Free consultation with a doctor by phone
Surgeon appointments are available daily by appointment!!!
LLC "Your Doctor"
Chat with the doctor
Addresses of medical centers in Moscow (unified reference) +7 (495) 255-45-59
Make an appointment at the clinic Discount on services Promotions
- +7 (495) 255-45-59
- Surgical centers in Moscow
- Every day from 9.00 to 20.00
- call me back
You can make an appointment with our operators by calling +7 (495) 255-45-59
Prices for services Clinic address Make an appointment Call a surgeon to your home Pediatric surgeon Ligation
A fibrous benign neoplasm, which occurs as a result of the closure of the outer lumen of the ducts of the sebaceous glands, is an atheroma on the penis. It looks like a round capsule of a yellowish color, it has clear boundaries. With atheroma on the penis, men experience complexes due to the unaesthetic appearance of the penis and psychological discomfort. Atheroma on the penis is not transmitted through sexual contact.
At the initial stage, atheroma is small in size and its growth takes quite a long time. If you ignore the presence and development of atheroma, the results can be disastrous. Atheroma on the penis can only be treated surgically or using a laser. It is advisable to remove it when the size of the atheroma is still small.
Useful information on the topic:
- Treatment of atheroma
- Ear atheroma
- Atheroma on the head
- Atheroma on the face
- Atheroma on the back
- Inflammation of atheroma
- Atheroma of the eyelids
- Purulent atheroma
- Breast atheroma
- Laser removal of atheroma
- Removal of atheroma at home
- Atheroma on the neck
- Atheroma on the lips
- Atheroma on the leg
- Atheroma in the groin
- Atheroma on the labia
Causes of white plaque
The causes of white plaque on the penis are classified into three groups:
- physiological. Associated with the peculiarities of the secretion of tyson glands located under the foreskin. The problem is aggravated by the lack of proper hygienic care of the genitals;
- non-infectious (endogenous). Caused by disruption of internal organs. Whitish accumulations on the penis are a concomitant symptom of chronic diseases or a sign of activation of opportunistic microorganisms that are part of the natural microflora of the body;
- infectious (exogenous). These are sexually transmitted diseases (STDs).
In the first case, it is enough for a man to get medical advice. To eliminate other causes, proper treatment is required.
PRE-CANCEROR FORMATIONS
Extramammary Paget's disease
Extramammary Paget's disease is clinically characterized by erythematous plaques with oozing, ulcerated, and scaly nodules and focal hyperpigmentation. Areas of hypopigmentation can also be seen (Fig. 6a). Dermoscopy of extramammary Paget's disease reveals milky red areas, vascular structures, superficial scales, ulcers, pigment network, shiny white lines and white structureless areas [Fig. 6b]. Common vascular structures are stippled vessels and glomerular vessels [22]. Paget's disease is often mistaken for melanoma due to features such as irregular pigmented globules, white negative pigment network, and structureless blue-gray areas [23].
Erythroplasia Keira
It is the genital counterpart of Bowen's disease and has similar dermoscopic features. Glomeruloid vessels are characteristic, located in clusters or diffusely, which can be used to differentiate Queyre's erythroplasia from other causes of chronic balanitis. In addition, linear vessels and brown dots can be seen [24]. Dermoscopic features in pigmented Bowen's disease include pigmented streaks combined with other features such as comedo-like structures [25].
Vulvar intraepithelial neoplasia
This is a common cause of genital itching. About 15% of vulvar intraepithelial neoplasias are pigmented. Typical findings are milky white or pink areas associated with punctate or glomerular vessels and papillomatous structures. In the pigmented version, brownish dots with clearly defined boundaries and brain-like structures are visible [26].
White coating on the penis: when is this normal?
Why might a white coating on the penis be normal? Due to the increased production of a special male secretion - smegma. It is produced by tyson (preputial) glands under the foreskin - a type of exocrine sebaceous glands. Smegma facilitates the sliding of the foreskin when exposing the head of the penis. The secretion mixes with exfoliated epithelial cells, forming a white coating on the head of the penis. The problem is more common in men who have not undergone circumcision. Increased secretion of the preputial glands does not require special treatment. But if the rules of hygiene of the genital organs are not followed, it can lead to inflammation (balanitis, balanoposthitis) and oncopathology.
BENIGN LOCATIONS
Seborrheic keratosis
Pigmented seborrheic keratosis, like its cutaneous counterpart, shows features such as polypoid structures, marrow-like structures, and finger-like structures on dermoscopy. Comedo-like structures, which are keratin-filled invaginations, are not observed in genital seborrheic keratosis due to constant friction. Milium-like cysts are usually visible because they are located intraepidermally [11,19].
Verruciform xanthoma
These are rare tumors composed of lipid macrophages that present clinically as yellowish plaques and nodules with a papillomatous surface in the anogenital areas. Dermoscopy reveals numerous yellowish papules with centrally located spiny vessels [20,21].
White plaque on the penis: possible diseases
White plaque on the penis accompanies balanitis, provoked by an exacerbation of psoriasis. Skin pathology has no clear cause and is considered irreversible. When relapsed, psoriatic plaques can affect the genitals, causing inflammation.
White plaque on the penis and itching of the genitals are not uncommon with diabetes. The disease is characterized by metabolic disorders, failure of the production of the hormone insulin or insulin resistance. A diabetic's urine contains glucose, which irritates the head of the penis when urinating. As a result, balanoposthitis develops.
Curdled discharge on the penis occurs due to candidiasis (thrush) of non-infectious origin - increased activity of fungi of the genus Candida. Disturbance of microflora balance occurs against the background of:
- weakened immune status;
- prolonged psycho-emotional overload;
- incorrect antibiotic therapy;
- intoxication (including alcohol);
- systematic contact of the genitals with synthetic fabrics;
- unbalanced diet;
- failure of metabolic processes.
Candidiasis is transmitted sexually if a woman has progressive thrush.
A separate category consists of sexually transmitted diseases. Infection occurs through unprotected intimate contact with an infected partner. Redness of the penis and a white coating are among the symptoms of most sexually transmitted infections.
STDs and pathogens
| bacteria | |
| syphilis | treponema pallidum |
| gardnerellosis (in men) | gardnerella |
| gonorrhea | gonococci |
| ureplasmosis | ureplasma |
| viruses | |
| papillomatosis | human papillomavirus |
| cytomegalovirus infection (CMVI) | cytomegalovirus |
| genital herpes | herpes virus type 2 |
| prokaryotes | |
| mycoplasmosis | mycoplasma |
| protozoan parasites | |
| chlamydia | chlamydia |
| trichomoniasis | trichomonas |
NORMAL PHYSIOLOGICAL CONDITIONS OF THE GENITAL ORGANS
Vestibular papillomatosis
It is believed to be an anatomical variant of the vestibular mucosa, but the condition is often confused with genital warts, leading to unnecessary interventions. This is the female equivalent of pearly penile papules. Clinically, this manifests itself on the inner side of the labia minora in the form of thread-like projections. When dermatoscopy, it appears in the form of transparent papillae with a pronounced fibrovascular center containing randomly located vessels (Fig. 2a). The bases of individual papillae remain isolated. Dermoscopy of genital warts demonstrates multiple, randomly arranged papillae with tapering ends that are less transparent and wider than the structures found in vestibular papillomatosis [Figure 2b]. The papillae arise from a common base [6]. Hemorrhagic lesions in the form of black and red dots and stripes are also visible [7].
Pearly penile papules
They are benign physiological formations located in the area of the coronary sulcus. They are also mistaken for genital warts. On dermatoscopy, they appear as white, slightly translucent papillae arranged in a cobblestone pattern, with a central vascular component that is comma-shaped or may appear as a dot [Figure 3] [8].
Hyperplasia of the sebaceous glands
Modified sebaceous glands located above and distal to the prepuce are called Tyson's glands. Hyperplasia of the sebaceous glands or ectopic sebaceous glands are usually observed in the red border of the lips. On the genitals they appear as pink-yellowish, tiny papules with an umbilical depression. On dermoscopy, they appear as distinct yellowish structures with milky white ovoid structures that are slightly translucent [Figure 4]. They are surrounded by non-branching vessels. Similar lesions can be observed in the mucocutaneous fold of the labia minora in women [9].
Pigment formations
Pigmented formations located on the mucous membrane of the genital organs are observed in approximately 10% of women with fair skin. In men, these formations are located on the head of the penis, and in women in the vulva area. This includes melanotic macules or lentiginosis, nevi, melanoma, angiokeratomas, seborrheic keratosis, squamous cell carcinoma and basal cell carcinoma (BCC) [10].
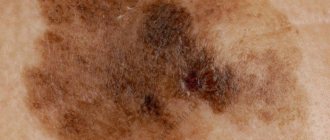
Melanosis
Melanotic macules, or melanosis, are the most common pigmented lesions observed in the genital mucosa. It is believed that this is a violation of the migration of melanocytes into the epidermis [11]. They tend to appear in areas of the mucosa with non-keratinizing epithelium, rather than in areas of the external genitalia with areas of hair growth. They are benign pigmented macules that are characterized histopathologically by increased pigmentation of the basal layer. It usually appears in people with skin phototypes IV, V and VI. They are clinically present as single or multiple macules ranging in color from light brown to black and can range in size from 1 mm to 1 cm [Figure 5a]. They can often be mistaken for mucosal melanoma. However, standard algorithms such as ABCDE—asymmetry, margin, color, diameter, evolution—may not be suitable for the assessment of genital pigmented macules [10]. The various dermoscopic patterns are described as follows:
1. Ring-like pattern: multiple ovoid structures with hyperpigmented borders, which in some areas look like bunches of grapes [12].
2. Parallel structures: This can be seen in the typical small spots located on the lips, glans penis and vulva. The pigment bands are arranged in regular parallel lines [Figure 5b].
3. Structureless Areas: Structureless pigmented areas ranging in color from light brown to dark blue-gray. Clinically, these macules have a slightly larger diameter [13].
4. Reticular pattern: Similar to the reticular component of pigmented nevi located on the skin, where the pigment appears as a round to ovoid reticular component [Figure 5c].
5. Globular pattern: round-ovoid dark brown globular structures [14, 15].
Genital nevi
They are even more rare, with the prevalence of vulvar nevi being 2.3% among cases of melanocytic nevi [13]. A variety of vulvar nevi are atypical melanocytic nevi of the genital type (AMNGT), which have specific histopathological features. Vulvar nevi are usually present in childhood, in contrast to AMNHT, which is observed in women of the reproductive age group. Vulvar nevi are flat or dome-shaped papules that are pink to dark brown-black or blue in color. They have regular borders and are evenly pigmented. The most commonly described dermoscopy patterns are globular and homogeneous patterns. In addition, milia-like cysts can also be seen. Other patterns, such as parallel structures and cobblestone patterns, are also found and are sometimes difficult to distinguish from vulvar melanosis, which exhibits similar patterns. Sometimes a mixed pattern and radial radiation may raise suspicion for melanoma, and then histopathology can solve this problem [10, 13]. “Divided” or “kissing nevus” of the penis, which are a type of congenital melanocytic nevus, have also been described. It is a solitary nevus that initially divides after the epidermis invaginates to form the coronal sulcus. Dermoscopic features similar to those of congenital melanocytic nevi on the skin, in particular dots and globules, have been described [16]. In a study on genital melanocytic nevi, the authors found that most dermoscopic features were similar to melanocytic nevi on the skin. However, in some cases, differentiation between melanosis and melanocytic nevi, as well as between benign and malignant melanocytic tumors, was not possible using dermatoscopy alone [11]. The practice of routine prophylactic biopsy of melanocytic nevi should be abandoned, especially in children, in the absence of any alarming signs, both clinical and dermoscopic [17].
Atypical melanocytic nevi of the genital type
They make up 5% of all benign melanocytic formations of the genitals. The main histopathological features are as follows [18]:
1. Nested pattern: round or ovoid nests of melanocytes of various sizes that are oriented perpendicular or parallel to the dermoepidermal border.
2. Dyshesive nest pattern: adjacent scattered melanocytic nests, represented by epidermal and dermal melanocytes.
3. Crowded pattern: closely spaced, ill-defined nests of melanocytes located at the dermoepidermal border.
A mixed model of structure is most often observed during dermatoscopy. Parallel lines appear along with structureless areas or brown-black globules [14, 15]. A blue-white veil and irregular dots have also been described. All cases with a mixed pattern on dermoscopy should undergo biopsy to rule out melanoma [10].
Diagnosis and treatment
Treatment of diseases of the male reproductive system, including treatment of STDs, is the responsibility of urologists and andrologists. In case of an infectious lesion, therapy is prescribed by a venereologist. The cause of plaque on the penis is diagnosed based on the results:
- visual medical examination;
- studying the patient's premorbid background;
- laboratory tests: OCA and blood biochemistry, urethral smear, urine test;
- ultrasound examination of the pelvic organs.
Based on the results of the examination, the doctor chooses treatment tactics, determines medications, dosage and duration of the therapeutic course. For bacterial, prokaryotic, and parasitic infections, antibiotics are prescribed. Candidiasis is treated with antimycotics in tablets and ointments. For diabetes and psoriasis, basic treatment and diet therapy are adjusted.
Preventive measures help prevent unpleasant manifestations - careful genital hygiene, barrier contraception, strengthening the immune system and following the recommendations of the attending physician (for chronic diseases).
An important point is a timely visit to a urologist, both in the event of symptomatic complaints and for prevention. Make an appointment
Main methods of treatment
If a cyst of any color or size is detected, you should contact a specialist. A urologist-andrologist will determine the cause of the disorder and draw up a treatment plan. There are three main methods:
- surgical excision;
- laser or radio wave removal;
- cryodestruction.
The appropriate method is selected individually. The choice depends on the type of neoplasm, concomitant and previous diseases. Cyst removal is performed on an outpatient basis using local anesthetics. You must first make an appointment with a urologist.
To get an appointment with a doctor, call the reception desk. We will select a time convenient for you. The prices for the clinic’s services can be found in the price list.
VASCULAR FORMATIONS
Angiokeratoma
Angiokeratoma of Fordyce manifests as multiple, well-defined, bluish-black papules on the skin of the scrotum [Figure 7a]. They are often clinically mistaken for genital nevus, blue nevus and melanoma. Various sources indicate that 20% of angiokeratomas were misdiagnosed as melanoma [32]. Dermoscopy clearly shows pronounced reddish-dark blue lacunae with a blue-white veil [Figure 7B] [33].
Lymphangiectasia of the vulva
Acquired lymphedema and lymphangiectasia of the vulva usually occur due to damage to the lymph nodes that occur after trauma, infection, malignancy, surgery, radiation, etc. Clinically, they present as flesh-colored papules or transparent vesicles with a diffuse erythematous background. Piercing the lesion may release clear fluid. Dermoscopy reveals clearly defined, round-oval reddish lacunae with whitish septa and numerous small pinpoint lacunae. This is similar to the manifestations of lymphangioma. Dermatoscopy is relevant when lesions are sometimes confused with warts or molluscum contagiosum [34].
CONCLUSIONS
Dermatoscopy has become important in the diagnosis of non-pigmented dermatoses and for differentiating benign lesions from equivocal and malignant lesions [1, 28]. Many dermatologists in modern practice have included dermatoscopy in their routine work. Although this does not eliminate the need for biopsy, the technique avoids unnecessary biopsies of benign lesions. It also helps us carefully select the biopsy site for suspicious or atypical pigmented lesions.
INFLAMMATORY DISEASES
Balanitis Zuna
In this condition, well-defined reddish plaques are visible on the skin of the glans or the inner side of the foreskin [Figure 8a]. Dermoscopy reveals uniform reddish-orange areas with curved vessels [Figure 8b] [24]. The orange areas correspond to hemosiderin deposition, and the curved vessels represent vascular proliferation. Other types of vascular structures include crescentic vessels and convoluted, cupped, linear and stippled vessels [35].
Candidal balanitis
Candida balanitis is characterized by curdled-like structures, which are colonies of fungi, as well as linear vessels [24].
Psoriatic balanitis
Clinically, multiple erythematous papules and plaques are detected. Dermoscopy reveals uniformly distributed, dilated and dotted vessels on an erythematous background [36].
Lichen planus
Thick, linear and irregular hairpin-shaped vessels are distributed diffusely according to the localization of lichen planus plaques. The Wickham grid is clearly visible against an intense red background [5].
Lichen sclerosus
White, ivory-colored atrophic plaques are visible on the skin of the glans and labia minora, disrupting the normal architecture of the skin of the anogenital area [Figure 9a]. Dermoscopy reveals white structures that appear pinkish, consistent with sclerosis on histopathology [36]. The gray-blue dots are arranged in a pattern of scattered pepper, which corresponds to melanophages of the skin. Characteristic features are a marked decrease in the number of vessels and the presence of polymorphic vascular patterns [Figure 9b] [5]. Purple-red globules and spots are visible especially in women, consistent with blood stains due to excessive scratching.
MALIGNANT EDUCATIONS
Melanoma
Vulvar melanomas account for 1-3% of all melanomas observed in women. They are often found in older women and present as flat or raised pigmented lesions that are often larger than 7 mm in size. Non-pigmented variants have also been described. Multiple colors and a multicomponent structure pattern characterize the dermoscopic picture of mucosal melanoma [11, 27]. The presence of blue, gray and white colors with or without structureless areas had 100% sensitivity for diagnosing melanoma [28]. Reticular depigmentation and a network of fine whitish lines are valuable in the diagnosis of early vulvar melanoma [10]. In non-pigmented melanoma, dermoscopy reveals whitish, skin-colored papules with polymorphic vessels [29]. Asymmetry, multicomponent patterns, blue-white veil, and the presence of vessels should raise suspicion of malignancy and be confirmed by histopathology [30].
Basal cell carcinoma
Dermoscopy of genital BCC is similar to cutaneous BCC, consisting of bluish-gray ovoid globules, whitish homogeneous areas, and tree-like vessels. Non-pigmented lesions are difficult to diagnose because... they can mimic inflammatory diseases. In this case, clearly visible tree-like vessels help make the diagnosis [31].