A lipoma on the neck is a benign pathological formation consisting of fat cells. Locations: under the jaw, front, side and back of the neck. There are single and multiple lipomatous formations that arise both in internal organs and on the surface of the skin. The size of the cervical growth reaches up to 20 centimeters in diameter. Wen is characterized by slow growth and absence of symptoms at an early stage of development. Reaching a substantial size, the wen puts pressure on nerve endings and blood vessels.
The occurrence of pathology does not depend on age, body weight and gender. Despite its nature, a tumor can transform into a cancerous form at a late stage of development.
Types of skin pathologies
Wen that appears in the neck area are divided into the following types:
- a tumor consisting entirely of adipose tissue and having a capsule is called a soft tissue wen;
- a large wen without a capsule is known as a diffuse tumor;
- a growth that has a hardened capsule inside, consisting of both fatty and connective tissue, is called a fibrous tumor;
- a neoplasm partially consisting of muscle tissue is called myolipoma;
- multiple formations spreading to the head and neck area are called lipomatosis;
- the wen that touches the nerve fibers is called perineural;
- a tumor containing calcium is known as angiolipoma;
- a growth affecting the sweat glands is called adenolipoma;
- a wen that arises on the cervical vertebra and blocks the blood duct is known as Bichat's hump.
Bish's hump
Ultrasound diagnosis of neck lipomas
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Currently, ultrasound is the leading method for the differential diagnosis of tumors of the thyroid gland and adjacent soft tissues of the neck [6-8,10]. According to the Moscow Oncology Center, adipose tissue tumors account for about 13% of all non-organ neoplasms and 45% of tumors derived from mesenchyme [3]. Among them, lipomas, diffuse lipomatosis, and liposarcoma are distinguished [4]. Solitary lipomas are most often observed. They are characterized by slow growth and occur with equal frequency in men and women [5]. Lipomas have a thin, well-defined capsule. Microscopically, mature lipomas consist of adipose tissue and represent accumulations of fat cells located in the connective tissue stroma, the ratio between which is different. Malignant tumors from adipose tissue are rare [9].
Solitary lipomas have different shapes and are localized on the back, less often on the lateral or anterior surfaces of the neck. Depending on the depth of location, several types of lipomas are distinguished: I - superficial, localized in the subcutaneous tissue, II - fascial-muscular, located in the fascia of the neck or muscles and enclosed between the fascial layers, III - paravisceral, located near the trachea, thyroid gland, pharynx and the cervical esophagus, between the muscular and vertebral fascia [1]. With solitary superficial lipomas, neck asymmetry is usually observed. Diagnosing them by palpation is not difficult. They have a pasty consistency, are mobile, and when localized on the anterior surface they can simulate a goiter. Diagnosing deep neck lipomas is more difficult. They are usually recognized either after the appearance of compression syndrome of nearby organs or vessels, or as incidental findings during ultrasound of the neck. We present four cases of superficial and deep neck lipomas identified during mass preventive examinations of people living in areas contaminated with radionuclides after the accident at the Chernobyl nuclear power plant.
Materials and methods
Ultrasound of the neck and thyroid gland was performed according to a standard technique using sensors with a frequency of 7.5 MHz [11]. 4 patients (2 men and 2 women) aged 9, 12, 45 and 53 years were examined. We present the corresponding observation.
Case 1
Patient A., 12 years old. A routine examination revealed uneven thickening of the left half of the neck. A clinical examination in the area of the left lobe of the thyroid gland revealed a tumor formation of doughy consistency measuring 7×4 cm. When scanning, a decrease in the accumulation of the radioisotope drug in the left lobe of the thyroid gland was noted. Ultrasound examination: the left lobe of the thyroid gland is displaced upward, its size is reduced. Posterior to it, an oval-shaped formation with clear outer contours measuring 3.2×2.2×7.8 cm is determined. The formation has a heterogeneous structure due to areas of reduced density (along the periphery) and areas of increased density of a linear shape, occupying almost the entire area of the formation (Fig. 1a, b).
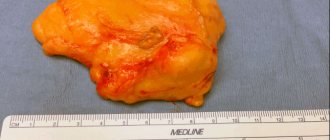
A puncture biopsy was performed under ultrasound guidance. Cytological examination: adipose tissue. Operation: behind the left lobe of the thyroid gland a formation is detected, 7x4x3 cm in size, yellow in color, in a capsule, with a uniform doughy consistency. The left lobe of the gland is of normal consistency, reduced in size. Histological examination of a distant formation: lipoma. Dynamic echography, 6 months after surgery, showed that the left lobe of the thyroid gland was located normally, reduced in size, and no signs of lipoma recurrence were detected in the area of the postoperative bed (Fig. 1c).
Rice. 1.
Deep lipoma of the neck. Echograms of the thyroid gland in the transverse (a) and longitudinal (b) planes. Posterior to the reduced left lobe of the thyroid gland, a formation of increased density is detected, displacing it anteriorly. Echogram of the thyroid gland in the transverse (c) plane 6 months after surgery: no signs of lipoma recurrence were detected, the location of the left lobe is normal.
Case 2
Patient B., 9 years old. A clinical examination revealed a formation in the area of the right lobe of the thyroid gland, which gradually increased over the course of 1 year. During a clinical study at the Medical Research Center of the Russian Academy of Medical Sciences, in the projection of the right lobe of the thyroid gland, a formation of soft-elastic consistency measuring 3x2 cm was determined. According to the scanning data, the location, shape and size of the thyroid gland were normal, the accumulation of the drug was uniform, the palpable formation was not clearly displayed on scanograms. Ultrasound examination: the shape and size of the thyroid gland are normal, the structure is homogeneous, without focal changes. In front of the right lobe of the thyroid gland there is an oval-shaped formation with fairly clear contours, measuring 2.7×1.3×3.6 cm. The structure of the formation is heterogeneous due to linear areas of increased density, between which areas of reduced density are defined (Fig. 2a , b).
Rice. 2.
Lipoma of the neck (fascial-muscular). An echogram of the right half of the neck in the transverse (a) and longitudinal (b) planes: an increased density spindle-shaped formation is determined anterior to the thyroid gland. The right lobe of the thyroid gland is unchanged.
A puncture was performed under ultrasound guidance. Cytological examination: adipose tissue. Operation: between the short muscles of the neck and the anterior surface of the right lobe, a yellow formation was detected in the capsule, 3x2x1.5 cm in size, doughy consistency and equal density. Histological examination: mature adipose tissue in the capsule (lipoma).
Case 3
Patient P., 46 years old. A preventive examination revealed a moderate deformation of the right half of the neck due to a painless neoplasm of soft elastic consistency. Preliminary diagnosis: lateral neck cyst. During a clinical study at the Medical Research Center of the Russian Academy of Medical Sciences, in the area of the right lobe of the thyroid gland, a formation of doughy consistency, painless, displaceable, measuring 3x2 cm was determined. An ultrasound examination over the right lobe of the thyroid gland visualized a spindle-shaped formation, with clear contours and a thin capsule. The structure of the formation is heterogeneous due to areas of increased density of a linear shape and pockets of low density located between them. The size of the formation is 2.4 × 1.2 × 3.2 (see Fig. A, b). No pathological changes were detected in the thyroid gland.
Rice. 3.
Lipoma of the neck (fascial-muscular). Echogram of the right half of the neck in the transverse (a) and longitudinal (b) planes: anterior to the unchanged right lobe of the thyroid gland, an oval-shaped formation of a heterogeneous structure is determined, the short muscles of the neck are displaced anteriorly.
Ultrasound-guided needle biopsy: fat cells. During dynamic clinical and ultrasound observation for 4 years, no signs of enlargement of the formation or changes in its structure were revealed. Clinical diagnosis: soft tissue lipoma of the neck.
Case 4
Patient K., 53 years old. A preventive ultrasound examination outward from the right lobe of the thyroid gland revealed an oval-shaped formation with clear, even contours and a thin capsule, the short muscles of the neck were displaced posteriorly. The size of the formation is 0.9×6.6×6.6 cm (Fig. 4a, b). The thyroid gland is not changed, the location of the neck vessels and their sizes are normal.
Rice. 4.
Superficial lipoma. Echograms of the right half of the neck and the right lobe of the thyroid gland in the transverse (a) and longitudinal (b) planes: the formation of reduced echo density of a spindle-shaped form is determined subcutaneously. The right lobe of the thyroid gland is unchanged, the neck muscles are displaced posteriorly.
Ultrasound-guided puncture: adipose tissue cells are obtained. During dynamic clinical and ultrasound observation for 3 years, the size of the formation and its structure did not change, and no additional cystic or nodular formations were identified. Clinical diagnosis: soft tissue lipoma of the neck.
Discussion
Our data indicate that modern ultrasound devices with high resolution make it possible to reliably differentiate tumors of the soft tissues of the neck, including lipomas, from pathological formations located in the thyroid gland. In our observations, in one case the lipoma was located paraviscerally, in two cases - between the fascial layers (fascial-muscular), in the last case - superficially in the subcutaneous tissue. With a paravisceral location (case 1), the lipoma was located near the trachea, pushing the left lobe of the thyroid gland anteriorly and the vessels of the neck laterally. With fascial-muscular localization, lipomas were located between the short muscles of the neck and the anterior surface of the thyroid gland, pushing the muscles anteriorly. With a superficial location, the lipoma was localized directly under the skin in the subcutaneous tissue, causing a posterior displacement of the neck muscles. In three patients, the ultrasound image of deep neck lipomas was characterized by the presence of a uniform alternation of linear areas of increased density with small foci of reduced echogenicity located between them. In the last observation (case 4), the lipoma appeared as a spindle-shaped formation of reduced density.
It should be noted that in all cases, lipomas were clearly differentiated against the background of the neck muscles, thyroid parenchyma and great vessels. The different echogenicity of lipomas, in our opinion, is explained by the unequal ratio of fatty and connective tissue components, since when the latter predominates, their reflectivity increases. Ultrasound-guided needle biopsy is a valuable additional diagnostic method. All patients had adipose tissue in their smears. This facilitates the preoperative differential diagnosis of solitary neck lipomas located in the paravisceral spaces and allows choosing rational tactics for their treatment.
Literature
- Barkov A.D., Krichevsky A.A. About deep lipomas of the neck // Issues of oncology. - 1961.- 9. - P. 89-92.
- Oshmyanskaya A.I. Mesodermal tumors of the neck // Issues of oncology. - 1971. - 1. - P. 119-120.
- Oshmyanskaya A.I. Mesodermal and neuroectodermal tumors of the neck / Abstract of doctoral dissertation. - 1977. - 19 p.
- Bouffant AM. Tumors of the head and neck. - M.: Medicine, 1983.
- Falileev G.V. Neck tumors. - M.: Medicine, 1978.
- BrunetonJ.N. Ultrasonography of the Neck. Heidelberg: Springer. — 1987.
- Bruneton J.N., Mourou MY Ultrasound in salivary gland disease. ORL 1993; 55: 284-289
- Gooding GAW Sonography of the thyroid and parathyroid. Radiologic clinics of North America 1993; 31:5:967-989
- Pack G., Ariel J. Tumor of the soft somatic tissues. New York, 1958
- Robert J. Baatenburg de Jong, Robert J. Rongen. Guidelines for the use of ultrasound in the head and neck. ORL 1993; 55:309-312
- Parsbin VS, Ilyin AA, Tsyb AF Age dynamics of changes in thyroid volume. Acta Med. Nagasaki 1994; 39:4:172-175
Ultrasound scanner WS80
An ideal tool for prenatal research.
Unique image quality and a full range of diagnostic programs for an expert assessment of a woman’s health.
Factors causing the occurrence of wen
The reasons for the appearance of a subcutaneous tumor are still not clear, but possible factors include:
- heredity;
- neglect of hygiene rules;
- presence of bad habits;
- physical and chemical effects on the area where pathology occurs;
- diseases of the digestive organs and slow metabolism;
- excessive consumption of junk food;
- hormonal imbalance in the body;
- lipid imbalance of the skin;
- diabetes;
- infectious skin lesion.
Symptoms of atheroma in children
In 80-85% of cases, apart from the visual defect, children do not present any other complaints. Uncomplicated atheroma is characterized by:
- painlessness;
- mobility;
- elasticity upon palpation.
The skin over the surface of the tumor is smooth and does not fold. The clinical picture may change when the contents of the atheroma become inflamed against the background of the addition of bacterial flora. In this case, patients may note:
- pain when pressed;
- redness and increase in size of the tumor itself;
- local increase in body temperature.
If the above symptoms occur, you should immediately seek help.
This situation threatens the penetration of infection into nearby tissues and blood with the spread of microorganisms to distant areas of the body and can cause a deterioration in the general condition of the child. Atheromas occur in areas of the skin that are rich in sebaceous glands. Therefore, they especially often have the following localization:
- scalp;
- face and neck area;
- shoulder girdle, armpit area;
- back.
Neoplasms occur less frequently in the groin area and scrotum (in boys). In these areas they have the appearance of a skin growth and require differential diagnosis with other skin tumors.
Symptoms of the disease
The primary symptom of the pathology is the presence of a soft, small growth under the skin in the neck area. The tumor makes itself felt at a late stage of development with the presence of the following signs:
- the size of the wen has noticeably increased;
- inflammatory processes around and on the surface of the growth;
- pronounced pallor of the skin in the area of pathology;
- painful sensations when pressing;
- the tumor loses its ability to move due to growth into the deep layers of the skin, touching blood vessels and nerve endings.
Wen on the neck has an adverse effect on the physical and mental state of a person, interfering with normal blood circulation and the functioning of the respiratory tract. The tumor often causes difficulty breathing and creates difficulties during the absorption of food, putting pressure on the esophagus. By compressing the phrenic nerve, the wen causes hiccups and coughing. Multiple lipomatosis spoils a person’s appearance and can cause complexes in the form of lack of self-acceptance.
Symptoms of a wen on the neck
Wen can be detected with the naked eye. Upon visual examination, a tumor is visible, rising above the skin, the color of which does not differ from the surrounding areas. Upon palpation, a small formation easily moves without causing any discomfort. The growth of the wen does not stop over time, it is constantly increasing.
Negative symptoms as a reason for urgent consultation with a surgeon:
- Skin hyperemia is a sign of the onset of the inflammatory process;
- Reduced mobility of the wen - the transition of the wen to deep structures or its soldering to the epidermis;
- Pain on palpation - the growing wen touches the nerve fibers;
- Pallor of the skin - compression of the blood vessels by the wen;
- A rapid increase in wen is a dangerous sign of malignancy or a symptom of a serious metabolic disorder.
The difference between a cervical lipoma and a lymph node
Lipoma of the cervical spine presents difficulties for self-diagnosis. The patient is often unable to distinguish a fatty growth from a lymph node. The true nature of a lipomatous tumor is revealed by the following signs:
- soft consistency of the wen contents;
- the ability to change color around the site of formation and the skin on the wen itself;
- the presence of inflammatory processes at a late stage of the disease;
- the wen is able to reach muscles and bone tissue as it grows progressively, putting pressure on nerve fibers and blood vessels;
- pathology can be located in any area of the human body, especially in places of maximum accumulation of fatty cell formations;
- the tumor can pose a risk of transformation into a malignant pathology;
- brings pain when pressed;
- at an early stage it does not benefit the body, and at a later stage it worsens the state of health, causing discomfort and unpleasant sensations in the cervical region.
A lymph node differs from a wen in the following ways:
Lymph node examination
- Warns of infection or virus entering the body, increasing in size.
- During inflammatory processes, the formation does not exceed the size of a pea.
- The skin is not susceptible to external changes and retains its color.
- Swelling and pigmentation of the lymph node were recorded during inflammatory processes.
- The anatomy of the formation is different: the bulk of the lymph node is lymphoid tissue. The presence of blood vessels, medulla, lymph and reticular fibers was discovered, which explains the density and elasticity of the lymph node.
- These formations are considered exclusively benign and have a beneficial effect on the human body. Being part of the lymphatic system, formations have a cleansing and antiviral effect on the human body. Inflammation of the lymphatic formations indicates the body’s fight against infections and viral diseases.
Arising on the left side of the neck, the wen is easily mistaken for a lymph node, since lymphatic formations most often arise on the sides of the cervical region.
Surgical method for removing wen
If a child’s wen is too large, what to do? Usually in this case surgery is needed.
Surgical intervention may be prescribed in several cases:
- if the tumor is larger than 5 or 7 centimeters;
- if the lipoma grows very quickly;
- if the tumor develops rapidly in an infant in the first year of life;
- if there are white wen on the child's face.
During surgery, when it is performed on a small child, only general anesthesia is used. If the child is an older child or a teenager, then a local anesthetic is injected subcutaneously. General anesthesia is also used when operating on a lipoma on the face of a child.
The operation is performed on an outpatient basis if the lipoma is small. For newborns and children of the first year of life, surgery is performed only inpatiently. Surgery is also performed in a hospital if a tumor of significant size needs to be removed.
Before the lipoma removal procedure, certain types of tests are performed. This is a general blood and urine test. The blood is also tested for clotting and its group is determined. In addition, sometimes a test is prescribed to check for syphilis and/or HIV, etc.
Single and multiple lipomatosis in children
People of any age are at risk of developing a fatty tumor. Infants and newborns are no exception. A child’s fatty tissue rapidly increases in size in a short time and causes pain. Often, lipomatosis is a congenital pathology in children under five years of age. The appearance of fatty formation is strictly forbidden to be ignored, and it is recommended to immediately consult a doctor. If the child’s body is affected by multiple lipomatosis, it is recommended to remove some of the large wen.
Fat growth is dangerous because the pathology transforms into a malignant tumor known as liposarcoma. A cancer cell forms in the muscle space, smoothly passing into the adipose tissue of the lipoma. Liposarcoma is a subcutaneous tubercle of irregular shape, reaching gigantic sizes. Most often, wen appear in the area of the extremities and on the back, less often - on the neck, face, head and in the area of the mammary glands.
Liposarcoma on the neck
The surface of liposarcoma has a pronounced yellow and gray tint. A cancerous tumor provokes anemia, interferes with the functioning of the circulatory system, causing numbness at the localization site, and depletes the child’s body. After surgery, the risk of liposarcoma recurrence is high - from 45% to 80% of patients undergo a second course of treatment and removal of the pathology.
The phenomenon mainly manifests itself in children, since the cells of a young body are susceptible to malignant transformations.
When to go to the doctor for help
After examining the lipoma, doctors themselves may delay prescribing treatment. But if symptoms such as:
- sharp and rapid growth of wen
- change in skin color and lipoma shape
- the appearance of redness or inflammation around the lipoma itself
- when squeezing or pressing, pain occurs
- release of any liquid (substance) from the wen
- appearance of a foreign pungent odor
If any of the above symptoms appear, it is best to contact a medical institution, where the doctor will prescribe all the necessary studies and tests to clarify the diagnosis. Most often, such tests are prescribed to exclude the appearance of a malignant tumor.
Useful information about visiting a surgeon at the clinic:
- How to prepare for a surgeon's appointment
- What diseases does the surgeon treat?
- Calling a surgeon to your home
- Surgical care in the clinic
- Surgical care at home
- What symptoms should you contact a surgeon for?
- Treatment of surgical diseases
- Treatment of intestinal pathologies
- Treatment of skin surgical pathologies
- Treatment of bedsores and necrosis
- Treatment of parasitic diseases
- Treatment of inflammatory processes of soft tissues
- Treatment of diseases of the musculoskeletal system
- Diagnosis of surgical diseases
Diagnosis of wen
If you discover a suspicious growth on your neck, you should immediately consult a doctor and do not wait for the situation to worsen. The issue is dealt with by dermatologists, cosmetologists, therapists, oncologists and surgeons. At the first stage, the patient should consult a doctor and undergo a superficial examination. External diagnostics involves examination, palpation and determination of the size of the pathology. If the origin of the tumor is in doubt, the patient undergoes additional examination. This includes ultrasound, CT scan and biopsy. The latter makes it possible to determine the nature of the lipoma, since this phenomenon is easily confused with a cyst, atheroma, mastopathy and other subcutaneous pathologies.
To avoid mistakes, the sebaceous fluid located inside the tumor is sucked out using a syringe with a thin needle and sent for histological examination. By observing fat cells under a microscope, it becomes possible to establish an accurate diagnosis and determine the presence of cancer cells. In most cases, the surgeon advises removing the wen immediately, without waiting for it to become cancerous.
Diagnostics
An accurate diagnosis can be made by visual examination and palpation of the wen.
It is characterized by such signs as:
- No pain;
- Softness and mobility;
- Clear contours.
The extent of the spread of the formation in the tissues of the neck and the condition of the wen capsule can be assessed by ultrasound or computed tomography. To determine the composition of the wen, a biopsy is performed, sending the material for cyto- and histology. This tactic will help differentiate cervical lipoma from tumors with similar external signs.
Radical removal of lipomatous formation
Indications for removal:
- the wen reaches five centimeters in diameter;
- damage to the tumor by physical and chemical effects;
- the presence of inflammatory processes;
- neck discomfort and pain;
- pathology puts pressure on the larynx and interferes with breathing;
- change in lipoma skin color.
If the presence of a wen on the neck is not noticeable, the development of the pathology should be left under the supervision of the attending physician.
A common method of removal is surgery. The tumor is excised along with the capsule to avoid further relapse. Surgery is a budget option and lasts a maximum of 20 minutes. The only drawback is that after the operation a scar remains, which is smoothed out over time under the influence of ointments and creams. The postoperative period lasts two weeks. The patient should remain in bed and limit physical activity.
Laser removal is an innovative way to get rid of lipoma. This method is characterized by speed, efficiency and painlessness. Laser is actively used in cosmetology, as it eliminates the occurrence of inflammatory processes, scars, spots and scars after surgery. The risk of recurrence of a wen after the procedure is minimal. The operation is prohibited during pregnancy, breastfeeding, skin diseases, diabetes and herpes. The procedure lasts at least 15 minutes, after which the patient is free. The rehabilitation period lasts a couple of days.
The radio wave method is recommended for use at a late stage of lipoma development. The surgeon removes the pathology using a radio knife, excising the surface affected by lipomatosis. The operation occurs without bleeding, injury, pain and does not leave unwanted marks. This method is effectively used in surgery, cosmetology and dermatology. The procedure lasts a maximum of 25 minutes and does not require further hospital stay provided the patient is in normal health. It is strictly forbidden to use the radio wave method for people suffering from cardiovascular diseases, dysfunction of the hematopoietic system and skin inflammation. The method is contraindicated for people with sensitive skin and early stage lipomatosis.
The electrocoagulation method is used to remove small formations at an early stage of development. The contents of the lipoma are removed along with the capsule, which prevents the possibility of further relapse. This procedure is recommended for use in case of multiple lipomas on the face and in the cervical region. The procedure lasts no more than 15 minutes using painkillers. The advantages of electrocoagulation are that the operation does not cause pain, does not leave spots, scars or cicatrices and eliminates the recurrence of lipomatosis. It is strictly forbidden to perform surgery if a person suffers from allergies, subcutaneous infections, herpes, hypertension and flu.
Radio wave method for removing wen
In fact, removing a tumor using the radio wave method is the same surgical operation, only the tissue is cut not with a metal scalpel, but with a “radio knife”, which, while cutting the skin, simultaneously seals (coagulates) the capillaries. Thus, the cut is bloodless. Despite all the advantages of radio wave surgery, there are contraindications to its use:
- the diameter of the neoplasm is over 6 cm;
- acute infectious diseases;
- elevated temperature;
- diabetes mellitus, epilepsy;
- the presence of metal implants or a pacemaker.
Atheromas on the scalp are most susceptible to trauma followed by inflammation.
In this case, the radioknife is most effective. The operation is performed under local anesthesia in the same way as with a regular scalpel. If the size of the neoplasm does not exceed one centimeter, stitches do not need to be applied; in other cases, the wound is sutured. The advantage of this method is painless postoperative recovery, which is achieved through nerve coagulation.
Unconventional treatment
If the wen turns red and hurts, you can relieve inflammation using traditional methods. Herbal compresses made from yarrow, celandine, chamomile, watercress, Kalanchoe and hogweed are suitable. It is recommended to take herbal infusions orally to improve the effect. The course of treatment lasts no more than two months. It is advisable to make tinctures yourself.
Honey, egg yolk, alcohol, pepper and aloe juice are also used as a compress. Raw potatoes are suitable for relieving inflammation and redness of lipoma. Aloe leaf slows down the growth of pathology and removes pain in the affected area. A compress of chopped onions can reduce the size of the growth and stop the pain symptoms. For quick results, it is recommended to apply compresses daily and change the gauze bandage three times a day.
It is important to note that it is impossible to cure lipoma on your own at home. The use of an unconventional remedy is acceptable if the wen is inflamed and causes pain. Treatment of wen should be carried out comprehensively: with the help of folk remedies and medications.
Treatment
How to remove a wen from a child? In what ways does this happen? If necessary, only a qualified specialist can fix the problem.
There are different cases of lipoma formation and, accordingly, different treatment is provided for each of them. Let's look at typical cases of lipomas in children.
If a wen is on the face of an infant - how to get rid of it? In babies under one year of age, they look like pimples, white on the inside. Most often they can be seen on the baby's nose or on the child's eyelid. Such formation is usually provoked by a hormonal disorder and after some time disappears on its own. Under no circumstances should the integrity of this pimple be violated. It is prohibited to influence such a lipoma in any way. It cannot be squeezed out, pierced, etc.
The baby must make an appointment with a dermatovenerologist. If necessary, he will prescribe an appropriate course of treatment.
If the formation is located in the occipital region and is subcutaneous, only a surgeon can remove it. The same can be said about lipoma, which is located in the chest area. Surgery is also needed here. If the formation occurs on the chest, it is especially important to eliminate it in girls. In the future, the wen can interfere with the normal development of the mammary glands.
If a wen is detected in a child, treatment can also be conservative. This is practiced when the patient is still quite young in age, and the tumor has just appeared. This type of treatment is carried out therapeutically, using medications. May be assigned:
- special medicinal ointments;
- a special diet in which you should eat foods with a high content of fiber and nutrients.
Conservative treatment is also indicated after the tumor has been surgically removed. It can be prescribed for prophylactic purposes to avoid relapse of the tumor.
Preventive measures
The understanding of the causes of subcutaneous neoplasm remains vague, so it is impossible to accurately determine measures to prevent the disease. Doctors are of the opinion that disorders of lipid metabolism of the skin, diseases of the digestive system and failure to comply with hygiene rules are possible causes of the disease.
Dermatologists advise sticking to a healthy lifestyle, eliminating junk food from your diet, adding exercise to your daily routine, and regularly caring for your skin using pharmaceutical and cosmetic products. Annual scheduled examinations and regular visits to a dermatologist, cosmetologist and therapist will protect a person from the occurrence of painful lipomas.
Causes of atheroma in children
Atheromas in children occur due to a violation of the secretion of sebum by the corresponding glands.
When the excretory duct is blocked, the secretion of the gland has nowhere to go. It is secreted into the subcutaneous space, where a dense capsule is formed around it. Common causes of atheroma development in children are as follows:
- Using children's cosmetics (creams, ointments, moisturizing masks) in excessive quantities. Sometimes parents, in an effort to protect their child’s skin from harmful external factors, use cosmetic products uncontrollably. This leads to dysfunction of the sebaceous glands with blockage of their excretory ducts.
- Hormonal changes in the child's body. Infants and teenage children are traditionally at risk. It is during these periods that changes in the concentration of sex hormones occur. Against this background, acne appears, the function of the sebaceous glands is disrupted, and conditions are created for their blockage.
- Seborrhea. This is a dermatological disease that leads to dysfunction of the sebaceous glands in a certain area of the skin.
- Genetic predisposition or congenital structural features of the skin. Atheromas most often occur in children after 3 years of age. If neoplasms are detected in children immediately after birth, the doctor may assume the presence of problems with the sebaceous glands that developed in utero.
In addition, factors that increase the risk of developing atheromas are poor personal hygiene, metabolic disorders (obesity, diabetes) and frequent mechanical damage to the skin.
Indications and contraindications for surgical removal of lipoma
Important!
Although a lipoma is not cancerous and does not cause pain, we recommend seeking medical attention at the first sign of its appearance.
Removal of the wen is mandatory in the following cases:
- The lipoma begins to quickly increase in size.
- If, after an injury, the skin over the wen begins to redden and itch.
- If the neoplasm is a serious visual defect.
- If discharge occurs from the wen.
- If the lipoma reaches a size of more than 4 cm.
- If the neoplasm compresses nearby vessels and nerves.
- If there is a suspicion of malignancy.
- When the wen sag (the appearance of the so-called “pedunculated lipoma”).
Contraindications to surgery to eliminate lipoma are:
- The presence of acute infectious diseases.
- Decompensation of diabetes mellitus.
- Pathologies of the cardiovascular system.
- Exacerbation of chronic diseases.
- Presence of allergic reactions.
- Heat.
The operation must also be rescheduled during pregnancy and breastfeeding. Women are also advised to schedule surgery after the end of menstruation.
Important!
Most contraindications to removing a wen are relative and require only postponing the operation, and not canceling it.
Preparing for the intervention
Before the intervention, the patient is prescribed a series of tests that must be completed. This is necessary so that the doctors of our center can choose the optimal treatment method, determine the presence of contraindications and be able to prevent complications. This is especially important in cases where the removal is performed on a child.
The standard research package includes
- General laboratory blood test.
- Coagulogram to determine blood clotting and estimate bleeding time.
- Checking blood glucose levels.
- Test for infectious diseases (HIV, syphilis, etc.).
In order to accurately determine the location of the lipoma, its size, as well as the characteristics of the blood supply, an ultrasound examination is prescribed. If the pathology is old and located in a critically dangerous area (for example, in the temporal region), MRI and CT are also prescribed.
Important!
You can get all the necessary types of diagnostics at a medical center at affordable prices.
Another important stage of preparation is consultation with an anesthesiologist. The doctor will help you choose the optimal type of pain relief and dosage of the substance. To obtain accurate data, the results of a general urine test and ECG are necessary.
Important!
After surgery, it is recommended to conduct a histological analysis of the removed tissue. Based on its results, the doctor can detect the presence of certain diseases, including cancer.
Diagnosis of atheroma in children
It is relatively easy to identify atheroma.
Even at the stage of the initial conversation with the patient or his parents, the surgeon assesses the general well-being of the child, collects anamnesis and analyzes complaints. When examining a neoplasm, the doctor pays attention to its size, location, pain, and the presence of redness. Before surgery, the surgeon prescribes a number of tests to comprehensively assess the child’s condition:
- general and biochemical blood test;
- general urine analysis;
- blood test for infections (HIV, syphilis, viral hepatitis B, C);
- ECG, fluorography.
The child is also examined by an anesthesiologist and pediatrician before the operation. A mandatory diagnostic method is histological examination of tumor tissue after its removal. At this stage, it is possible to determine whether it was an atheroma or a lipoma (a tumor similar in appearance).
Questions
- Which doctor treats atheroma in children?
A pediatric surgeon is involved in identifying and treating atheroma in children. - Is it possible to cure atheroma without surgery?
Sometimes in the early stages of the disease the surgeon chooses a wait-and-see approach. In 20-35% of cases, atheroma can resolve on its own. However, if the capsule is formed and the tumor is large, it will not be possible to do without surgical intervention. - How dangerous is atheroma in childhood?
Atheroma is a relatively safe tumor. It does not become malignant, rarely becomes complicated and is not accompanied by the development of permanent defects. However, this does not eliminate the need to consult a pediatric surgeon. Only a doctor can establish the correct diagnosis and select treatment. In addition, atheroma can sometimes become inflamed due to the addition of bacterial flora and cause a deterioration in the child’s well-being. - Is it possible to play sports after surgery?
After surgical removal of atheroma, it is recommended to refrain from active activities for 2-3 weeks. This will allow the tissues to fully heal and recover.