pregnant within a year after the start of regular sexual activity without contraceptives.
Infertility in men can have various causes, but it is always based on three main factors:
- impaired viability or motility of sperm;
- significant decrease in sperm count;
- disruption of the passage of sperm through the vas deferens.
Congenital or acquired diseases can lead to such consequences. Thus, the most common causes of male infertility are:
- varicocele;
- testicular injuries, torsion;
- infectious diseases (infertility in men and mumps are closely related conditions; sexually transmitted infections can also lead to reproductive dysfunction);
- inflammatory diseases of the prostate gland, urethra;
- immunological and hormonal disorders;
- exposure to toxic substances: alcohol, drugs, certain medications.
First of all, a man should undergo the necessary tests to detect and confirm the fact of infertility. This can be done at a family planning center or a male infertility clinic. If you are interested in treatment in Moscow, then there will be no problems with this, since in any medical center there is a specialized doctor - andrologist. If there are no such clinics in your city, you can get tested for infertility by a urologist or andrologist at a local clinic.
Infectious mumps (mumps) as a cause of infertility
According to statistics, every fourth infertile man acquired this disease after suffering from infectious mumps, which is popularly called mumps. Infertility in men after mumps develops due to the fact that the mumps virus affects the gonads (testes in boys). A complication of mumps is manifested by orchitis (inflammation of the testicle), which also negatively affects the reproductive capabilities of men. It should be noted that mumps does not always affect the testicles; this only occurs with severe orchitis. Milder forms of mumps may have no effect on testicular development in future men!
Sources
- Mayo Clinic. Rubella. 2022.
- Brenda L. Tesini. Rubella. MSD Handbook, 2022.
- FBUZ "Center for Hygienic Education of the Population" of Rospotrebnadzor. Rubella.
- Antipova A.Yu. Rubella virus and its teratogenic effect. Pathogenesis, clinical picture, diagnosis, prevention of congenital rubella syndrome // Infection and immunity. 2011. T. 1. No. 2. Page. 131–134.
- World Health Organization. Rubella. 2022.
- National Association of Healthcare Associated Infection Control Professionals. Rubella. Vaccination experts. 2022.
Specialists
| 4.8 88 reviews | Lebed Dmitry Nikolaevich Therapist Experience 27 years Admission from 2500 rub. |
| 4.6 2 reviews | Tikhonova Irina Igorevna Therapist Experience 19 years Doctor of the highest category Admission from 5000 rub. |
| 4.4 4 reviews | Belyaeva Iraida Viktorovna Therapist 23 years of experience Doctor of the second category Admission from 7420 rub. |