Mycoses of large folds (MCF) are a significant interdisciplinary problem [1–6]. They represent a group of diseases united by the principle of selective localization in the area of large skin folds [7]. However, they receive less attention than mycoses of the feet (MF). Dermatophytosis of the feet is registered 3 times more often than dermatophytosis of other localizations combined [8, 9]. The problem of the ISS is the subject of research by domestic scientists [2, 10-12]. The relevance of the ISS problem was analyzed in detail by the authors of this article in 2015 [12].
The etiological factor of rubromycosis of large folds (RMF) is Tr. rubrum,
which, according to researchers [13-16], is the leader among the causative agents of dermatophytosis at present.
However, the frequency of its verification during examination of patients with MCS in Russia is only 15-20%, and in the Republic of Kyrgyzstan, for example, 25% [17, 18], in Italy, during examination from 2005 to 2010, more than 6 thousand patients with dermatophytosis were identified skin. Among the clinical forms of dermatophytosis, inguinal dermatophytosis was in the lead (39.2%), 2nd place was occupied by mycosis of the trunk (22.7%) and MS (20.4%), Tr. predominated in the structure of the cultured pathogens. r ubrum
(64%) [19]. In a multicenter open-label controlled study in the Russian Federation in 1999 involving 14 specialized institutions, 160 patients with superficial mycoses of the skin (SMC) were examined. Rubromycosis was represented by rubromycosis of the feet (52.9%), large folds (26.5%) and their combination (20.6%) [20]. According to the State Scientific Center for Dermatovenerology and Cosmetology, the mycological center at the City Clinical Dermatovenerological Dispensary (Moscow) and the Department of Skin and Sexually Transmitted Diseases of the Military Medical Academy named after. CM. Kirov (St. Petersburg), among 120 patients with MVP, rubromycosis of smooth skin and large folds in combination with MS accounted for 28.3% [21].
Dermatophytosis of large folds (LCF) is often recorded against the background of somatic diseases (diabetes mellitus, oncological processes, vegetative-vascular dystonia, chronic venous insufficiency, hepatitis and others) [4, 22-24]. They can occur when patients are prescribed systemic glucocorticosteroids for various diseases (rheumatoid arthritis, bronchial asthma, systemic lupus erythematosus, pemphigus, T-cell lymphoma, etc.) [25-27]. A particularly severe course of DCS has been reported in HIV-infected patients [28, 29]. Dermatophytes can infect large folds that are involved in the process of dermatoses of various origins. It is no coincidence that the term “dermatoses of combined etiology” appeared in the literature [30].
The clinical picture of DCS is determined by the pathogenicity and virulence of the pathogen, the state of the human body and environmental conditions. The manifestations of the disease are caused, on the one hand, by the destruction of the stratum corneum of the epidermis due to the growth and reproduction of fungi, and on the other, by a pronounced inflammatory reaction of the dermis. Lesions have the ability to grow peripherally due to proliferative activity, which increases 4 times in the focal area. At the same time, the rate of fungal reproduction outstrips the development of the body’s defense reactions [10, 31]. Dermatophytes are characterized by dermatotropism, keratolytic and lipolytic activity. The enzyme keratinase destroys and utilizes only human keratin. If the rate of proliferation of the epidermis exceeds the rate of reproduction of the fungus, then elimination of the pathogen and spontaneous recovery are possible [1, 10]. In chronic rubrophytosis, the infection from the feet spreads to the nails, palms, and then to smooth skin and to the area of large folds. Often recurrent onychomycosis (OM) of the feet is the cause of persistent MCS [32]. DCS is more often recorded in obese men suffering from excessive sweating and impaired carbohydrate metabolism [33]. The reasons for gender and age predisposition are determined by the anatomical and physiological characteristics of this group of patients. These are increased trauma to the thighs when they rub against the scrotum, the special composition and pH of sweat secreted by the apocrine glands of the genital area, the function of which is more pronounced in men [34].
RCS is characterized by pronounced polymorphism of clinical manifestations. Often the disease has a chronic course from the very beginning. The process involves not only large folds, but also the feet, hands, nails, buttocks, and legs [10, 35—37]. As a result of autoinoculation or primary infection, the axillary cavities, folds under the mammary glands in women, elbow bends and popliteal fossae, as well as any area of the skin, including the scalp, may be affected [38–40]. Generalized variants of rubrophytia have been reported in 16–25% of patients [41].
Lesions in RCS are often symmetrical, appear synchronously, and have irregular round or oval shapes. They are represented by inflammatory spots of pink or pink-red color, sometimes with a bluish tint. Inflammatory phenomena are most pronounced in the area of the peripheral ridge. Unlike epidermophytosis of large folds (ECF), it is not represented by vesicles, but by follicular focal small nodules of bluish-red color. The boundaries of the lesion are usually clear, intermittent, often with scalloped outlines. The lesions have peripheral growth, due to which they merge with each other. As a result, continuous large lesions with scalloped outlines are formed, covering large areas of the skin, including the thighs, buttocks, abdomen, pubis, genitals, back, and chest. In elderly people, the process, as a rule, extends beyond the folds and patients note severe and sometimes painful itching [1, 10, 42, 43]. It is no coincidence that RKS is called “eczema serpiginozum” [44]. Rarely, the lesions have an iris-like appearance due to two or more ridges running parallel to each other. Erythema with RCS is less pronounced than with ECS. There is also an isolated lesion of large folds without involving other areas of the skin in the process [45]. Sometimes deep follicular nodular infiltrates can be detected on the skin of the thighs, legs, and buttocks, and in a third of patients vellus hair is involved in the process [41]. A rare bullous type of RCS has been described [46]. MCS can occur atypically with simultaneous infection with Epidermophyton floccosum
and
Tr . rubrum
[47].
In some cases, the so-called unrecognized dermatophytosis ( Tinea incognito
) may develop - a local fungal infection of the skin, the clinical picture of which has changed due to the use of external corticosteroids. In this case, damage to the groin area, face, and back of the hands is more often noted. The infection spreads, and the clinical picture mimics another dermatological disease. The diagnosis is verified when the pathogen is detected [1, 46, 48].
Data on the frequency of lesions of the feet, hands, nail plates on the hands and feet, and other areas of the skin during RCS are rare in the literature and are based on a small volume of clinical observations, although the effectiveness of therapy directly depends on the sanitation of these lesions. Considering that Tr .
rubrum
has the ability to spread lymphogenously and affects vellus hair, it can be assumed that its course is more aggressive compared to ECS. In this regard, a comparative analysis of the occurrence of clinical manifestations in both forms of DCS on a large sample of patients can form the basis for the development of differential diagnostic criteria. To accomplish this task, we used data on the characteristics of the course of ECS presented in our earlier publications [12, 49].
Choosing a treatment strategy for MCS is not an easy task. Ointment-based preparations are rarely used, since the rashes are localized in areas with high humidity of the skin. MCS can be complicated by secondary infection and mycotic eczema, especially with concomitant diabetes mellitus. In this regard, mycosis proceeds torpidly and is more difficult to treat [50]. Therefore, when choosing treatment tactics, it is advisable to use topical single drugs that simultaneously have a pronounced antimycotic, antibacterial and anti-inflammatory effect. One such remedy is sertaconazole cream ( Zalain
) [51-56]. The high lipophilicity of the drug leads to its accumulation in the deep layers of the skin, ensuring that it maintains an effective therapeutic concentration of serum within 48 hours after application. Resistance of mycotic pathogens to the drug has not been registered. Relapses of the disease after a full course of treatment are practically absent. The drug does not have a systemic effect, does not cause side effects and is well tolerated by patients. The duration of its administration is determined individually depending on the characteristics of the clinical case, on average it is 2-4 weeks. Approved for use in children without age restrictions [51, 57].
On the other hand, the presence of exudative morphological elements, oozing (mycotic eczema) and maceration justifies the advisability of using anti-inflammatory drying therapy. For this purpose, it is advisable to choose water-based rather than alcohol-based drugs to avoid burning. Such a drug is povidone iodine solution ( Betadine
).
It has a wide spectrum of antimicrobial activity, causing the death of gram-negative and gram-positive bacteria, dermatophytes, yeast-like fungi of the genus Candida
spp
.
, lipophilic yeast of the genus
Malassezia
spp., pathogenic molds, viruses, protozoa. The drug does not have mechanisms for developing pathogen resistance. Available in the form of a solution (for acute processes) and ointment (for subacute and chronic processes).
The purpose of the study was to study the epidemiology of RCS in outpatients, features of the course of the disease, differential diagnosis with epidermophytosis based on a quantitative analysis of clinical manifestations, and to evaluate the effectiveness of treatment with the topical antimycotic (TA) sertaconazole ( Zalain
).
Mechanism of infection by rubromycosis
Infection occurs during contact with a sick person. But infection often occurs due to the use of common household items. To inoculate the pathogen of this disease, antibacterial drugs, as well as hormonal and cytostatic agents, are used.
It is known that disturbances in vascular tone, as well as changes in blood circulation in the extremities, which are so often observed in a variety of diseases, affect the contamination of fungal spores. It is certain that the disease does not affect the development of immunity. As for the incubation period of the disease, it has not yet been precisely established. In case of contact of the fungus with spores, long-term carriage develops, which is why a person who is not characterized by clinical manifestations of rubromycosis can become a carrier of the pathogen.
Causes of infection
Infection with rubromycosis occurs due to the influence of factors of exogenous and endogenous origin on the human body.
Exogenous causes that provoke the development of nail and foot fungus:
- Hyperhidrosis as a result of wearing shoes made of synthetic materials that do not allow air to pass through;
- Dry skin of the feet;
- Uncomfortable shoes that contribute to foot injury (formation of calluses, corns, inflammation);
- Lack of foot hygiene;
- Taking antibiotics and antihistamines in large courses;
- Wearing someone else's shoes;
- Use of general hygiene products;
- Failure to comply with personal hygiene rules in public places (swimming pool, sauna, bathhouse, locker rooms of sports institutions, beach and shower cabins).
Endogenous causes of rubromycosis of nails and feet:
- Hormonal imbalance;
- Low immunity;
- The presence of endocrine diseases (problems with the pancreas, diabetes mellitus);
- Diseases of the nervous system;
- Varicose veins of the lower extremities;
- Swelling of the legs;
- Blood diseases;
- Genetic dermatoses;
- Excess body weight;
- Immunodeficiency conditions (HIV, not HIV-related).
Causes of rubromycosis
Important!
Rubromycosis of the nails is transmitted only from person to person. If one family member is a carrier of the infection, there is a high risk of infecting the rest - both adults and children.
Symptoms of rubromycosis
Rubromycosis of the feet is usually diagnosed in more than 90% of cases of ailments that were caused by Tr. Rubrum. After the incubation period has passed, all interdigital areas are usually affected, followed by the skin of the soles.
In appearance, the skin that has been affected by rubromycosis is dry and infiltrated; diffuse hyperemia is also noted; the pattern on the skin becomes clearer. On the damaged area of the dermis, bright mucoid peeling is visible, which is more intense in the areas of the grooves. If rubromycosis is not treated, the disease spreads to the back and sides of the feet and toes. In children, exudation is observed on injured feet, which makes diagnosis difficult.
In case of chronicity, rubromycosis can affect the nail plate, disseminating to other places.
If we talk about rubromycosis of the hands, then it occurs through self-infection, less often - it is diagnosed initially. The clinic is the same as in the case of foot lesions, but not as intense due to frequent hand washing. Along the periphery of the lesions, you can notice an intermittent ridge that extends to the back of the hand.
As for rubromycosis of the nails, it is diagnosed when there are existing skin lesions. The latter is considered a separate disease that is very rare. Rubromycosis of nails involves damage to all nail plates at once. Yellow or white stripes appear on the side of the nail, which are visible through the nail.
In the case of the hypertrophic variant of nail rubromycosis, the nail itself is thickened and soon begins to break or crumble, hyperkeratosis (subungual) is also observed, not often, but yellow stripes are present. In the case of the atrophic form, the nail gradually becomes thin and collapses. The remains of such a nail remain near the nail fold, and sometimes the plate itself is separated from its bed.
Trichophyton rubrum - the causative agent of rubrophytosis
Trichophyton rubrum is an anthropophyll fungus. It only affects humans. The disease affects the feet, nails, hands and smooth skin. Hair is extremely rarely affected.
Characteristics of culture
Trichophyton rubrum grows slowly on a nutrient medium. Optimal growth temperature + 300C. Fungal colonies reach maturity after 14 days and are polymorphic: most often they are white and fluffy, with a cotton texture, less often they are leathery or mealy with areas of a purple, red-brown or yellow hue. As colonies age, they acquire a pink tint. After 3 - 4 weeks, a crimson or bright red pigment appears on their back side, diffusing into the nutrient medium. During the process of reproduction and growth, mushrooms create either flat or piled-up colonies and are grainy and fluffy.
Culture microscopy
The mycelium of red trichophytons is thin, microconidia (single-celled spores) are often pear-shaped, less often oval or rod-shaped, abundant, more common in granular strains. Blunt macroconidia are formed at the ends of the mycelial filaments. Chlamydospores can only be found in old crops.
Rice. 3. Pear-shaped microconidia (single-celled spores) Trichphyton rubrum They are located on hyphae, like birds on a wire.
Rice. 4. Trichophyton rubrum colonies: often white and fluffy, with a cotton texture (photo on the left), less often mealy, radially striated (photo on the right).
Rice. 5. The mushroom is named red because of its ability to deposit red pigment at the base of the colony when grown on Sabouraud’s nutrient medium.
Clinical manifestations of generalized rubromycosis
If we talk about the generalization of rubromycosis, then it occurs only after the prolonged existence of limited forms. Diseases associated with internal organs, nervous and endocrine systems, changes in the skin are considered the main cause of generalization of rubromycosis. The reasons also include the side effects of various medications, including antibiotics, cytostatics and hormones. The lack of appropriate treatment for forms of the disease is also considered the cause of the disease.
If we talk about the erythematous-squamous form of rubromycosis, then it is concentrated in various parts of the dermis, accompanied by characteristic itching and disguised as another disease. Only a doctor can distinguish this form from atopic dermatitis, atypical eczema and parapsoriasis.
You can confirm the mycotic nature by examining the damaged area. It is known that lesions are located in groups; they often form rings, arcs and even garlands. In the case of hyperpigmentation or peeling (localized from the center to the periphery), the skin change is mycotic in nature. The edges of a scalloped nature with existing edematous intermittent ridges are considered signs of rubromycosis. Typically, the disease has an undulating course with further exacerbations that occur during the warm season.
The follicular nodular form of rubromycosis affects the feet, hands, legs, forearms and buttocks. Rubromycosis particles tend to grow peripherally and also to coalesce. Such elements are characterized by similarities with vasculitis nodosum and erythema nodosum. If the skin of the face is involved in the process, the clinical manifestations are very similar to the manifestations of lupus erythematosus.
Rubromycosis can affect the intergluteal folds, the dermis located under the mammary glands, and people who are overweight often suffer from excessive sweating. The lesions are considered infiltrated. Often their surface has a yellowish-red color (or brown), peeling is visible, which is characterized by a transition from the center closer to the periphery.
Due to the presence of an intermittent scalloped ridge that has crusts and papules, rubromycosis can be distinguished from a number of diseases, for example, from microbial eczema and candidal infection. It is very important to identify the absence of maceration during diagnosis. The latter is inherent in candidiasis. And the absence of polymorphism will allow us to say for sure that a person does not have eczema.
Material and methods
The work was carried out at the Department of Skin and Sexually Transmitted Diseases with cosmetology at the Medical Institute for Advanced Training of Physicians of the Moscow State University of Food Production, as part of the departmental research work “Infectious and parasitic skin diseases”. It is based on data from a multicenter study “Study of real practice in the treatment of patients with dermatomycosis in the Russian Federation,” conducted in 2012-2013. under the patronage of the pharmaceutical industry (Hungary) simultaneously in 50 regions of the Russian Federation. 97 medical and preventive institutions of various profiles, 174 doctors are involved. The number of doctors participating in the study depended on the size of the city population and ranged from 1 to 24 specialists, and the number of completed questionnaires in the city ranged from 10 to 644. To unify the research, the author’s version of the questionnaire was developed, including 27 points. Instructions for filling out the questionnaire were presented in the form of a presentation, in which the rules for filling out each item of the questionnaire were explained to doctors and photographs of clinical cases were provided.
In total, doctors filled out 5025 questionnaires for patients with MVP. The diagnosis of mycosis was confirmed bacterioscopically. More than half of the sample ( n
=2784, 55.4%) were patients with dermatophytosis (B-35).
In their structure, MS was in the lead ( n
=995, or 35.7%), 2nd place was occupied by DKS (
n
=735, 26.4%).
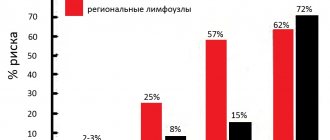
There were 870 (17.3%) patients with MCS, taking into account candidiasis of this localization, including 735 (84.5%) DCS. In the structure of the latter, ECS ( n
=615, or 83.7%) prevailed over RCS (
n
=129, or 16.7%) by 5.1 times.
Statistical processing of 70 (58.3%) well-filled questionnaires for patients with RCS was carried out. The sample was representative to obtain statistically significant data. Statistical processing of the results was carried out using the statistical software package Statistica 6.0. The method of correlation analysis (Spearman coefficient) and t
-test were used.
The level of statistical significance corresponded to 95% ( p
<0.05).
The criteria for including patients in the study were developed: patients with RCS, including those with ineffective previous treatment; in the presence of concomitant MS, including damage to the nail plates with a KIOTOS index of 1-2; superficial form of OM, distal form with lesions up to 1/3 of the depth of the nail in the absence or moderate hyperkeratosis, as well as distal form with lesions up to 1/3 of the depth of the nail with pronounced hyperkeratosis, but with involvement of the II-V nail plates in the process.
For uncomplicated RCS, including concomitant MS, sertaconazole ( Zalain
) rubbed 2 times a day (morning and evening).
Treatment of the complicated process was carried out according to a single scheme. In the presence of exudative manifestations (vesicles, blisters, pustules, erosions, oozing, maceration), they were extinguished with Betadine
.
Drying of the exudate of the cavity elements in the lesion into crusts usually occurred within 3-5 days. Zalain
was used at night .
Allergic dermatitis, as a rule, resolved within 5-7 days. In the presence of mycotic eczema, treatment was carried out in stages: shading and/or lotions with Betadine
, then rubbing in travocort (in the morning) and sertaconazole (
Zalaina
) (at night) until the crusts disappeared.
After the complications were relieved, treatment with sertaconazole ( Zalain
) was continued 2 times a day.
When mycosis was complicated by secondary pyoderma, a solution was used (in the presence of pustules and erosions) and Betadine
(until the crusts came off) in the morning, and sertaconazole (
Zalain
) in the evening. If mycoallergens were present outside the folds and feet, they were treated with a combined topical corticosteroid (Travocort). General treatment was indicated for patients with mycotic eczema, allergic dermatitis, and mycoallergides. Antihistamines (suprastinex, parlazin) were prescribed orally for 7-10 days.
In the presence of OM, doctors were required to recommend that patients carefully cut off the grown part of the nail once a week, file off its shiny layer and polish nails with hyperkeratosis, as well as explain methods of disinfecting shoes and tactics for its implementation. The effectiveness of therapy was monitored after 2, 3 and 4 weeks according to the following criteria: recovery, significant improvement, improvement. Recovery was considered to be the resolution of all clinical manifestations of RCS, MS and OM in the patient; significant improvement - reduction in the area of lesions, predominance of erythema in the clinical picture of the disease, disappearance of papules, vesicles, epithelization of erosions, reduction of pathological changes in the nail plate; improvement - preservation of the area of lesions with positive dynamics of resolution of rashes.
Diagnosis of rubromycosis
Although rubromycosis in its clinical manifestations is often similar to various skin diseases, the main symptoms are specific, so even with a careful examination, the doctor can make an accurate diagnosis. In order to confirm the diagnosis, a cytological examination of the taken pathological material is usually carried out. To detect the exact pathogen, culture and other examinations are performed to help determine the sensitivity of the disease to various medications. Speaking of differential diagnosis, it is carried out with microbial eczema, psoriasis and skin tuberculosis. If the lesion has affected the skin of the face, then it is necessary to differentiate the disease from lupus erythematosus.
Preventive actions
Prevention of rubromycosis consists of following simple tips:
- maintaining foot hygiene;
- refusal of uncomfortable shoes made of synthetic materials;
- mandatory use of personal belongings and shoes;
- regular disinfection of shoes;
- wearing socks and stockings made from natural fibers;
- refusal to walk barefoot in public places, on the beach;
- taking antibiotics only as prescribed by a doctor.
A strong immune system reduces the risk of infection with trichophytons. By paying attention to your health, you can forever forget about relapses of the disease.
Treatment
When prescribing a course of treatment, not only the dynamics of the course of rubromycosis, but also the presence of concomitant diseases are taken into account. Treatment of rubromycosis is carried out after eliminating inflammation, suppuration, removing swelling, and freeing the affected area from keratinized epithelium. In case of squamous leaks, rubromycosis is immediately treated.
Groups of medications to eliminate associated symptoms:
- relieving inflammation - non-steroidal anti-inflammatory drugs;
- removal of swelling - antihistamines;
- exfoliation of keratinized epithelium – keratolytics;
- inhibition of reactive inflammatory processes - glucocorticosteroids or cortisones.
If the inner skin layer (endoderm) is not affected, gels and ointments based on terbinafine and oxyconazole are sufficient. Course duration is 3-6 months. If the effectiveness of external agents is insufficient - fluconazole, mycosolone. If the nails are affected, fungicidal varnishes are used, and a scraper is used to remove the keratinized epithelium. With rubromycosis of smooth skin, softening and exfoliation of dead epithelium is not required.
Important!
When viral, bacterial and immune diseases occur simultaneously, the interaction of medications with antifungal drugs should be taken into account. The simultaneous use of penicillins, cephalosporins and antifungal drugs reduces the effectiveness of each other. With tetracyclines and aminoglycosides – mutual enhancement. Do not combine medications at home. Only the attending physician can calculate the concentration of both drugs and adjust the course of treatment without increasing the toxic load on the liver and kidneys.
Features of therapeutic therapy in childhood
In children, discomfort (itching, burning) can significantly affect mental development. When treating a child, along with the main drug, it is also necessary to take medications to eliminate discomfort. When treating adults, this is a secondary aspect.
Other features:
- due to the presence of contraindications to most effective drugs, several analogues of one drug are used, for example, a glucocorticosteroid is replaced with an antihistamine and an immunomodulator;
- doctors try to avoid the simultaneous prescription of antifungal drugs and medications that enhance or slow down the effect of it;
- Tablets and capsules are replaced with suspensions;
- The course dosage is calculated based on body weight, and not the number of units of this release form.
Due to the child’s accelerated metabolism, the course of treatment is several times shorter. Chronic cases are rare in children.