October 25, 2020
These are completely different diseases and it is possible to distinguish them from each other, although not always easy. The addition of signs of eczema and infection to skin rashes makes diagnosis even more difficult.
People already suffering from one of these ailments know the difference between neurodermatitis and psoriasis and will not confuse their manifestations during exacerbation. When a skin lesion is first noticed, the following facts must be considered:
- after which rashes appeared on the skin;
- is there itching and peeling, how strong are they;
- in what places of the body did they appear: hands, neck, skin folds, head and others;
- the presence of such manifestations in relatives;
- combination of skin disease with allergic rhinitis, bronchial asthma, frequent urticaria.
A careful examination of the rash itself will provide a lot of information.
Causes of genital psoriasis and risk factors
Scientists from around the world continue to put forward hypotheses regarding the causes of psoriasis, including genital psoriasis. It should be noted that none of the assumptions made has yet been 100% confirmed. However, based on a combination of factors, experts conclude that the main role in the development of this pathology is played by an autoimmune disorder, when one’s own immune cells fight not against foreign agents, but against their own cells.
IMPORTANT! Genital psoriasis is not an infectious or viral disease. This is a dermatological problem caused by autoimmune processes. Therefore, it is impossible to become infected through sexual contact, blood transfusions, or at home.
Possible provoking factors causing genital psoriasis include:
- changes at the hormonal level (the likelihood of exacerbations increases during puberty, pre- and postmenopause, as a result of taking hormonal drugs);
- state of stress, increased nervous or physical stress;
- damage to the mucous membranes or skin in the intimate area;
- decreased immunity due to exacerbation of existing chronic diseases;
- hypothermia or prolonged exposure to damp underwear;
- allergic reactions to food, intoxication due to alcohol or medications;
- change of place of residence, moving to another climate zone;
- overweight.
Prevention of psoriasis in the groin
Prevention measures can seriously delay relapses and alleviate the patient's condition immediately during an attack of the rash.
The following rules should be followed:
- Monitor your psycho-emotional state. One of the key factors. It is important to limit any stress and anxiety, and also try to always maintain a positive attitude. Negative emotions can provoke an exacerbation of the disease.
- Wear the right clothes. Underwear should not be tight or made of synthetic materials. The latter do not allow the skin to “breathe” and cause increased sweating.
- Control your diet. It is worth excluding or limiting spicy, salty and fried foods, as well as everything fatty, smoked and sweet. It doesn't hurt to remove potential allergens from your diet. These include citrus fruits, chocolate and coffee, nuts, all bee products, and eggs.
- Maintain a healthy lifestyle. It is important not only to give up cigarettes and alcohol, but also to follow the regime. Walking in the fresh air, moderate exercise and a daily routine will be beneficial.
- Rest. People with psoriasis need a moderate work schedule and adequate sleep. A visit to a sanatorium or a simple vacation at sea will also be beneficial. This will strengthen the immune system and improve the condition of the nervous system.
Compliance with the recommendations is the key to a comfortable life and the absence of frequent relapses.
Diagnosis of genital psoriasis or psoriasis on the genitals
Psoriasis on the labia in women and on the head of the penis in men is not a separate disease. This is just one of the areas where the rash may be located. The problem can be localized in other parts of the body, most often the knees, elbows, abdomen, chest, back, buttocks, scalp, and in this case diagnosis is not difficult. Only genital rashes are rare, but cause more concern due to complex diagnostics, and often such patients are prescribed many tests to exclude infectious and allergic diseases.
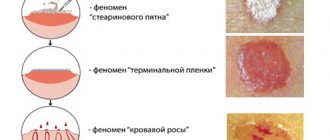
Psoriasis of any localization, including genital psoriasis, is characterized by the psoriatic triad:
- The “stearin stain” phenomenon.
- The phenomenon of “terminal film”.
- The phenomenon of "bloody dew".
Fig.1
If the psoriatic triad is doubtful, the doctor may suggest a histological examination.
Diagnosis
If even single and minor rashes appear in the groin area, you should immediately seek qualified medical help. The doctor will conduct an examination and refer you for examination to clarify the diagnosis.
For diagnostics of psoriasis the following is carried out:
- blood analysis;
- dermatoscopy is a visual assessment using a special device - a dermatoscope;
- taking samples of the epidermis of the affected areas of the skin.
It should be remembered that all assumptions and diagnoses from numerous doctors and specialists must be confirmed by the results of laboratory tests.
Self-diagnosis using medical literary sources, photos and information from the Internet is impossible. It is the diagnostic stage that predetermines all further treatment: it determines the stage and form of the disease.
Characteristic signs of psoriasis on the genitals
A patient with psoriasis on the genitals complains of suspicious rashes.
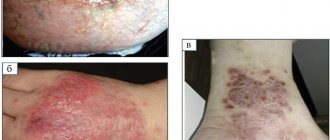
Regardless of the location, most psoriatic rashes appear as a cluster of rich pink or red papules, the top of which is covered with white scales.
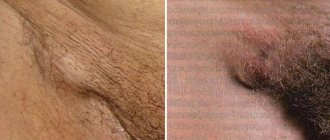
Genital psoriasis in women is predominantly associated with hormonal changes in the body that occur during puberty, pregnancy and the onset of menopause. A rash with psoriasis in women appears on the skin of the labia majora, in the pubic area, and inguinal folds. Sometimes psoriasis affects the mucous membranes of the labia minora. The disease can be recognized by the characteristic features of the rash: papules usually have a clear oval or circle shape, their boundaries are clearly visible, covered with scales on top, itching is almost always absent. Even though there are lesions in other parts of the body, women usually do not perceive this disease as psoriasis. Representatives of the fairer sex more often identify rashes as a manifestation of gynecological infections.
In men, genital psoriasis primarily affects the penis and head of the penis; the rash can also be located in the folds and pubic area. Usually the rashes are pink or red papules, slightly protruding above the surface of the skin, having smooth borders and covered with scales on top. Peeling and itching are usually absent. In advanced situations, the rash spreads to the inner surface of the skin covering the penis. Such phenomena cause particular discomfort among representatives of the stronger sex.
When a man or woman is diagnosed with genital psoriasis, treatment should not be delayed. Since this area is subject to mechanical friction, the skin in the groin area can become even more traumatized, its surface will begin to crack, which leads to the spread of rashes and damage to an increasingly larger area.
IMPORTANT! Psoriasis on the genitals threatens the normal sexual life of men and women. This, in turn, can trigger neuropsychiatric disorders, which will require more serious correction, so treatment should be started in a timely manner.
Lichen sclerosus
Lichen sclerosus of the penis, also known as balanitis obliterans, can occur at any age. The average age of patients at diagnosis is 42 years, and the incidence is 1 in 300 men. In 4–6% of patients, lichen sclerosus is associated with the development of squamous cell carcinoma. Genital lichen sclerosus is considered a precancerous condition.
Lichen sclerosus appears as a hypopigmented lesion with a surface resembling wrinkled paper or cellophane. It mainly affects the glans penis and foreskin. There may be visible blisters, erosions and skin atrophy. Patients usually have phimosis, painful erections, difficulty urinating, itching, pain and bleeding.
Photo 1. Lichen sclerosus
Photo 2. Lichen sclerosus
Because skin lesions can obstruct the urethra, the first symptom in patients may be urinary retention. Although lichen sclerosus can affect almost any part of the body, some people may have no symptoms. It must be differentiated from carcinoma in situ, leukoplakia, and systemic sclerosis. If squamous cell carcinoma cannot be ruled out, a biopsy is indicated.
- In the treatment of lichen sclerosis, topical fluorinated glucocorticoids with moderate to very high potency are usually used to reduce symptoms and prevent malignant transformation.
- With very high efficacy, GCS pulse therapy is effective and safer than long-term daily use of weaker GCS.
- Tacrolimus or pimecrolimus may also be effective, but their safety for long-term use has not been established.
Surgery is indicated for persistent lesions or if there is clinical suspicion that changes in the penis may be squamous cell carcinoma. In uncircumcised patients with lichen sclerosus limited to the glans and foreskin, removal of the foreskin (circumcision) may be indicated. For severe lesions, reconstructive surgery may be required, although if the risks of surgery outweigh the potential benefits, conservative treatment may be appropriate.
Systemic medications such as retinoids and methotrexate are indicated for the treatment of severe lichen sclerosus or when topical treatments are ineffective. Long-term follow-up with periodic physical examination is necessary to monitor the patient for malignant transformation.
Treatment of genital psoriasis in men and women
Treatment regimens for genital psoriasis differ from generally accepted methods for eliminating rashes on other parts of the body. The difference is that the genitals have special sensitive areas with mucous membranes; the effect in this area must be especially delicate and careful.
As a rule, for genital psoriasis, complex treatment is prescribed. The optimal therapy should be selected by the doctor, based on medical history, the general condition of the patient, and his individual characteristics. The principles of treatment depend on the degree of the disease and the severity of symptoms.
Typically, a regimen of external therapy for genital psoriasis or psoriasis on the genital organs involves prescribing the following groups of drugs:
- hormonal drugs - such drugs help relieve inflammation and reduce rashes, but they are not recommended for long-term use;
- non-hormonal agents based on activated zinc pyrithione;
- softening and caring components - they help moisturize the skin in the delicate area, eliminate signs of peeling, and restore the natural lipid barrier.
External hormonal preparations should be used with caution, because the surface of the genitals is highly absorbable.
Anatomical differences in absorption (% of the total absorbed dose from the entire
body surface area) are:
- Plantar surface of the foot - 0.14%;
- Palmar surface - 0.83%;
- Forearm - 1.0%;
- Scalp - 3.5%;
- Forehead - 6.0%;
- Lower jaw area - 13%;
- The surface of the genitals is 42%.
The use of external hormones inhibits local immunity, which enhances the growth of fungal flora. After a course of therapy, it is important to gradually reduce the use of hormonal drugs to avoid withdrawal syndrome.
Preparations with the irritating effect of tar and petroleum derivatives are not recommended for use in psoriasis on sensitive areas and genitals, as they have side effects such as severe skin irritation (including burns), persistent discoloration of the skin, increased sensitivity of the skin to the sun (phototoxicity) , frequent cases of allergies. Also, these groups of drugs are characterized by low compliance due to an unpleasant odor.
Many specialists prefer to treat genital psoriasis with non-hormonal Skin-cap cream. Skin-cap cream contains activated zinc pyrithione, which has a pronounced anti-inflammatory property and antipruritic effect. Additionally, the formula of the drugs includes moisturizing components. Skin-cap cream can also be used to prevent progression, for example, to avoid the appearance of psoriasis rashes on the pubis after depilation or shaving.
Classification and examples of local GCS
| Group | Power of action | Examples |
| 1 | very strong | clobetasol 0.05% |
| 2 | strong | betamethasone ointment 0.05% |
| 3 | strong | triamcinolone ointment 0.1% |
| 4 | average | hydrocortisone 0.2% |
| 5 | average | triamcinolone cream 0.1% |
| 6 | small | betamethasone lotion 0.02% |
| GCS - glucocorticosteroids | ||
Additional Relapse Prevention Recommendations
Psoriasis on the genitals cannot be completely cured, but you can take control of this disease and reduce the likelihood of exacerbations. To do this, it is necessary not only to undergo timely medical examinations and follow doctors’ recommendations, but also to reconsider your lifestyle. Here are some recommendations to reduce the likelihood of relapses of genital psoriasis:
- review the diet, exclude foods that cause aggravation;
- provide high-quality and regular skin care in the intimate area;
- exclude traumatic procedures (epilation, shaving, aggressive peelings in the bikini area);
- give preference to linen made from natural soft fabrics (cotton is ideal);
- try to avoid stress, balance activity and rest.
With an integrated approach to prevention and treatment, genital psoriasis can be kept under control, thereby increasing the quality of life of patients.
Fig.1. Psoriatic triad
Rice. 2. Psoriasis on the penis
Therapeutic options for non-infectious penile lesions
| Diagnostics | The main method of struggle | Alternative Methods |
| Papular and scaly changes | ||
| Psoriasis | local GKS | vitamin D analogues 3, tacrolimus, pimecrolimus |
| Inflammatory changes | ||
| Lichen sclerosus | local GKS | circumcision for lesions limited to the foreskin |
| Ringworm | observation | topical corticosteroids, tacrolimus, pimecrolimus |
| Lichen planus | local GKS | circumcision for lesions limited to the foreskin |
| Vascular changes | ||
| Angiokeratoma | observation | surgery, cryoablation, electrocoagulation, laser ablation |
| Tumor changes | ||
| Cancer is in place | circumcision for lesions limited to the foreskin | Mohs microsurgery technique, topical imiquimod |
| Invasive squamous cell carcinoma | circumcision for lesions is limited to the foreskin; Mohs microsurgical technique for non-isolated lesions | partial or radical removal of the penis, radiation therapy, brachytherapy |
University
— Alexander Mikhailovich, I have been suffering from psoriasis for 10 years. Can it be cured permanently?
— Do your relatives have psoriasis?
- On the paternal side there is.
— During these 10 years, how many exacerbations have you had?
— Usually in winter and spring.
- How are you being treated?
— I mainly use ointments containing salicylic acid and vitamins.
— Psoriasis is a disease, the predisposition to which is transmitted genetically, occurs chronically and has a wide variety of manifestations. Most often, the skin and its appendages (nail plates) are involved in the process. Sometimes we see the systemic nature of lesions in psoriasis, when, for example, the clinical picture of psoriatic arthritis develops. Unfortunately, at the moment medicine does not have a universal remedy that could help everyone at once. Giving practical recommendations over the phone without seeing the patient is not an easy task; telephone consultation can in no way replace communication with the attending physician for a number of reasons, the most important of which are: an objective assessment of anamnestic, clinical, laboratory data in each specific case. If you have only used salicylic acid-based ointments, then I can tell you that you have not used the entire arsenal of modern medicine. It should be understood that there are general rules for the treatment of psoriasis. It is believed that if the pathological process affects no more than 3 - 5% of the skin, then the course of psoriasis is regarded as mild. In this case, you should limit yourself to using exclusively local medications: creams, ointments, emulsions containing corticosteroids, vitamin D3 analogues, tar, anthralin, topical retinoids, etc.
If up to 10% of the skin is involved in the process (moderate psoriasis), it is recommended to consider the use of selective phototherapy, more often narrow-band (with a wavelength of 311 - 313 nm). The latter is considered the most effective and relatively safe. Currently, all regions of the country have installations for its implementation. In cases of severe psoriasis, phototherapy can be general in nature, with irradiation of large surfaces of the skin. If the process cannot be stabilized, the issue of prescribing systemic therapy, using antimetabolites, cytostatics, and systemic retinoids, is considered. If systemic therapy is ineffective, as well as in cases of initially malignant forms of psoriasis, it is possible to use a new group - genetically engineered biological drugs. It should be remembered that self-medication is dangerous and, I would say, emphasizes the patient's lack of respect for himself. Only a dermatologist can correctly assess your condition and the adequacy of your response to the prescribed therapy.
If one ointment doesn't help you, that's okay. You need to consult a specialist and select adequate treatment. Be patient. Psoriasis is not a stigma, it is a disease that you can and should live well with, and the quality of life of patients with psoriasis should be exactly the same as that of healthy people. And this depends not only on the doctors, but also on you.
TREATMENT SCHEME FOR PSORIASIS IS DETERMINED ONLY INDIVIDUALLY
— Is there an effective cure for psoriasis in Belarus?
— Today in Belarus there are all the necessary drugs for the treatment of psoriasis. But there is no panacea. In order to choose the medicine that is right for you, I need to ask you many questions. How did the disease begin, how long did it last, how was it treated, what was the result of the treatment? Look at the condition of your skin.
“I’ve had psoriasis for forty years now. Only the sun can save you. Ointments don't help. They say you need to take something internally.
— What ointments do you use?
- Salicylic acid, folk...
— How do you assess your condition?
- It doesn’t itch or hurt me. But I’m embarrassed to go to the beach - my knees and elbows are affected.
- As I understand it, you now only have emergency plaques. Do not try to remove them by any means, sometimes this can lead to a completely opposite, negative effect. Irrational aggressive local therapy is the cause of the complicated course of psoriasis. It is best to contact the nearest dermatovenous dispensary, where the doctor will competently select the necessary therapy, which should be carefully followed. Most often, psoriasis is very dependent on a person’s behavior and bad habits. You just need to learn how to care for him.
— My husband is 57 years old, and he has had psoriasis for 10 years. In recent years, the disease has spread throughout the body. He complies with all the treatment prescribed. But after ointments, the spots become red and inflamed.
“The fact is that the ointment base creates a film on the skin, which disrupts the processes of skin respiration, the blood vessels dilate, and the patient gets the impression that the element is becoming even redder. Hormonal ointments, whose effect is precisely to constrict blood vessels, in most cases relieve this redness.
— Maybe you can suggest something effective?
— Consulting a patient with a skin disease over the phone is very dangerous. You should contact the skin and vein clinic in your area, where you can get qualified help. If necessary, you will be referred for consultation to employees of specialized departments of medical universities in the country, State Educational Institution BelMAPO. Don't hesitate to ask for help. Currently, more than 100 treatment methods have been proposed, but none of them are ideal or 100% effective. Therefore, in each case the problem is solved individually.
— Is it supposed to be like that when the skin peels?
— The primary rash in psoriasis is a nodular element of bright red color, which is covered with silvery scales. Therefore, peeling is one of the most consistent clinical characteristics of psoriasis.
— Does my husband need a special diet?
- Is yours full?
- No, he’s skinny, he smokes all the time.
— For patients with psoriasis, smoking is especially undesirable. A person who smokes deprives tissues of oxygen, which is needed to normalize processes, including those affecting the development of psoriasis. Regarding the diet. If there are no problems with gaining excess weight, then no special recommendations need to be followed.
- One more question. He uses hormonal ointments twice a day - morning and evening. This is right?
— All hormonal products should be used only for a certain time; you cannot accustom your skin to hormones; you need to take breaks. If you use a hormonal drug for a long time and often, psoriasis over time becomes insensitive to topical therapy. In addition, side effects of using local hormones develop. Therefore, you should not use topical corticosteroids for more than 10 to 14 days. It is better to use hormonal drugs once a day - in the morning. You should also know that not all hormonal agents have the same activity, and this, in turn, dictates special rules for their use not only in terms of duration and frequency of application, but also, for example, in the place of their application (face, torso, large folds and etc.). There are many nuances that only your treating dermatologist can help you understand.
— Is it worth taking baths with sea salt?
- It is very useful. And it’s very good if you can go to the sea, to the sun.
THE TENDENCY TO PSORIASIS IS INHERITED
— My granddaughter is 18 years old, psoriasis was discovered six months ago. In our family, only her great-grandfather had this disease.
— Psoriasis is a disease that is associated with genetics. But it is not the disease itself that is transmitted, but the tendency to it. And the reasons that trigger disease genes can be very different: stress, infections, medications, etc. That is why each patient must have an individual approach. In Belarus, 4.5% of the population suffers from psoriasis. Here we are almost at the level of Norway and Sweden, where the percentage is the highest (about 6%).
— I have a question about childhood psoriasis. My daughter is 10 years old and has had psoriasis since she was 5 years old. Then we even ended up in the hospital with psoriatic erythroderma.
- And this happens, unfortunately...
“After treatment, she ended up in intensive care. Fortunately, we made it out. Psoriasis, of course, did not go away. We try to contain it, but only with folk remedies. I keep her on a strict diet, and every summer and autumn we go to the sea.
— Do you use any ointments or creams?
- Nothing. Any impact causes an aggravation. At least, from what she was prescribed then. Has anything changed in the treatment of psoriasis over these five years?
— Today there are many approaches to the treatment of childhood psoriasis. And in order to choose the right one, you need to visit the dermatologist again. What is the girl's defeat percentage now?
- Only three spots on the head and on the elbows.
— Currently, the course of psoriasis in your daughter can be regarded as benign. Your task is to prevent progression; in some cases it is not recommended to touch the plaques at all. With excessive irritation, psoriasis can be transferred from a limited form to a widespread one. The proverb “Don’t make a fuss while it’s quiet” is relevant here.
Perhaps it will be enough just to care for the scalp so that dandruff does not bother you, so that the girl does not develop complexes. Now there are special shampoos for the treatment of psoriasis of the scalp. In most cases they contain tar, which has a keratolytic effect, i.e. Effectively removes excessive peeling.
— And we use shampoos with zinc...
- It is not right.
— My daughter is 14 years old, three spots appeared on her head. The dermatologist says it's seborrheic dermatitis. But my mother, brother and sister have psoriasis, and these spots are very similar to what my relatives have. Now my daughter has growths on her elbows, the doctor says it’s an allergy. But tests for allergens revealed nothing. What should we do?
— You can ask for a referral for a consultation to the dermatovenous dispensary to which you belong geographically. Of course, your girl needs to be examined. And you need to find your own doctor who will see your daughter constantly. This is the whole value of treatment.
— My son has been sick for 11 years. It all started in the head, then psoriasis spread throughout the body, and now it has caused complications in the joints. We just can't cope.
- How old is he?
— I’m already 30 years old, I’ve been sick since I was 19.
— Which joints are affected?
“It started on one finger, and now all the joints are affected. There is morning stiffness.
— Did rheumatologists look at him?
- Yes, they say treat psoriasis.
- Now there are drugs that can help your son. They usually start with antimetabolites; if there is no effect, the prescription of biological agents should be considered. You need consultation with specialists, perhaps a joint consultation with a dermatologist and a rheumatologist.
- Can my son be cured?
— If someone tells you that psoriasis can be cured, don’t believe it. This is a chronic disease. If the diagnosis is made and confirmed, it is relevant throughout life. The task of the doctor, the patient and his immediate family is to control the disease so that its manifestations either disappear completely or are mitigated as much as possible. At the present stage, our doctors have in their arsenal all the necessary effective means to achieve this goal.
Komsomolskaya Pravda , May 17, 2015