Causes of tinea versicolor
The content of the article
Ringworm affects middle-aged people. Medicine identifies the causes that lead to the appearance of this disease in humans. These include:
- Predisposition to fungal skin diseases.
- Disruptions in the course of physiological processes in the epidermis.
- Endocrine diseases.
- Lack of a good night's sleep.
- Lack of rest.
- Time zone change.
- Excessive hygiene, using antiseptics.
- Improper functioning of the human immune system.
- Frequent bathing in salt water.
- Lack or excess of vitamins.
- Wearing clothes made of synthetic materials.
- Improper functioning of the lymphatic drainage system.
- Long-term use of steroid hormones.
- Nervous system problems.
- Hormone imbalance.
- Lack of hygiene measures in public places.
Dermatologists have known about Gibert's rosacea (RL; synonyms: lichen maculae and ringworm, scaly roseola, disseminated lichen) for more than 150 years (described by S. Gibert in 1860), but its etiology and pathogenesis remain unknown [1, 2]. This dermatosis is considered an inflammatory disease of unknown etiology [3]. In LV cancer, a certain causal role is noted for a number of background diseases and conditions of patients, in particular, neurotrophic and endocrine disorders, respiratory infections, visceral pathology, focal diseases, and intoxications [1, 2]. A viral etiology of LVH is suggested [4], and streptococcal genesis is also not ruled out [1, 5], but researchers are more inclined to the infectious-allergic nature of this disease [1, 3, 5].
LV cancer is included in the group of presumably infectious diseases [1, 2, 6]. The infectious nature of this dermatosis is indicated by the presence of mild prodromal symptoms, seasonal nature (usually occurs in spring and autumn), simultaneous disease of members of the same family (rarely observed), maternal plaque (primary focus) and generalized rash, paroxysmal efflorescence, slight enlargement of regional lymph nodes [ 2-4, 7]. Other representatives of this group are psoriasis, lichen planus, polymorphic exudative erythema.
The rash is preceded by a mild period of prodrome in the form of malaise, headache, myalgia, arthralgia, redness of the pharynx, and low-grade fever. After 7-10 days, a bright pink maternal plaque (reaching at least 5 cm in diameter) appears on the body in the form of a medallion, oval-round in outline. Its central part is yellowish, somewhat sunken, the edges are pink, slightly elevated. The elements of the rash are located randomly, discretely, but can touch and even merge, located on the torso, proximal areas of the skin of the extremities, in the axillary and inguinal folds, and rarely on the neck [1, 2, 8]. Itching is usually absent or mild, rarely severe [3, 8, 9]. The orientation of efflorescence along Langer lines is noted [3, 6]. In approximately 20% of patients, there is no maternal plaque, and in some cases there are several of them, which is regarded as an atypical manifestation [2, 8, 9].
In the clinical picture of LVH, one should note the peculiarity of the spots - their pink corolla and a collar of thin scales, in the center resembling crumpled (corrugated) tissue paper [8].
The diagnosis of LV cancer is based on characteristic clinical manifestations [2, 9], but in order to avoid diagnostic errors, one should remember about the atypical manifestations of dermatosis - papular, urticarial, hemorrhagic, vesiculobullous, pustular rashes, accompanied by intense itching [1, 2, 8, 10]. Sometimes, apart from the maternal plaque, there are no other rashes or they are located on the face and neck, and may also have a target-like appearance. Histological changes are not specific [1, 6].
The range for the differential diagnosis of RLZ includes a number of diseases: mycosis of smooth skin, seborrheic dermatitis, psoriasis, parapsoriasis, secondary syphilis, multiform exudative erythema, toxicoderma, Lyme disease, coin-shaped eczema, pityriasis versicolor, Devergie's disease.
RLZh compares favorably with many dermatoses by spontaneous recovery in 6-8 weeks, persistent immunity, as well as a pathognomonic feature - lacy collar folds and a bright pink corolla of spots and maternal plaque.
The prognosis of the disease is favorable. In most cases, treatment for patients with LV cancer is not required [2, 9]. However, for acute inflammatory, exudative phenomena and complicated forms, Presocial, antihistamines, sodium thiosulfate, and glucocorticosteroid drugs are used [9].
For severe rashes, antibacterial drugs are used (for example, erythromycin for 14 days), as well as ascorbic acid, calcium pantothenate, and suberythemal doses of ultraviolet radiation [10]. Externally, shaken mixtures, lorindene C, hyoxysone, and 10% methyluracil ointment are prescribed [1, 6].
It is recommended to avoid water procedures and wearing synthetic clothing; spicy, salty foods are excluded from the diet [1, 3]. It is recommended to limit the consumption of chocolate, citrus fruits and spices.
We present clinical observations of patients with LV cancer who were in City Clinical Hospital No. 14 named after. V.G. Korolenko (Fig. 1-7).
Figure 1. Patient Ts., 55 years old.
Figure 2. Patient R., 31 years old.
Figure 3. Patient S., 13 years old.
Figure 4. Patient K., 14 years old. a - front view; b — rear view.
Figure 5. Patient K., 10 years old. a - front view; b — rear view.
Figure 6. Patient Ts., 13 years old.
Figure 7. Patient Zh., 8 years old. a - front view; b — rear view.
Patient Ts., 55 years old (see Fig. 1)
, the “maternal” plaque in the back area was discovered a week before going to the doctor, daughter exanthemas began to appear 6 days after the appearance of the “maternal” plaque. There was no itching. No treatment was given.
Patient R., 31 years old, a plaque with a diameter of 2 cm of oval-round outline appeared on the skin of the left breast near the areola (see Fig. 2)
. The edges of the lesion, 2 cm wide, are pink-red, the central part is yellowish with thin scales. A similar rash appeared on the skin of the right breast after 4-5 days and on the skin of the torso (spots up to 1 cm in diameter). No treatment was given.
Patient S., 13 years old, was admitted to the DCVO on March 30, 2013 with a diagnosis of psoriasis (see Fig. 3)
. The duration of the disease was 1.5 months, it began with the appearance of a pink plaque with peeling on the thigh. The rash subsequently spread to the torso and limbs. There was no itching. Concomitant diseases: juvenile gynecomastia. Treatment: calcium gluconate, oxacillin, nystatin, mezim-forte, antihistamines; externally - zinc-oil and zinc-water talker. Full resolution of efflorescence.
Patient K., 14 years old (see Fig. 4)
. He had been ill since December and was sent to the hospital with presumptive diagnoses of psoriasis and parapsoriasis. He was treated at the DKVO from 05/23/13 to 06/21/13.
Dermatosis began with rashes on the skin of the chest, then the process spread to the torso and limbs. He was treated as an outpatient with naphtoderm, sulfur-salicylic ointment, radevit, elocom S. He took a bath every other day, and a hygienic shower every day.
Upon admission to the hospital, the acute inflammatory process is represented by spots, papules of bright pink color with oval outlines, the elements of the rash are swollen, covered with crusty scales. Moderate itching was noted. Treatment: intravenous infusion of saline with 30% sodium thiosulfate solution, calcium gluconate, antihistamines, diprospan 1.0 No. 1, cefazolin (intramuscular), enterosgel, delagil (1 tablet per day), Essentiale Forte, Sonopax, external zinc-oil and naphthalan mash, elocom cream, 2% naphthalan paste, 1% methylene blue solution. The rashes have regressed.
Patient K., 10 years old (see Fig. 5)
, was sent for treatment to City Clinical Hospital No. 14 named after. V.G. Korolenko with a diagnosis of guttate parapsoriasis. Disease duration - 2 weeks. First, a pink plaque with peeling appeared on the skin of the abdomen. Soon similar spots of smaller sizes were found on the torso and limbs, in the inguinal folds. The “maternal” plaque is 3.5 cm in diameter, edematous erythematous scaly spots up to 1 cm in size, without itching. According to laboratory and instrumental examinations, as well as consultations with specialists, no pathology was identified. Diagnosis: LV. Treatment: sodium hyposulfite, enterosgel, tavegil, macropen; zinc-oil mash, 5% ASD paste, 1% methylene blue solution. The rashes have regressed.
Patient Ts., 13 years old (see Fig. 6)
, 1.5 months was treated as an outpatient for psoriasis (white salik externally). The DCVO confirmed LVH. Treatment: oxacillin, calcium gluconate, enzistal, antihistamines, 2% naphthalan paste, 1% salicylic cream, 5% ASD paste, 1% methylene blue solution. The rashes have regressed.
Patient Zh., 8 years old (see Fig. 7)
, received external laticort and zinc paste for 2 weeks as an outpatient. Water procedures. The itching didn't bother me. Upon admission to the DCVO, a multiple rash of pink, swollen spots was observed; some of the elements in the central part had a collar of thin scales, reminiscent of crumpled tissue paper. Elements of the rash on the trunk and limbs with a diameter of 0.5-0.7 cm, on the neck - 1.5-2 cm. There was a tendency towards peripheral growth of efflorescence and merging into larger lesions. Treatment: oxacillin, calcium gluconate, enzistal, antihistamines, 2% naphthalan paste, 1% salicylic cream, 5% ASD paste, 1% methylene blue solution. The rashes have regressed.
At first glance, LVRD does not represent a pressing dermatological problem. The main thing is timely recognition and refusal of water procedures, which ensures spontaneous regression of the pathological process within 6-8 weeks. Unfortunately, at present, patients with pityriasis rosea are admitted to hospital treatment due to inadequate treatment and care due to erroneous diagnosis. Intense insolation also plays a negative role. With irrational therapy, complications are observed in the form of eczematization, impetiginization, which leads to an increase in recovery time to 2-3 months.
Method of infection
Mushrooms can come into contact with the skin of a healthy person, but with strong immunity, the body uses protective functions and the disease does not occur.
Main routes of transmission:
- Skin contact with the carrier.
- In public places: shower, fitting room.
- Use of a person’s personal belongings: towel, washcloth.
When infected with this microorganism, symptoms do not appear for 2 weeks to several months. They may not appear at all unless a situation arises when the immune system weakens.
Description of the disease
Pityriasis versicolor is a disease of the upper layer of the epidermis, caused by a fungus of the genus Malassezia. For a long time it can be asymptomatic, and subsequently affects only the stratum corneum of the skin and the hair cuticle. It affects mainly young people aged 14 to 40 years, and is practically not diagnosed in children under 7 years of age. Treatment of pathology is systematic and includes the use of antifungal agents for internal and external use. Otherwise, the lichen begins to grow, spreading to increasingly large surfaces of the epidermis.
Homeopathy and herbal medicine
For patients with individual hypersensitivity to components in most drugs, doctors often prescribe homeopathic remedies and herbal medicine sessions. This treatment regimen is suitable for women during pregnancy. During this period, the use of many medications is prohibited. A good therapeutic effect is observed from Psorilom tablets.
Their composition is absolutely safe and does not cause side effects. This drug is also available in the form of ointment and gel for external use, shampoo and spray.
Homeopathic tablets, as a rule, are allowed to be taken not only during pregnancy, but also during lactation.
To eliminate the external manifestations of lichen, doctors recommend herbal medicine sessions. Patients are prescribed tinctures based on calendula, propolis and celandine. You can either prepare them yourself at home or purchase them ready-made at any pharmacy chain.
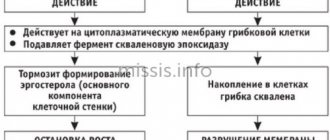
Tablets for pityriasis versicolor
Systemic antifungal drugs are available in the form of tablets or capsules. Their help is resorted to in severe cases of lichen, when external means in the fight against the fungus have proven ineffective. Most often, doctors prescribe medications from the table below.
| Drug name | Features of application | Price |
| Rumicosis | The composition contains itraconazole, a substance that, when taken in a course, retains antifungal activity for 28 days. The single dose selected by your doctor should be taken twice a day. Contraindications include children under 12 years of age, disorders of the gastrointestinal tract, liver and heart diseases. | 396 rubles |
| Itrazole | Take 2 capsules twice a month. Then they take a break for 3 weeks, and after that the treatment is repeated 2 or 3 times, depending on the dynamics of recovery. The drug is available with a doctor's prescription. Treatment may be accompanied by disorders of the gastrointestinal tract, nervous and vascular systems. In some cases, allergies appear in the form of a rash and severe itching. | 276 rubles |
| Fluconazole | The medication is available in the form of capsules, tablets or syrup. The active component is the substance of the same name, fluconazole. The medicine does not have a cumulative effect and is eliminated from the body within 24 hours. Adults are prescribed 50 mg of the drug once a day or 150 mg once a week. The maximum duration of therapy is 6 weeks. | 62 rubles |
Antifungal agents in tablet form may have other restrictions on use. Therefore, a preliminary consultation with a doctor is mandatory. Otherwise, you can harm your own health, and the disease will continue to progress.
Diagnosis of lichen
Diagnosis of all types of lichen includes:
- listening to patient complaints;
- anamnesis analysis;
- inspection of rashes to determine their color, size, shape, location, etc.
Further, the dermatologist’s actions depend on the preliminary diagnosis he made.
Diagnosis of pityriasis rosea
To diagnose pityriasis rosea in a child or adult, in addition to a medical examination, during which the final diagnosis is usually determined, the following is additionally carried out:
- microscopy of scales to exclude syphilis;
- serodiagnosis of syphilis.
A biochemical and general blood test is also taken, and a general urine test is given.
Diagnosis of herpes zoster
Usually, a doctor can accurately determine whether a patient has pityriasis rosea during an examination. But in some situations additional research methods are required:
- detection of viral DNA by polymerase chain reaction in the contents of vesicles and in the blood;
- determining the presence of antibodies to the pathogen;
- identification of the pathogen virus genome in cells/tissue sections using in situ hybridization.
Diagnosis of pityriasis versicolor (lichen)
Diagnosis of versicolor versicolor pumps in:
- Balzer test (iodine test). The affected areas of the skin are treated with iodine and immediately wiped with alcohol. Pityriasis versicolor always turns brown;
- examination under a Wood's lamp (lichen looks like a brown or yellow glow);
- microscopic examination of scales (allows one to identify hyphae (curved short filaments of mycelium), oval and round spores).
Diagnosis of ringworm
To determine ringworm, the following are carried out:
- examination of lesions using a Wood's lamp (lichen becomes green);
- microscopic examination;
- sowing the discharge on various nutrient media (to determine the sensitivity of the pathogen to antibiotics);
- biochemical and general blood tests, urine analysis.
Diagnosis of lichen planus
To diagnose lichen planus in an adult/child, a small affected area of skin is taken for histological examination. The patient is also prescribed a general urine and blood test and biochemistry.