Skin diseases have accompanied humans for thousands of years. Various types of dermatitis and non-infectious skin diseases significantly complicate a person’s life. Guttate psoriasis is a type of psoriasis that does not damage the nails. A teardrop-shaped rash appears on the torso and limbs and then spreads throughout the body.
The teardrop shape is a complication after suffering from ordinary psoriasis. This form of the disease is called wandering because it is impossible to understand where the scaly papules will appear. The disease must be treated as soon as the first pathological symptoms appear, otherwise it will become chronic.
Causes of the disease
Guttate psoriasis is not a contagious disease. Since the nature of the disease is non-infectious, it is impossible to become infected through contact with a patient with drip psoriasis. Scaly rashes on the skin appear as a result of autoimmune processes in the body. The immune system aggressively attacks its own cells, mistaking them for foreign bodies. The exact reasons for the launch of autoimmune processes have not yet been established.
There may be several exogenous risk factors for the appearance of a teardrop rash:
- Unhealthy Lifestyle;
- action of aggressive chemicals;
- poor ecology of the region of residence;
- psychological overload.
Possible endogenous causes of the disease include:
- bacterial infections;
- viral diseases;
- genetic predisposition;
There are many reasons for the appearance of the disease, so the number of people with guttate psoriasis is growing every year all over the world, and in particular in Russia.
Pathogenesis of psoriasis
The pathogenesis of the disease is not fully understood. It has been noted that a large number of activated T cells penetrate the epidermis, which trigger the proliferation of keratinocytes . The rate of their renewal changes from the usual 23 days to 3–5 days, which leads to the appearance of pathologically altered cells and peeling of the skin. Keratinocytes, which normally lose nuclei in the granular layer of the epidermis, retain them in psoriasis, which results in a disruption of the keratinization process - parakeratosis .
Against this background, uncontrolled inflammation with excessive production of cytokines: tumor necrosis factor alpha (TNF-α), interferon gamma, interleukin-12. It has been noted that a surge in TNF-α levels corresponds to exacerbations of psoriasis.
In the affected skin there is increased vascularization and dilation of superficial vessels. The main triggers of angiogenesis in psoriasis come from the epidermis - in particular, keratinocytes secrete vascular endothelial growth factor A (VEGF-A). Sources of angiogenic factors are also macrophages and fibroblasts, and additional participants are hypoxia-inducible factor (HIF), tumor necrosis factor α (TNF-α), interleukins (IL)-1, -6, -8, etc. ( Fig. 2 ) But the most important component is VEGF-A - it activates blood and lymphatic vessels, directly influencing the attraction of inflammatory cells to the psoriatic lesion. Serum VEGF-A levels correlate positively with disease severity and negatively with the success of standard therapy, indicating a critical role for VEGF-A in disease progression.
Rice. 2. The role of the vascular component of the skin and angiogenesis in the pathogenesis of psoriasis (Heidenreich R., et al. Angiogenesis drives psoriasis pathogenesis. Int J Exp Pathol 2009; 90(3): 232–248)
With the participation of vascular endothelial growth factor ( VEGF ), the proliferation of keratinocytes and vascular endothelial cells is triggered, which promotes angiogenesis. T helper cells ( Th ) produce interleukin-17 ( IL -17 ), which triggers the production of pro-angiogenic factors - this further enhances angiogenesis. Against this background, dendritic cells ( DC ) of the epidermis act on the population of T helper cells ( Th ), which begins to synthesize interferon gamma ( IFN -γ ), which suppresses angiogenesis. But this doesn’t help for long, because... other proangiogenic factors are activated: VEGF , bFGF , IL -8 , triggering further growth of small vessels and “unwinding” the pathogenesis of psoriasis.
- VEGF - vascular endothelial growth factor
- IL - interleukin
- IFN - interferon
- TNF - tumor necrosis factor
- TGF - tumor growth factor
- MMP—matrix metalloproteinases
- bFGF - basic fibroblast growth factor
- ECs - endothelial cells
- DC - dendritic cells
- Th - T-helpers
- N - neutrophils
Symptoms of the disease
The disease occurs in waves with alternating periods of exacerbation and remission. Typically, exacerbation occurs in winter. It is believed that in winter the body is weakened and is not able to resist the disease. The main symptom is a drop-shaped red papule on which small scales are located. Gradually the entire body becomes covered with papules. The limbs, back, and abdomen of the patient are especially susceptible to rashes. The rash does not spread to the face. Nails are also not affected during the development of the disease.
The rash may disappear on its own, but this does not mean that the patient has recovered. In most cases, this is a sign of the onset of temporary remission. Repeated exacerbation can occur spontaneously, without obvious reasons.
When the rash covers the entire body and limbs, but does not affect the nail plates, this is the main symptom of guttate psoriasis.
In most cases, recognizing psoriasis is not particularly difficult. Diagnostic difficulties arise with a rare form of psoriatic disease—guttate psoriasis (CP). This is due to the fact that the rashes with this type of psoriasis are in many ways similar to those with some other skin diseases. In Russian guidelines, there is almost no description of the pathomorphological picture of KP, although it has a number of features [1, 2].
According to the literature [1], PC occurs in less than 2% of patients with psoriasis. Children are more often affected, and among adults - people under 30 years of age. There are no differences in the incidence of diseases between men and women. It is emphasized that in children, KP is one of the most common types of psoriasis [3].
Clinically, KP manifests itself as sudden rashes of small (1-10 mm in diameter), teardrop-shaped, orange-pink papules, usually with fine-plate peeling on the surface. The rash is often accompanied by slight itching. Elements of the PC are usually localized on the trunk and proximal limbs. They can also be located on the face, ears and scalp. The palms and soles are rarely affected. Changes in the nails characteristic of chronic psoriasis may be absent [4, 5].
Fresh KP rashes usually appear during the entire 1st month of the disease, they remain unchanged for 2 months, and then gradually disappear [6]. Elements of the rash regress without scarring and leave behind areas of hyperpigmentation or pseudoleukoderma. In approximately 68% of people, this disease becomes chronic [1]. The course of the disease improves in the summer, and worsens in the cold season.
2-3 weeks before the onset of rash, in 80% of cases, CP is preceded by a streptococcal infection of the upper respiratory tract (for example, pharyngitis or tonsillitis) [7, 8]. Perianal streptococcal infection in children is also considered important [9]. The importance of immunological restructuring of the body under the influence of a previous streptococcal or other infection is emphasized. An increased risk of developing CP is observed in individuals with an established family history of this disease [10].
According to the literature, β-hemolytic streptococcus ( Streptococcus pyogenes
) [eleven];
Staphylococcus aureus ( Staphylococcus aureus
), some types of fungi (
Malassezia, Candida
); human papillomavirus (HPV), retroviruses [12]. Immunomodulators, as well as medications such as lithium preparations, β-blockers, antimalarials and non-steroidal anti-inflammatory drugs may be related to the onset of the disease [12].
KP in patients can go away without treatment for several weeks, so it is often not diagnosed or misdiagnosed. Patients are observed with such erroneous diagnoses as guttate parapsoriasis, Zhiber's pityriasis rosea, allergic dermatitis, and eczema. Even pathohistological examination of the elements of the rash does not always turn out to be informative regarding KP. This is usually associated with previous treatment with antibiotics and topical corticosteroids. In addition, the informativeness of a biopsy examination for diagnosing KP depends on the stage of the disease at which the biopsy was performed.
The noted difficulties in the clinical and pathomorphological diagnosis of KP served as the basis for our research, the purpose of which was to identify the clinical and morphological features of KP, allowing us to differentiate this disease from dermatoses with similar clinical manifestations, as well as to determine the clinical stage of the course of KP, at which the most significant pathohistological changes in this disease.
Material and methods
We observed 25 patients (16 women, 9 men) with diagnosed KP. The age of the patients ranged from 16 to 36 years. To clarify the diagnosis, all patients underwent a punch biopsy from the affected skin areas under local anesthesia (0.5 ml of 2% lidocaine solution). At least two biopsies were examined in each patient. A similar study was carried out on 6 patients with guttate parapsoriasis, 5 patients with pink lichen of Gibert and 12 with nummular eczema.
The biopsy material was fixed in immunofix, followed by ethanol-isopropanol processing of the biopsy material using a Milestone vacuum processor (RHS-1) and embedded in paraffin.
Histological sections 5 μm thick were prepared from paraffin blocks, which were stained with hematoxylin and eosin according to the standard method [13] and examined using a Nikon eclipse 80i light microscope, followed by microphotography with a DS-Fi1 digital camera.
results
Of the 25 patients with KP, in 20 patients the disease was preceded by bacterial or acute respiratory viral infections. In the anamnesis of these patients, 3-4 weeks before the appearance of skin rashes, acute tonsillitis, acute pharyngitis, and acute respiratory viral infection, accompanied by a rise in temperature, were noted. In 4 patients the disease occurred due to stress.
4 patients with psoriasis had relatives.
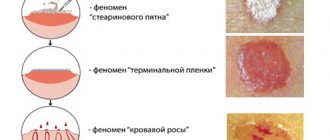
Skin rash in the form of multiple miliary and lenticular papules of pink-orange and pink-red color, 0.1-1.5 cm in size, located on the skin of the trunk and limbs; individual elements were detected on the face, behind the ears, and on the scalp. The papules were characterized by fine-plate peeling over the entire surface (Fig. 1, a)
Figure 1. Clinical manifestations of KP.
a - papular elements with peeling; b — papular elements with “collar” type peeling; c - early rashes of miliary and lenticular papules with virtually no peeling. or had the appearance of a “collar” only along their periphery (see Fig. 1, b)
.
With a short duration of the disease (1-2 weeks), miliary and lenticular papules with a smooth surface were observed (see Fig. 1, c)
. Sometimes Koebner's sign was detected. Only one patient, in addition to rashes, had pustular elements on the palms and soles of the body. In all patients, the psoriatic triad characteristic of psoriasis was determined. In addition, 5 people had a “thimble” symptom on their fingernails, and 4 had dystrophic changes in the nail plates. Slight skin itching was noted in 14 patients.
In the differential diagnostic plan, we were guided by a number of features of the clinical manifestations of some diseases that have a clinical picture similar to CP. In this regard, we most often had to carry out a differential diagnosis with guttate parapsoriasis, pink lichen of Gibert and nummular eczema.
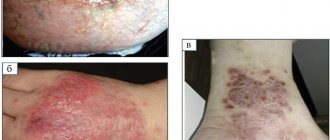
Guttate parapsoriasis
manifests itself as fairly typical nodular rashes of a round or oval shape measuring 2-10 mm
(Fig. 2, a),
Figure 2. Dermatoses with a similar clinical picture to KP. a — guttate parapsoriasis; b - nummular eczema; c - pink lichen of Zhiber. from light pink to brownish-red. The surface of the nodules is covered with dense, dry scales, attached in the center and lagging along the periphery like a wafer. This is the difference from CP, in which peeling is noted over the entire surface of the element or along its edge. With careful scraping, the scales for parapsoriasis are removed without breaking. There are also papules that are not covered with scales. When such papules are scraped, pityriasis-like peeling is observed (“the phenomenon of hidden peeling”). With more intense scraping, pinpoint hemorrhages appear on the surface of the rash and close to it on apparently healthy skin - a symptom of purpura. The infiltrate at the base of the papules is very slight and is difficult to palpate. There is usually no itching. The rashes are usually localized on the lateral surfaces of the torso and limbs, very rarely on the scalp, palms and soles. Sometimes, simultaneously with papules, roseate spots appear, often covered with lamellar scales. After 3-4 weeks, the papules spontaneously flatten and regress, leaving temporary pigmentation or pseudoleukoderma. Children suffer from guttate parapsoriasis much less often than adults. It occurs 2 times more often in women than in men [14].
Unlike KP, for nummular eczema
characterized by severe itching.
Most often, numular eczema is localized on the back of the hands, and only in some cases the process can take on a disseminated character, when widespread erythematous areas appear on the trunk and limbs, against which small vesicles and papules form lesions up to 4-5 cm in diameter. The shape of the hearths is round, similar to a coin. The color of the lesions is from pink to dark red (see Fig. 2, b)
. On their surface there is abundant drip wetting with the formation of crusts. Excoriation occurs as a result of scratching. The disease is prone to relapse.
For pink lichen of Zhiber
, which is also observed in people aged 10-30 years, unlike psoriasis, there are no typical psoriatic phenomena.
The disease often begins with a primary “maternal” plaque. The so-called “incubation period” with the subsequent generalization of the rash is characteristic, as well as the mostly spotty rather than papular nature of the elements. They are oval in shape (see Fig. 2, c)
with peeling in the form of crumpled papyrus paper. The rash is located predominantly along Langer's lines. The disease usually does not affect the scalp, face, hands and feet. Skin manifestations regress relatively quickly. Difficulties in differential diagnosis often arise in the initial stage of the disease, when psoriatic elements look like spots without a noticeable infiltrate [5]. In most patients, it is possible to note a pronounced seasonal nature of the disease with exacerbations, which most often occur in the autumn-winter period [14].
The main histological signs of plaque psoriasis are parakeratosis, acanthosis of the epidermis in the area of the interpapillary processes, and above the papillae, thinning of the Malpighian layer and, in addition, elongation and swelling of the dermal papillae. In the papillae and in the upper third of the dermis, dilated and tortuous capillaries and lymphohistiocytic infiltrates with an admixture of neutrophils were noted. CP revealed morphological signs characteristic of early psoriasis. They were characterized by more pronounced inflammatory infiltrates and less pronounced acanthosis compared to chronic plaque psoriasis [1, 2]. Early elements (miliary papules, papules with a smooth surface) revealed swelling of the papillary dermis and dilation of the capillaries with the presence of a lymphocytic infiltrate surrounding the capillaries. Red blood cell extravasation was noted. Orthokeratosis was observed covering areas of parakeratosis with the presence of loosely located neutrophils. Exocytosis of leukocytes spread to the epidermis, where a small focal spongiosis developed (Fig. 3a).
Figure 3. Morphological picture of the PC. Hematoxylin and eosin staining (×100). a — early psoriasis. Parakeratotic masses with neutrophils. Moderate acanthosis, focal spongiosis, increased mitotic activity in the epidermis. Dilated capillaries at the ends of the dermal papillae. Perivascular lymphocytic infiltrates mixed with neutrophils; b — psoriasiform hyperplasia of the epidermis. Vacuolar degeneration of the granular layer. Dilated capillaries in the dermal papillae; c — psoriasiform acanthosis. Areas of agranulosis under the parakeratotic layer; d — Munro microabscesses forming under areas of parakeratosis. Extravasation of red blood cells in the papillae of the dermis; e - exocytosis of neutrophils into the psoriasiform epidermis - “papillary splashes” (left). Munro's microabscesses. Perivascular lymphohistiocytic infiltrates mixed with neutrophils; e - pronounced exocytosis of neutrophils with the formation of spongioform Kogoya pustule in the upper parts of the epidermis.
In fully developed scaly papules with PC, granular cells of the epidermis looked vacuolated (see Fig. 3, b)
.
After their lysis, foci of agranulosis were determined, followed by the formation of areas of parakeratosis (see Fig. 3, c)
.
Neutrophils were not only scattered throughout the orthokeratotic masses of the stratum corneum, but were also located on the surface of the parakeratotic masses. As a result of the accumulation of neutrophils in the parakeratotic layer, Munro microabscesses were formed (see Fig. 3, d)
, as a result of the migration of neutrophils from the papillary capillaries through the thickness of the epidermis with their subsequent grouping in the parakeratotic masses.
This was called the phenomenon of “papillary splashes” (squirting papillae; Fig. 3, e)
[1].
In some cases, pronounced exocytosis of neutrophils with their concentration in the upper part of the spinous layer led to the formation of small spongiform Kogoya pustules (see Fig. 3, f)
. Increased mitotic activity was observed in the epidermis. He became increasingly hyperplastic. Swollen dermal papillae with dilated and tortuous capillaries were detected. Perivascularly there were moderate infiltrates of lymphocytes, histiocytes with a small admixture of neutrophils and single eosinophils, as well as erythrocyte extravasates.
Based on the described histological picture, pathognomonic for the period of the disease, characterized by the appearance of early scaly papules, the diagnosis of psoriasis can be confirmed.
Differential diagnosis of KP with guttate parapsoriasis, pityriasis rosea of Gibert, and nummular eczema in the study of biopsy specimens was based on the analysis of histological features that make it possible to distinguish these diseases. For example, with guttate parapsoriasis, as well as with KP, parakeratosis, acanthosis, and migration of infiltrate cells into the parakeratotic layer can be observed. However, unlike CP, more pronounced focal spongiosis and vacuolar degeneration of the basal layer of the epidermis are detected, and in the dermis there are dense muff-like lymphohistiocytic infiltrates and changes in the walls of blood vessels, characteristic of vasculitis (Fig. 4, a)
[15].
Figure 4. Morphological picture of dermatoses that have clinically similar rashes to KP.
Hematoxylin and eosin staining (×40). a — guttate parapsoriasis; b - pink lichen of Zhiber; c - nummular eczema. For pink lichen of Zhiber
histological changes are very reminiscent of early psoriasis, however, areas of spongiosis and small vesicles in the spinous layer, exocytosis of lymphocytes and diapedesis of erythrocytes into the epidermal papillae serve as distinctive features
(see Fig. 4, b)
[2].
For nummular eczema
the exudative component is more pronounced - spongiosis in the spinous layer of the epidermis up to the formation of vesicles and pustules in the upper parts of the epidermis, as well as more pronounced inflammatory cell infiltration of the dermis
(see Fig. 4, c)
[15].
conclusions
The clinical features of skin manifestations in KP include the sudden appearance of an abundant small papular rash covered with small plastic scales, localization of the rashes mainly on the skin of the torso and extremities, and the frequent precedence of the disease by acute infectious pathology of the upper respiratory tract with a febrile symptom.
The morphological features of the PC are especially clearly manifested in the presence of developed scaly papules. These include moderate acanthosis, the presence of neutrophils in orthokeratotic masses of the stratum corneum and on the surface of parakeratotic masses, the formation of Munro microabscesses, vacuolization of granular cells with the formation of foci of agranulosis, increased mitotic activity in the epidermis, and the phenomenon of “papillary splashes” (squirting papillae).
The given main clinical and morphological features allow us to differentiate KP from dermatoses with similar clinical manifestations. At the same time, biopsy diagnosis has the greatest value in the verification of CP precisely during the period when pronounced scaly papules appear (3-4 weeks from the onset of the disease).
Diagnosis and treatment
A dermatologist diagnoses and treats the disease. It is often impossible to confirm the diagnosis during examination. To determine the nature of the rash, the following laboratory tests are prescribed:
- a smear of the mucous membranes of the oral cavity to exclude an infectious cause of the rash;
- blood test for allergens;
- antigen study;
- general urine analysis;
- patient's skin biopsy.
The teardrop form of psoriasis can be treated only under the supervision of a doctor. To date, the causes and pathogenesis of the disease have not been fully studied, and therefore self-medication is unacceptable.
There is no general treatment regimen. Doctors can only eliminate the symptoms and increase the period of relative rest. The doctor will select medications for treatment. Patients are prescribed hormonal and bacterial ointments. However, these drugs have severe side effects and are therefore used with caution.
During the recovery period, preventive measures must be taken. Switching to dietary nutrition and reducing the level of emotional stress reduces the risk of disease. You also need to harden your body and switch to a lighter work regime. This will strengthen the body and prolong the period of remission.
Prices for services
Initial appointment with a dermatologist (assessment of patient complaints, history taking, examination, preliminary diagnosis, consultation)
Primary appointment – visiting a doctor of a specific specialty for the first time. Make an appointment
1510 ₽ 2160 ₽
Repeated appointment with a dermatologist
Make an appointment
800 ₽
Treatment of mild psoriasis for 7 days (7 Dermalight procedures or 7 injections with our drugs + ointment from our components)
Make an appointment
4000 ₽
Treatment of moderate psoriasis for 7 days (3-6 droppers; 4 injections with our drugs; ointment from our components; 4 Dermalight procedures)
Make an appointment
5500 ₽
Treatment of severe psoriasis for 7 days (6-7 droppers or 12 injections with our drugs; ointment from our components; 4-6 Dermalight procedures)
Make an appointment
8000 ₽
Note: Most often, treatment of any grade requires a minimum of 4 weeks of treatment.
Psoriatic arthritis
Psoriatic arthritis can be considered both a type of psoriasis and arthritis. There are 5 types of the disease, we will look at the common features.
Manifestations
- the skin becomes red, bluish, purple;
- joint damage, up to deformation;
- swelling of fingers and toes.
Common sites of injury
- small finger joints;
- knee and hip joints;
- joints on the shoulders and shoulder blades;
- vertebrae
Photo
Hand deformity due to psoriatic arthritis
Leg deformity due to psoriatic arthritis