The penis, or penis, is an organ of the male genitourinary system. It performs a double function: the urethra passes through the thickness of the penis, through which urine and sperm are excreted. Anatomically, the penis has the following parts:
- The body, which starts from the trunk and passes from the front to the head.
- The glans is the terminal part of the penis, covered with thin, sensitive skin.
- The foreskin is a fold of skin that runs transversely in a circle and protects the head.
- The frenulum is a fold of skin that runs from below the head in the longitudinal direction and connects it to the skin.
Inside the penis there are two cavernous bodies - during sexual intercourse they fill with blood and provide an erection - and one spongy body - the urethra passes through it.
Is there such a thing as penile cancer? Penile cancer refers to malignant tumors that develop from the skin that covers it. They are rare. According to American and European statistics, penile cancer is diagnosed in one in 100,000 men every year, accounting for 1% of all cancers in men.
Causes and risk factors for penile cancer
The exact causes of penis cancer are unknown, but doctors and scientists know about some risk factors:
- Human papillomavirus. The pathogen is sexually transmitted and many people are currently infected. There are more than a hundred types of HPV. Only a few of them are dangerous. In women, they increase the risk of cancer of the vagina and cervix, in men - the risk of penile cancer (viruses of types 16 and 18 are found in patients).
- Promiscuous sexual intercourse. Apparently, this factor is directly related to human papillomavirus infection. Research shows that men who have had two or more sexual partners before the age of 20 have a 4-5 times increased risk.
- Age. The disease mainly occurs in men over 50. Before the age of 40, penile cancer is extremely unlikely to develop.
- Smoking . Tobacco smoke contains carcinogens that penetrate into the blood and can cause mutations in the DNA of cells in any organ. In addition, smokers have worse local defense mechanisms, so they are more likely to become infected with HPV.
- Immunodeficiency states. The immune system destroys not only pathogenic viruses and bacteria, but also defective ones, including cancer cells. If the immune system does not work well, the risk of any cancer increases.
- Phimosis . This is a condition in which the foreskin narrows and prevents the head of the penis from being exposed. According to statistics, men with phimosis are more often diagnosed with penile cancer.
If a man has any risk factors from this list, this does not mean that he will necessarily develop a malignant tumor. At the same time, sometimes the disease is diagnosed in men who do not have any risk factors.
Introduction
Precancerous dermatoses of the male genital organs are often encountered in routine dermatological practice.
It is often difficult to distinguish these precancerous lesions from benign genital dermatoses. The tendency for delayed presentation, often with a history of prolonged self-medication or treatment failure, can lead to progression to invasive carcinoma requiring major surgery (1).
This affects not only a person’s physical well-being, but also their psychological health and quality of life. Therefore, early diagnosis and treatment before deep invasion is very important for effective conservative treatment, which avoids the need for partial or complete amputation of the penis.
The rarity of these diseases has meant that our knowledge is based on few retrospective studies. This review outlines the common features of precancerous penile lesions.
Etiology and classification
Several risk factors are associated with the development of genital malignancies. These include the presence of foreskin, phimosis, poor hygiene, smoking, chronic inflammation and having multiple sexual partners.
Infection with the human papillomavirus (HPV) is one of the most important risk factors for developing penile cancer.
Precancerous lesions of the penis can be divided into:
1. Those associated with HPV infection
2. Those that are not associated with HPV, but are caused by chronic inflammation.
HPV-associated lesions include Bowen's disease (BD), Queyre's erythroplasia (EC), and bowenoid papulosis (BP), which are associated with “high-risk” HPV types 16 and 18. Low-risk HPV types 6 and 11 are associated with other precancerous lesions such as giant condylomata acuminata (GCA) or Buschke-Lowenstein tumors.
Non-HPV lesions are primarily associated with penile lichen sclerosus (LS). However, they are also associated with rarer chronic inflammatory conditions such as penile cutaneous horn, leukoplakia, porokeratosis, extramammary Paget's disease, and pseudoepitheliomatous and keratotic mica balanitis (PKMB).
The risks of progression of various precancerous conditions to malignant lesions are given in the table [Table. 12).
Pathogenesis
Although penile cancer accounts for only 1% of malignancies diagnosed in men in the United States, the rate is significantly higher in parts of Asia, South America, and Africa, where it approaches 10% (3).
Precancerous lesions account for approximately 10% of all penile malignancies at initial presentation, with the vast majority located on the glans. The risk of malignant transformation has been reported to be as high as 30% if left untreated.
Squamoproliferative dysregulation caused by human papillomavirus
A recent systematic review of existing polymerase chain reaction techniques identified the influence of HPV DNA in approximately 50% of cases of penile squamous cell carcinoma (PeSCC) (4).
In this regard, penile tumors appear to share pathogenesis and histology with vulvar carcinomas and other HPV-associated, low-grade SCCs ( 5 ).
“High risk” HPV types 16 and 18 are found in 60-75% of invasive tumors in situ. HPV exerts its tumorigenic effects through the expression of two viral genes, E6 and E7, which are continuously expressed in cells infected with high-risk HPV types.
The interaction products of the E6 and E7 genes impair cell differentiation, proliferation, and apoptosis through their involvement in the retinoblastoma Rb/E2F and P53 tumor suppressor pathways. Of course, their expression is required for the induction and maintenance of the neoplastic phenotype of cells in cervical cancer, and similar mechanisms appear to exist in penile cancer.
Human papillomavirus-independent squamoproliferative dysregulation
Chronic inflammation occurred in half of newly diagnosed penile cancer cases (6).
Unlike HPV-associated tumors, progression of these precancerous lesions to keratinizing/verrucous PeScc is possible (7).
Associated intraepithelial neoplasia is usually highly differentiated and may have a more predictable course compared with thick dysplastic lesions. The mechanism of HPV-independent carcinogenesis is still not fully understood.
Lesions associated with human papillomavirus
Keir's erythroplasia, Bowen's disease of the penis and Bowenoid papulosis
EC, BD penile (BDP), and PD are three clinical variants of carcinoma in situ (CIS) of the penis (8).
Smegma, poor hygiene, immunosuppressive condition, trauma, site friction, etc. are risk factors. The exact etiology of EC, BDP and PD is still unclear.
However, it has been suggested that PD is probably a virus-induced epithelial dysplasia associated primarily with HPV 16 and 18.
Patients usually complain of itching, pain, bleeding and difficulty retracting the foreskin. Penile BD consists of red, shiny, slightly pigmented patches or plaques of keratinized penile epithelium, while EC affects the genital mucosa.
The term “PD” should be used to describe multiple warty lesions that are often pigmented in keratinized areas and more numerous and more inflamed in “mucous” areas.
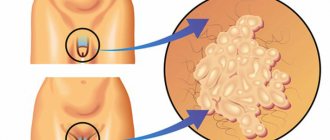
PD lesions are less papillomatous, smoother in surface, more polymorphic, and more clustered than common genital viral condylomata, and occur in younger, sexually active men, in contrast to the macular or scaly plaques of EC and BDP, respectively, seen in older men. [rice. 1] and [fig. 2].
The differential diagnosis of EC and BDP includes psoriasis, LS, erosive lichen planus, ZB, and extramammary Paget's disease. Differential diagnosis of PD includes lichen planus, common warts, seborrheic warts, nevi and condylomas.
A biopsy is indicated in cases where the clinical diagnosis is unclear. Occasionally, a repeat biopsy may be required if initial histology is inconclusive.
On histological examination, EC and BDP show SCC in situ, that is, atypical squamous cells proliferate throughout the thickness of the epidermis and do not penetrate the dermis. PD may also demonstrate scattered atypical cells or thick atypia.
The risk of progression to invasive cancer is thought to be higher for EC (approximately 30%) than for BDP (9). The risk of progression of PD to invasive squamous cell carcinoma is very low (2.6%) unless an immunocompromised condition exists.
This may also be due to the fact that most cases of PD are treated like warts with destructive therapy, so the exact number of cases is unknown.
Patients with these conditions should be counseled and tested for HPV and other sexually transmitted diseases, including HIV infection. You should be advised to quit smoking. Sexual partners should be advised to seek testing.
Long-term follow-up is necessary and this should be explained to the patient.
Treatments include topical 5-fluorouracil (5-FU) 5% cream, topical imiquimod, cryosurgery, curettage and electrocautery, excisional surgery, Mohs micrographic surgery, laser and photodynamic therapy (PDT).
Circumcision removes a major risk factor for malignancy and provides sufficient tissue for histological examination.
Giant condyloma accuminatum (Buschke-Levenshtein tumor)
Giant condyloma, also known as Buschke-Loewenstein tumor, is a large, warty, exophytic, cauliflower-like growth that is an HPV-associated lesion that affects any part of the anogenital area.
On the penis, lesions are found around the coronary sulcus, frenulum, penile shaft, and sometimes in the anterior urethra. Spread to the posterior urethra and bladder is usually seen only in immunocompromised patients.
Risk factors include immunosuppression, chronic irritation, presence of foreskin and poor hygiene.
Organ transplantation and chronic hidradenitis suppurativa are also predisposing factors (6). They are caused by infection with low-risk HPV types 6 and 11.
Both sexes can be affected. These lesions usually occur in sexually active men in the third decade of life.
In cases of suspected carcinoma, a deep surgical biopsy is required. Histopathological examination shows hyperplastic epithelium, parakeratosis in the stratum corneum, atypia, and focal small islands of atypical squamous epithelium.
Surgical excision is the method of choice (glansectomy or penectomy). Mohs micrographic surgery, cryotherapy, laser treatment, interferon-α, radiation therapy or bleomycin, systemic retinoids are alternative methods.
Radiation therapy should be avoided as it may accelerate transformation to anaplastic carcinoma. The prognosis is poor because the tumor may continue to grow and deepen locally. The cause of death was hemorrhage from femoral artery invasion or cachexia.
Even with treatment, relapses and progressive malignant transformation occur, so observation is necessary.
Lesions associated with other types of papillomavirus
Lichen sclerosus localized to the genitals in men
The male variant of LS is a chronic, progressive inflammatory dermatosis of unknown etiology affecting the glans penis, foreskin, anterior urethra, and meatus (10).
It is also called end-stage balanitis obliterans sclerosis. It occurs almost exclusively in uncircumcised men (11).
Its exact etiology remains unclear, although an autoimmune component or even a genetic predisposition based on human leukocyte antigens has been suggested. Thus, a multifactorial basis for pathogenesis can be suspected.
In men, the lesions may be symptomatic, but if symptoms are present there may be retraction of the foreskin, which can lead to phimosis, painful erections, impaired urination and obstruction, tenderness and decreased sensitivity of the penis.
On examination, a sclerotic narrowing band is detected 1-2 cm distal to the foreskin, which leads to phimosis and paraphimosis. Later, porcelain-white spots, papules, and sclerotic changes may appear [Fig. 3] (12).
Histopathological changes include hyperkeratosis with follicular plugging, atrophy of the Malpighian layer with hydropic degeneration of basal cells, flattening of the reticular ridges, marked edema and homogenization of collagen in the upper dermis, and a lymphocytic infiltrate in the middermis.
Differential diagnosis includes erosive lichen planus, balanoposthitis of various etiologies and idiopathic phimosis.
Treatment is aimed at relieving symptoms with topical corticosteroids, tacrolimus ointment, and antihistamines. Intralesional steroids may be tried for resistant thick plaques that do not respond to topical steroids.
For post-inflammatory pain syndrome after regression of skin lesions (that is, penile dysesthesia), you can try 5% lignocaine ointment. Of course, treatment with potent steroids and/or circumcision appears to eliminate the risk of cancer in most men with LS (11).
The development of persistent skin lesions or chronic inflammation in patients with LS should be closely monitored and, if necessary, biopsied to ensure the absence of associated cancer.
Extramammary Paget's disease
It is a plaque that clinically and histologically resembles Paget's disease but occurs in areas rich in apocrine glands, such as the vulva, anogenital area, and axilla. It can arise either de novo or from an underlying carcinoma, which has shaped the concept of primary and secondary extramammary Paget's disease.
In approximately 75% of cases of extramammary Paget's disease, it arises as a primary intraepidermal neoplasm, most often from apocrine gland duct cells or from keratinocyte stem cells. In the remaining 25%, primary adenocarcinoma is found.
It is a rare disease with a predominance of women in the fifth decade of life or older. The disease presents as an irritated, itchy, burning, red, scaly patch or plaque and may be multifocal (13).
The edge is sharp, rounded, slightly raised. The surface may be scaly and have small grayish crusts over erosions. Pruritus is a significant feature, and excoriation and lichenification may also occur. IN
Variable hyperpigmentation makes it difficult to differentiate between extramammary Paget's disease and superficial spreading melanoma. Characteristic clinical features include continuous progression and growth despite aggressive treatment. As it progresses, the lesion may thicken and ulcerate as evidence of deeper invasion.
The most common area is the vulva, followed by the perianal area, which is more often affected in men than in women, the scrotum, penis and axilla. Appearance depends on the area affected.
The mucous surfaces of the labia are often more red than the skin, and the lesions may extend to the thighs, pubis, and vagina.
Perianal lesions may extend upward into the anal canal, and lesions on the scrotum may extend to the thigh or penile shaft. The eyelids or ears may also rarely be affected.
Nearby lymph nodes may be involved or distant metastases may occur.
Differential diagnosis from eczema, intertrigo, and vulvar pruritus is based on distribution, lack of response to topical anti-inflammatory agents, and sudden and peripheral growth. BD, leukoplakia, and superficial spreading melanoma are other differential diagnoses that require biopsy for diagnosis.
Histological manifestations in the epidermis are similar to Paget's disease. The epidermis is diffusely infiltrated with large vacuolated cells with bluish cytoplasm; they are called Paget's cells. These distinctive cells are found in the lower part of the epidermis and can proliferate into the reticular ridges and skin appendages.
The epidermis exhibits varying degrees of acanthosis, hyperkeratosis, and parakeratosis. Cells stain positively for acidic and neutral mucopolysaccharides. Immunohistochemistry shows cells positive for carcinoembryonic antigen, cyclic adenosine monophosphate 5.2, and low molecular weight keratins such as cytokeratin 7.
If a malignant tumor is present, it should be removed along with all clinically abnormal epithelium. Mohs surgery may be performed.
The most common cause of relapse is inadequate excision of the lesion. PDT is also useful, but larger series and longer study periods are required.
Cutaneous horn of the penis
The cutaneous horn is a well-defined cone-shaped lesion with hyperkeratosis that occurs in areas of chronic inflammation. It is known that warts, nevi, preputial inflammation and phimosis play an important role. Cutaneous horn most often appears on parts of the body exposed to the sun, so it rarely affects the penis.
The first case of cutaneous horn was described in 1854, and since then fewer than 100 cases have been reported. They have a risk of malignant transformation into low-grade verrucous or keratinizing SCC in approximately 30% of cases (14).
Malignant transformation should be suspected in rapidly growing lesions.
Various lesions seen in the setting of cutaneous horn include SCC, actinic keratosis, keratoacanthoma, BD, seborrheic keratosis, basal cell carcinoma, hemangioma, keratotic and mica-papillomatous balanitis, Kaposi's sarcoma, sebaceous adenoma, extramammary Paget's disease, pseudoepitheliomatous mica and keratotic balanitis and verrucous carcinoma (15).
The decision to treat should be made after adequate excision and histological examination of the entire lesion. Microscopically, the cutaneous horn is represented by pronounced hyperkeratosis, acanthosis, dyskeratosis, papillomatosis and chronic inflammatory infiltration of the adjacent dermis.
Treatment options include wide surgical excision, which includes partial penectomy with or without regional lymph node dissection. Carbon dioxide (CO2) or neodymium yttrium aluminum garnet (Nd:YAG) laser is the second line of treatment. Follow-up is mandatory as relapse may occur.
Pseudo-epitheliomatous, mica and keratotic balanitis
PKMB is an extremely rare disease that occurs on the glans, characterized by a silvery-white plaque with a mica-like crust, which is mainly observed in older adults (over 60 years of age) [Fig. 4] (16).
The exact etiology is not known. The pathogenesis of PKMB occurs in four stages: a) early plaque stage, b) late tumor stage, c) verrucous carcinoma, and d) transformation to SCC and invasion (14). Differential diagnoses include SCC, verrucous carcinoma, keratoacanthoma, giant condyloma, penile cutaneous horn, and EC.
Histological examination reveals hyperkeratosis, parakeratosis, acanthosis, elongation of the reticular ridges and mild dysplasia of the lower epidermis with a nonspecific inflammatory infiltrate of the skin with eosinophils and lymphocytes.
Treatment is based on the stage of the lesion, with early stage plaque requiring topical therapy and later stages requiring more aggressive therapy. Treatment includes topical 5-fluorouracil and cryotherapy if malignancy is present (16) and surgical excision of the malignancy is required. Mohs micrographic surgery may be used.
Leukoplakia
Leukoplakia is rare and is a white, verrucous plaque that can appear on the surface of the mucous membranes. Oral lesions have a strong association with chronic tobacco use and have a high risk of developing malignancies, which increase with the appearance of fissures, ulcerations and erosions.
The mucous membrane of the genital organs is rarely affected. Lesions occur predominantly on the glans or foreskin. Diabetics are more likely to suffer. Clinically, they may resemble areas of LS. There are mainly two clinical types: homogeneous and heterogeneous.
It has no specific histology and dysplasia may or may not be present. Approximately 10%–20% of penile leukoplakia may present with dysplastic changes microscopically (17). Treatment involves addressing etiologic factors, and if biopsy shows dysplastic changes, surgical excision is the treatment of choice.
Porokeratosis
Porokeratosis is a pronounced disorder of keratinization. It usually has an autosomal dominant pattern of inheritance. The exact etiology is unknown, but it has been suggested that a mutant clone of keratinocytes may be responsible, which is supported by the fact that abnormal DNA ploidy is present in porokeratosis keratinocytes.
Another theory is that an unknown epidermal antigen causes a mitotic stimulus for epidermal cells. A genetic role is also suggested. There are different types of porokeratosis, such as classic Mibelli porokeratosis, disseminated forms, punctate porokeratosis, linear porokeratosis and other rare variants.
It can be localized anywhere, especially on the face, “v” area of the neck and extensor surfaces of the limbs.
Clinically, it presents as hyperkeratotic papules or plaques surrounded by a band-like raised border that expands centrifugally.
Genital porokeratosis of Mibelli itself is rare, but classic lesions have been reported on the penis and scrotum, which is common in Asian populations (18). Itching and ulceration may occur.
Characteristic histopathological features are present in the hyperkeratotic fold. It is represented by a horny plate, a parakeratotic column in which the horny cells appear homogeneous and have deeply basophilic pyknotic nuclei.
Epidermal cells at the base of the stratum corneum are unevenly distributed and have pyknotic nuclei with perinuclear redema. The granular layer is absent under the horny plate. The dermis has a weak infiltration of lymphohistiocytic cells.
Porokeratosis may be confused with psoriasis, BD, granuloma, or lichen planus; biopsy differentiates these conditions. Treatment includes the use of emollients and monitoring for possible signs of malignant degeneration.
Topical 5-FU can induce remission in all cases, but relapses are occasionally observed. Topical imiquimod cream has also been shown to be effective.
Oral retinoids have been tried in immunocompromised patients who are at higher risk of malignant degeneration. Excision is most appropriate when malignant transformation develops.
Treatment
There are several different options and treatments for precancerous lesions on the penis. The choice of treatment should be tailored to the type and location of the lesion, taking into account patient preferences and likely compliance with treatment regimens, as well as the need for close monitoring using minimally invasive techniques.
Vaccination against human papillomavirus
Naturally, “prevention rather than cure” is a much more attractive therapeutic proposition in this clinical area. The advent of new HPV vaccines (both bivalent and quadrivalent) has sparked an interesting debate about genital cancer in men.
Protection against HPV infection is provided for up to 5 years after vaccination. The CDC currently recommends the HPV vaccine for all boys aged 11 or 12 years and catch-up vaccination for men aged 13–21 years who have not yet received all three doses (19).
Topical therapy
Local treatment of precancerous lesions of the penis can be carried out with either chemotherapy or immunotherapy. They are best suited for immunocompetent patients with severe single lesions.
Lesions amenable to topical therapy include penile intraepithelial neoplasia (PIN), PD, and PKMB. It is not suitable for LS, GCA or cutaneous horn. The most common first-line treatment is topical 5% 5-FU. This antimetabolic chemotherapeutic agent is a pyrimidine analogue. It is used topically for 4-6 weeks every other day.
Patients are generally advised to apply the cream with or without gloves and to wash their hands thoroughly after application. This is because the treated area often becomes crusty and inflamed during the treatment period. Additional use of a topical steroid is possible if discomfort occurs during the treatment period.
However, these areas may take 4 to 8 weeks to heal. Refractors or partial responders to this treatment may receive immunotherapy using topical imiquimod 5% cream as second-line treatment for 5 days per week for 4 to 6 weeks. The frequency of use may be reduced if the inflammatory response persists.
Laser therapy
Laser therapy is mainly used to treat PIN and PD and is not suitable for LS, GCA or cutaneous horn. CO2 and Nd:YAG lasers are used as first-line therapy with sufficient response and good results. The CO2 laser has a tissue penetration of 2-2.5 mm and can be used as a scalpel to excise tissue for histological analysis by directly focusing the beam.
Treated areas usually heal within 3-4 weeks. The Nd:YAG laser has a tissue penetration of 3-5 mm, but causes tissue coagulation, preventing histological diagnosis, which may cause the disease to progress to the next stage.
Larger lesions can be treated with this laser, but ablation sites may also take 2-3 months to heal. Treatment with any of these lasers is usually well tolerated, with minor complications ranging from minor pain and bleeding at the treatment sites.
Laser has a higher rate of recurrence and disease progression, which may reflect a tendency to remove larger lesions with this minimally invasive approach compared with those treated with other topical treatments.
Cryotherapy
The method can be used in a wide range of skin diseases using a method involving the use of liquid nitrogen or nitrous oxide to create rapid freeze/slow thaw cycles to achieve tissue damage at temperatures below -20 by the formation of ice crystals, which leads to destruction of cell membranes and death cells.
Cryotherapy has a greater risk of recurrence in some cases compared with 5 FU and surgical excision after 5 years of follow-up (20).
Topical photodynamic therapy
PDT for precancerous penile lesions is still under investigation. A topical photosensitizing cream such as delta-5-aminolevulinic acid is applied to the penis for about 3 hours, which is then absorbed and retained by the malignant cells.
This area is then treated with incoherent light from a special PDT lamp, which leads to photoselective death of the sensitized cells. No intra- or perioperative side effects of photodynamic diagnostics were observed (21).
Surgical excision - circumcision
the method is an integral part of the treatment of precancerous conditions to treat and prevent the persistence of formations characteristic of HPV infection, chronic inflammation and the progression of invasive formations.
Surgical excision is the treatment of choice for all precancerous lesions. Primary surgical excision is recommended for extensive lesions, poor compliance, and recurrences.
The total glans resurfacing procedure provides the best surgical approach in which the affected area is excised, followed by a skin graft (22). This allows you to maintain the length, shape and function of the penis, as well as a good cosmetic appearance.
Partial glans resurfacing has also been used as the primary surgical approach for the treatment of glanular CIS. This approach has the advantage of preserving normal scalp skin, which allows for better preservation of glans sensation and a final appearance closer to original.
This approach would be more attractive to young, sexually active men.
An alternative surgical approach is excision using Mohs micrographic surgery. This involves removing the entire lesion in thin sections with simultaneous histological examination to ensure clear margins microscopically.
Although this technique allows for maximum preservation of normal penile tissue, it is complex and time-consuming, requires both a surgeon and a pathologist trained in this technique to ensure an adequate oncologic outcome, and has a higher likelihood of recurrence (23).
Conclusion
Some genital lesions that appear to be inflammatory in nature may actually be precancerous lesions that can develop into aggressive tumors.
In modern clinical practice, the possibility of non-infectious lesions of the genital organs is often underestimated, with a tendency to attribute sexually transmitted origin to any pathological condition affecting the genital organs, especially in young people.
Therefore, it is important to be aware of these cases. Their diagnosis is mainly based on the typical clinical presentation and in some cases on histopathological examination, which should always be performed as clinically indicated.
Symptoms of penile cancer
Sometimes penile cancer does not cause symptoms. A malignant tumor may be indicated by such signs as strange spots and rashes, thickening of the skin, ulcers, accumulation of contents with an unpleasant odor under the foreskin, bleeding from the urethra or from under the foreskin, lumps, warts. One of the possible symptoms of cancer of the head of the penis is its swelling. The “bump” in the groin may be enlarged due to damage to the lymph node by cancer cells.
All of these signs do not necessarily indicate penile cancer. This is how other, less dangerous diseases can manifest themselves. You need to visit a doctor as soon as possible. If changes on the penis turn out to be a malignant tumor, it is important to begin treatment as soon as possible.
How is condylomatosis transmitted and how to protect yourself from it?
There are three common ways of transmitting HPV, which leads to the appearance of condylomas on the male genital organ.
- Unprotected sexual contact and protected sex with a sick partner
. Even using a condom does not protect 100% from the virus. During sexual intercourse, cells of the affected epithelium penetrate the mucous tissues of a healthy partner, and this is the most common method of infection among people 18-35 years old. - During childbirth from mother to child
. The baby is born already infected, and neoplasms on the child’s penis can be seen already in the first year of life. - Contact and household method
. This happens extremely rarely, mainly in conditions of lack of sanitation (when using one razor, a shared towel or comb) and only if there is microtrauma on the surface of the skin.
A person can be a carrier of HPV, but he or she will not develop condylomas until the carrier of the virus has a weakened immune system. In this case, the affected epithelium will begin to multiply atypically (with the formation of cells unusual for this tissue), forming condylomas on the surface.
Condylomas pose the greatest danger to women, in whom in 99.9% of cases the disease is the cause of cervical cancer, therefore, upon learning about your disease, you must definitely warn your partner. Girls who are promptly vaccinated with the Gardasil vaccine against HPV have a lower risk of infection. By the way, this vaccination is also given to young men.
Diagnostics
The most accurate method for diagnosing penile cancer is a biopsy. The doctor removes the entire pathological tissue ( excisional biopsy ) or a fragment of it ( incisional biopsy ) and sends it to the laboratory for examination under a microscope. If cancer cells are found in the sample, the diagnosis leaves little doubt.
If enlarged lymph nodes are found, a biopsy may also be performed. The material for research is obtained using a needle or by surgically removing lymph nodes.
After penile cancer is diagnosed, the doctor may prescribe an ultrasound, computed tomography, MRI - these studies help assess how much the tumor has invaded neighboring tissues and spread to the lymph nodes.
Causes of polyps
The reasons for the development of polyps of the uterus, cervix, vagina or vulva are the same. The most likely factor predisposing to the appearance of formations is hormonal imbalance. This is especially true for glandular forms. Due to increased production of sex hormones or, conversely, a decrease in it, glandular cells begin to actively divide. More often, the spread of pathology throughout the body of the uterus is associated with ovarian dysfunction.
The disease is also caused by violations of tissue integrity, trauma, burns, which lead to necrosis of functional tissue and its replacement by connective (fibrous) tissue. For example, polyps develop with the following problems:
- Endometritis;
- Erosion;
- Vulvovaginitis and vaginitis;
- Injuries during surgical abortions.
Long-term wearing of an intrauterine device, as well as taking hormonal contraceptives, can also lead to the development of tumors.
There is a high risk of pathology in the following cases:
- Chronic arterial hypertension;
- Endocrine and autoimmune diseases;
- Obesity;
- Cardiovascular diseases;
- Neuropsychiatric disorders.
Metabolic disorders are also a common cause of the development of anomalies of the female genital organs.
Classification, stages of penile cancer
In 95% of cases, the tumor is squamous cell carcinoma of the penis , or squamous cell carcinoma . It usually grows slowly and is often diagnosed in its early stages and treated successfully. A malignant neoplasm can be located on any part of the penis; the most common is squamous cell carcinoma of the head of the penis and foreskin.
Much less common are warty carcinomas , or Buschke-Lowenstein tumors . Outwardly, they resemble large warts. This cancer also grows slowly, can reach large sizes, grow deeply into neighboring tissues, but rarely spreads to other parts of the body.
Melanomas occur on the skin of the penis, as in other places . This localization is not very typical, since melanoma most often appears on areas of the skin exposed to sunlight. This is an aggressive tumor, it metastasizes early and often has a poor prognosis.
Another slow-growing and very rare type of penile skin cancer is basal cell carcinoma , or basal cell carcinoma . Adenocarcinomas, malignant tumors from sweat gland cells, are extremely rare on the skin of the penis.
Depending on the size of the main tumor (T), the spread of cells to nearby lymph nodes (N) and the presence of distant metastases (M), the following stages of penile cancer are distinguished:
- Stage 0 : a tumor that is located in the superficial layers of the skin and does not spread deeper. This is the so-called “cancer in situ”.
- Stage I : the tumor has grown into the skin somewhat more strongly, but has not yet invaded adjacent tissues.
- Stage II : a tumor that has grown into the blood vessels, lymphatic vessels, spongy body, cavernous body, or into the urethra, or cancer cells have a low degree of differentiation and have completely lost their resemblance to normal ones.
- Stage III : The tumor has not grown beyond the penis, and the tumor cells have spread to one (substage IIIA) or more (substage IIIB) lymph nodes in the groin.
- Stage IV: the tumor has grown into the scrotum, prostate, pubic bones, or cancer cells have spread to the inguinal lymph nodes and have grown from them into surrounding tissues, or there are distant metastases.
Write to an oncologist
Stages of the disease
Staging of penile cancer is carried out according to the international TNM classification, where T is a description of the primary tumor, N is the condition of regional lymph nodes, M is distant metastases.
| Stage | T | N | M |
| 0 | is – carcinoma in situ; a – non-invasive verrucous (warty) carcinoma without destructive infiltrative growth | 0 – no palpable or visually enlarged inguinal lymph nodes | 0 – absence of distant metastases |
| I | 1 – invasion into subepithelial connective tissue | 0 – no palpable or visually enlarged inguinal lymph nodes | 0 – absence of distant metastases |
| II | 1-2 – invasion into subepithelial connective tissue; ingrowth into the corpus spongiosum with or without invasion of the urethra | 1 – a mobile palpable enlarged inguinal lymph node is determined on one side | 0 – absence of distant metastases |
| 2 – ingrowth into the corpus spongiosum with or without invasion of the urethra | 0-1 – there are no palpable or visually enlarged inguinal lymph nodes; palpable mobile palpable enlarged inguinal lymph node on one side | 0 – absence of distant metastases | |
| III | 1-3 – invasion into subepithelial connective tissue; ingrowth into the corpus spongiosum with or without invasion of the urethra; ingrowth into the corpus cavernosum with or without invasion of the urethra | 2 – mobile palpable inguinal lymph nodes on both sides or multiple | 0 – absence of distant metastases |
| 3 – ingrowth into the corpus cavernosum with or without invasion of the urethra | 0-2 – there are no palpable or visually enlarged inguinal lymph nodes; a mobile palpable enlarged inguinal lymph node is palpated on one side; mobile palpable inguinal lymph nodes on both sides or multiple | 0 – absence of distant metastases | |
| IV | 4 – tumor spread to other surrounding structures | 0 – no palpable or visually enlarged inguinal lymph nodes | 0 – absence of distant metastases |
| 1-3 – invasion into subepithelial connective tissue; ingrowth into the corpus spongiosum with or without invasion of the urethra; ingrowth into the corpus cavernosum with or without invasion of the urethra | 3 – fixed conglomerate of inguinal lymph nodes or enlarged pelvic lymph nodes on one side or both sides | 0 – absence of distant metastases | |
| 1 – there are distant metastases |
For squamous cell carcinoma, the histopathological grade of differentiation (G) is also indicated:
- Gx – insufficient data to assess histological differentiation;
- G1 – well-differentiated tumor;
- G2 – moderately differentiated tumor;
- G3 – poorly differentiated or undifferentiated tumor.
Surgery for penile cancer
Surgical removal of the tumor is the main treatment for penile cancer and can be used at almost any stage. If the cancer is within the foreskin, circumcision is performed. If the tumor is small and has not had time to grow deeply, it is removed with a small amount of surrounding healthy tissue. Such interventions are organ-preserving, after which all functions of the penis are preserved.
For large, deeply growing tumors, it is necessary to remove part of the penis or the entire organ. The consequences of such operations for penile cancer: disruption of the appearance of the genital organs and the ability to perform sexual intercourse, psychological discomfort.
When the entire penis is removed, the doctor creates a new hole in the perineum for the outflow of urine. After surgery, a man can still control the process of urination, but from now on he will have to urinate while sitting. Sometimes the scrotum and testicles have to be removed along with the penis, that is, castration must be performed.
Surgical intervention can be supplemented by removal of lymph nodes in the groin area. Previously, such operations were performed more often and on a larger scale, since the surgeon could not know for sure how many nodes were affected by cancer cells. Many men experienced a complication - lymphedema , swelling of the leg due to impaired lymph outflow.
Currently, there is a study that can be performed directly during surgery - sentinel biopsy , or sentinel lymph node biopsy . The surgeon injects a special dye into the tumor and looks at which lymph node it goes to first. This lymph node is called the sentinel lymph node. It is removed and examined for the presence of cancer cells. Depending on the result, a decision is made about the need to remove other lymph nodes.
Thanks to sentinel biopsy, surgeons remove inguinal lymph nodes only in cases where it is actually necessary.
1.General information
The term “polyp” in medicine refers to the growth of tissue in an area where nature does not provide any bulges. Polyps (for example, in the intestines, nose, etc.) are benign neoplasms. Often they do not manifest themselves in any way, and are discovered purely by chance, during a preventive or diagnostic examination for another reason. However, when they reach a certain size, polyps can cause serious problems associated, in particular, with pressure on surrounding tissues, the risk of traumatic injury and malignant degeneration.
All of the above fully applies to such an unpleasant formation as a urethral polyp. The urethra, or urethra, is the terminal portion of the urinary tract; Through the external opening of the urethra, renal filtration waste accumulated in the bladder is evacuated from the body to the outside. Any interference along this path complicates the passage (free flow) of urine, which ultimately leads to dysfunction and pathological changes in the entire genitourinary system, and sometimes, if the lumen of the urethra is completely blocked and the so-called develops. acute urinary retention creates a direct threat to life.
The peculiarities of the anatomical structure of the male and female body determine significant differences in the distal (most distant) segment of the urinary tract: in women, the urethra is thicker, straighter and several times shorter. This circumstance makes the female urethra, in general, more vulnerable to diseases, primarily infectious ones. Urethral polyps are also much more common in women than in men. In addition, polypous growths on the internal mucous surface of the urethra in male patients are usually detected deeper, i.e. closer to the bladder, namely in the part of the urethra that passes through the prostate.
However, in representatives of both sexes, a polyp can develop directly in the external opening, where it is, of course, easier to detect.
A must read! Help with treatment and hospitalization!
Chemotherapy
Chemotherapy for penile cancer is used before surgery to reduce the size of the tumor, after surgery to prevent relapse, and in case of metastatic cancer. The drugs used are: capecitabine, mitomycin C, ifosfamide, paclitaxel, 5-fluorouracil, cisplatin. Usually a combination of 2-3 drugs is used. Treatment is carried out in cycles: after each administration of the drug there is a break of several days. Cycles can last 3–4 weeks, the general course of treatment includes several cycles.
Find out the exact cost of treatment
Relapse problem
Performing organ-sparing operations provides a higher quality of life, but is associated with a higher risk of local relapse compared to amputation of the penis. In this regard, regular monitoring of the patient (physical and instrumental examination) is necessary in the postoperative period. As a rule, relapses are superficial, and their timely detection allows for minimally invasive intervention and preservation of the organ, which will provide a good chance of long-term remission.
Complications of condylomatosis: genital warts are very dangerous!
If you ignore tumors on the genitals or glans, the following problems will arise:
- Spread of condylomas to the urethra
. They block the urethra, leading to inflammation and viral urethritis. - Viral infection of the rectum
leads to the formation of paraproctitis, which interferes with bowel movements, causes severe pain, bleeding, and is difficult to treat. - The exophytic nature of condylomas
is that they grow inside the organ. - Condyloma has the ability to degenerate into a cancerous tumor
. With reduced immunity, the virus that infects the epithelial cell (the upper layer of the skin) begins to produce new cells that differ in structure from the maternal one (atypical). This is how condyloma degenerates into cancer. - Condylomas have an unaesthetic appearance
, causing disgust in the partner. A man may experience psychological and even physical discomfort during sexual intercourse, which significantly reduces the quality of sexual life. - Men suffering from diabetes mellitus have wide lesions of the foreskin, and their inguinal lymph nodes become inflamed.
- Phimosis
develops - the inability of the foreskin to expose the head of the penis. - In advanced cases, pus accumulates around condylomas, and the patient experiences unbearable pain.
- Condylomas located at the opening of the urethra impede the passage of urine and cause general intoxication of the body, which leads to decreased vitality, drowsiness, poor health, and depression.
In 100% of cases, the patient’s regular partner also becomes infected with HPV.
Prevention of penile cancer
The likelihood of developing the disease sharply decreases after circumcision (in medical parlance - circumcision) - an operation during which the foreskin is removed. There is virtually no incidence of squamous cell carcinoma of the penis in circumcised men. Other preventive measures:
- Careful personal hygiene.
- To give up smoking.
- Avoiding promiscuity and using condoms: This reduces the risk of contracting HIV and HPV.
| More information about treatment at Euroonco: | |
| Urologists-oncologists | from 5,100 rub. |
| Chemotherapy appointment | RUB 6,900 |
| Radiologist consultation | RUB 11,500 |
| Palliative care in Moscow | from 44,300 rubles per day |
Book a consultation 24 hours a day
+7+7+78
4.Treatment
Traditionally, and for a long time, the only method of removing polyps was to cut off their stems with a special loop. However, medical technologies are developing rapidly, and today the methodology has stepped far forward. If the polyp is located externally, an electrocoagulator or liquid nitrogen (cryodestructor) can be used; deeper growths are removed using modern minimally invasive endoscopic instruments. Currently, various models and designs of radioknives, medical lasers, etc. are widely used in urological practice.
It is important to emphasize that therapeutic success directly depends on the timeliness of seeking help, and the likelihood of relapse is determined by how adequately and effectively all existing foci of infections were treated. To suppress the activity of the papillomavirus, one should, in particular, follow all immunostimulating instructions, and to avoid re-infection and scarring urogenital inflammation, strictly adhere to the principles of personal hygiene and safe sex.
The possibilities of conservative treatment of urethral polyps are currently not seriously discussed.