Today, the question of the possibilities of scar correction is relevant for both dermatocosmetologists and surgeons. It is extremely important to understand the stage of scarring and prescribe therapy based on the “age” of the scar tissue.
As a rule, if a skin injury occurs only in the epidermis layer, then during healing there are practically no traces, due to the ability of the cells of the basal layer of the epidermis to regenerate throughout life. Damage to the deeper layers of the skin is filled with granulation tissue, which is further transformed into a scar. Gradually, the scar tissue flattens and takes on the color of the surrounding tissues, that is, it becomes a normotrophic scar. In some cases, this process is disrupted, leading to the formation of pathological scar tissue.
Material and methods
At the first stage of our study, 43 women aged 15 to 27 years with established diagnoses of acne and acne complicated by atrophic scars were observed. All patients, depending on the clinical picture, were divided into two comparable groups: group A included 22 patients (acne complicated by atrophic scars) and group B - 21 (acne). All patients underwent buccal scraping with sterile cotton swabs to collect material for analysis, followed by a genetic study of the frequency distribution of gene polymorphisms ESR1, Col1A1, Col1A2, Col3A1, Col5A1, MMP1, MMP12, MMP2, MMP3, MMP7
.
The study results were assessed on a 3-point scale:
1 — homozygote frequent allele (norm/norm), which corresponds to the absence of an increased risk of developing the trait under study (average population risk);
2 - heterozygote (normal/mutation), which corresponds to a moderate risk of developing the trait under study;
3 - homozygous rare allele (mutation/mutation), which corresponds to a significant risk of developing the trait under study (the gene for this trait is a risk factor for the disease).
At stage II of the study, 50 patients were observed - 28 (56%) men and 22 (44%) women with severe acne, whose average age was 15.7 ± 1.4 years. As the main treatment, participants received a systemic retinoid (isotretinoin) in standard dosages (initial dose - 0.7-0.8 mg/kg/day, followed by a dose reduction to 0.4-0.5 mg/kg/day, course duration at least 6 months). After achieving IGA 0-1, patients with atrophic post-acne scars were divided into two groups: group 1 included 24 patients, group 2 - 26. Patients of group 1, after completing the course of treatment with isotretinoin, used the drug externally with a fixed combination of 0 .1% adapalene/2.5% benzoyl peroxide once a day for 6 months. Patients of group 2 did not receive any treatment. The clinical picture in patients of groups 1 and 2 was represented by atrophic scars, post-inflammatory pigmentation and foci of congestive erythema. The effectiveness was assessed taking into account the number of primary elements of acne and atrophic post-acne scars (5-point system of severity for each element of the rash on a visual analogue scale), as well as an overall assessment of the severity of scars (Scar Global Assessment - SGA).
Prevention of scarring
To prevent the appearance of skin defects on the face and body, dermatologists recommend following certain recommendations. This will minimize the factors that provoke the appearance of scars:
- Rejection of bad habits. Nicotine and alcohol negatively affect the condition of the skin. Its healing is more difficult, inflammation occurs. And in their place remain hypertrophic and atrophic scars.
- Proper nutrition. Include vegetables, fruits, lean meat, and fish in your diet. Avoid starchy, spicy and sweet foods.
- Walking in the fresh air improves blood circulation and, accordingly, stimulates the natural saturation of the skin with oxygen and nutrients.
- Fluctuations in body weight cause negative processes in the structure of the skin. The risk of scarring increases.
- Skin care with hyaluronic acid-based cosmetics helps keep it in good condition.
We invite you to contact our dermatologists to find out more about scar treatment at the Lasersvit Medical Center for Mole Diagnostics in Kharkov. We will be happy to answer your questions and provide competent advice.
Results and discussion
During the comparative analysis of the first stage of the study of gene polymorphisms, a statistically significant difference in the distribution of alleles of the genes Col1A2, MMP3, ESR1, MMP1, MMP7
between the two groups of patients (Fig. 3).
Rice.
3. Average code value of alleles of genes Col1A2, MMP3, ESR1, MMP1, MMP7 in groups A and B. Group A (22 patients diagnosed with acne complicated by atrophic scars):
- Col1A2
— allele code 3 was determined in 17 (77.2%) patients, allele code 2 in 3 (13.6%), allele code 1 in 2 (9.1%);
- MMP3
- allele code 3 was determined in 19 (86.4%) patients, allele code 2 - in 2 (9.1%), allele code 1 - in 1 (4.5%);
— ESR1
- allele code 3 was determined in 8 (36.3%) patients, allele code 2 - in 12 (54.5%), allele code 1 - in 2 (9.1%);
- MMP1
- allele code 3 was determined in 6 (27.2%) patients, allele code 2 - in 14 (63.6%), allele code 1 - in 2 (9.1%);
- MMP7
- allele code 3 was determined in 8 (36.3%) patients, allele code 2 - in 13 (59.1%), allele code 1 - in 1 (4.5%).
Group B (21 patients diagnosed with acne):
- Col1A2
— allele code 3 was determined in 2 (9.5%) patients, allele code 2 in 3 (14.2%), allele code 1 in 16 (76.1%);
- MMP3
- allele code 3 was determined in 5 (23.8%) patients, allele code 2 - in 7 (33.3%), allele code 1 - in 9 (42.8%)
— ESR1
- allele code 3 was determined in 1 (4.7%) patient, allele code 2 - in 2 (9.5%), allele code 1 - in 18 (85.7%);
- MMP1
— allele code 3 was determined in 6 (28.5%) patients, allele code 2 in 5 (23.8%), allele code 1 in 10 (47.6%);
- MMP7
— allele code 3 was determined in 2 (9.5%) patients, allele code 2 in 4 (19.1%), allele code 1 in 15 (71.4%).
Moreover, in patients of group A, the average value of the allele code of the Col1A2
was 2.8 ± 0.1 (
p
< 0.01),
MMP3
- 2.9 ± 0.1 (
p
< 0.01),
ESR1
- 2.1 ± 0.1 (
p
< 0.01 ),
MMP1
- 2.3±0.1 (
p
<0.01),
MMP7
- 2.0±0.1 (
p
<0.01).
In patients from group B, the average allele code of the Col1A2
was 1.3±0.1 (
p
<0.01),
MMP3
- 1.6±0.1 (
p
<0.01),
ESR1
- 1.2±0.1 (
p
<0.01 ),
MMP1
- 1.5±0.1 (
p
<0.01),
MMP7
- 1.4±0.1 (
p
<0.01).
Accordingly, in group A there was a high value of the allele code of the genes Col1A2, MMP3
, the average code value of the alleles of the genes
ESR1, MMP1, MMP7
, at the same time, low values of the alleles of the same genes in group B are shown. At the same time, when analyzing polymorphisms of the
Col1A1, Col3A1, Col5A1, MMP12, MMP2
, no statistically significant difference in the distribution of alleles was revealed of these genes between the study groups of patients. Thus, based on the results of the study, it can be assumed that there are certain genetic predictors of the formation of atrophic post-acne scars.
At stage II of the study, the preventive and therapeutic effectiveness of a fixed combination of 0.1% adapalene/2.5% benzoyl peroxide in patients with post-acne was assessed.
In group 1, during the use of a fixed combination, not a single clinical case showed a relapse of the disease, which indicates the preventive nature of the drug. With regard to post-acne symptoms, a pronounced positive trend was observed: post-inflammatory erythema decreased by 85%, pigmentation resolved by 70%, the morphological structure of scars, their relief and number decreased by 56.1% (largely due to scars of mild and moderate severity) ( Fig. 4).
Rice. 4. General assessment of the clinical symptoms of acne and post-acne at baseline, after 3 and 6 months in patients of group 1.
In group 2, by the 3rd month, 15.4% of patients noted the appearance of new single inflammatory elements (papules, pustules). Significant changes in post-inflammatory erythema and pigmentation were observed only by the 6th month, but the severity of these symptoms decreased only by 35 and 24%, respectively. The morphological structure of the scars and their relief did not tend to improve; moreover, scars continued to form at the sites of new rashes, and their total number increased (Fig. 5).
Rice. 5. General assessment of the clinical symptoms of acne and post-acne at baseline, after 3 and 6 months in patients of group 2.
A general assessment of the severity of atrophic acne scars was carried out taking into account the SGA scale. After 3 months of using a fixed combination of 0.1% adapalene/2.5% benzoyl peroxide, the number of patients with clear skin increased 2-fold, and the quality characteristics and relief of scar deformities of moderately severe scars improved 1.5-fold. After 6 months, in group 1, the number of patients with an SGA score of “almost clear skin” increased 7-fold, while in group 2 there was no positive dynamics after 3 and 6 months. Thus, the fixed combination of 0.1% adapalene/2.5% benzoyl peroxide has a certain preventive effect regarding the formation of atrophic scars, which was confirmed by the absence of new secondary elements, while the proportion of patients with an SGA rating of “almost clear skin” (barely noticeable scars ) increased from 6.4 to 46.7% when using the combination drug and did not change in the control group (Fig. 6).
Rice. 6. General assessment of the severity of scars, taking into account the indicators of the SGA scale at baseline, after 3 and 6 months in patients of both groups.
Causes of scars
Deep keloid scars are a consequence of atrophy or incomplete regeneration of skin tissue after damage. The tissue defect is covered by granulation tissues that form a scar. Their structure is denser than healthy skin, therefore they stand out visually and tactilely on the surface of the skin.
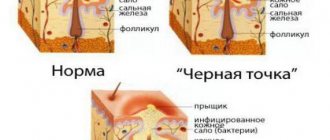
Important: Atrophic scars may appear after acne, after chickenpox in a child, at the site of skin inflammation (teenage acne), cuts, burns.
Video:
Laser scar modeling with a fractional erbium laser (laser dermabrasion). The procedure removes scars, “craters” of pores on the skin, and any consequences of post-acne. It is performed under anesthesia; the age of the scars does not matter.
Maria's review:
“When I was young, I suffered a lot from acne. They passed, but by the age of 25 my face had turned into one endless scar. Without exaggeration, white and red scars were piled one on top of the other.
Those who know will understand: even just to leave the house you need to carefully apply concealer, foundation and powder, but as a result you look no better than a young old woman.
There is no quick way to remove acne scars. Unlike acne, they do not go away on their own. Dealing with scars turned out to be more difficult than acne. I burned them out with chemical peels and with a laser - it helped, but I was not able to completely get rid of acne scars.
What I have after a year and a half of treatment with Vasilyev Maxim is very similar to a miracle - there are almost no signs of acne visible, the skin is smooth and beautiful.
How much patience a doctor must have who works for so long with such jeweler precision and brings the work to perfection. Thank you"!
Just getting rid of acne scars on your face is not enough. Removing red spots
The first thing we offer after working with scars is a course of biorevitalization with 3% hyaluronic acid. This procedure very well lightens stagnant spots and evens out skin tone.
Finally, after six months or even a year, the time for the laser comes. The fact that we raised the bottom of the scar almost to the level of healthy skin will save it from aggressive resurfacing. Surface or medium grinding will be sufficient.
Please note that it is not the scar that is polished, but the skin surrounding it: as a result, it partially lowers to the level of the scar. The skin is evened out.
How to remove acne scars on face 100%
Despite the fact that subcision itself shows good results in the fight against scars, it does not provide a 100% effect of smoothing the skin. Removing an acne scar by cutting it is only the first stage.
The second stage is the introduction of a drop of collagen or stabilized hyaluronic acid into the lacuna formed under the crater.
Initially, the injected drug creates the necessary volume and physically “pushes” the scar area to the skin level. Within 6 months, the gel is removed and replaced with its own collagen. Collagen fills the area of the lacuna and takes on the function of maintaining the required volume.
As a result, the craters are significantly leveled with the healthy surface of the skin.