An infectious disease such as ringworm is caused by various types of fungi, most often of the Microsporum or Trichophyton genus.
Cost of services in our clinic
| Appointment with a dermatologist, candidate of medical sciences | 1500 rub. |
| Consultation with a dermatologist (KMS) when removing 2 tumors | 0 rub. |
| Removal of a neoplasm (wart, mole) using the radio wave method | 500 rub. |
| Make an appointment by phone: 8-800-707-15-60 (toll-free) |
| *The clinic is licensed to remove tumors |
The disease manifests itself in the form of pinkish, scaly, rounded spots on the skin. The incubation period is one to two weeks from the moment of infection.
Causes and types of disease
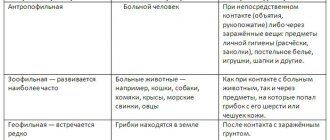
Ringworm, microsporia, trichophytosis is a disease transmitted to humans from animals. Very often children who play with stray cats and dogs become infected. The disease can also be caught from a sick person through hygiene items, personal belongings and through direct contact.
Factors that provoke the appearance of ringworm in a person include:
- Contact with a sick animal, often a cat or dog. Infection is possible, including through lost fur. In this case, the disease is designated by the term microsporia, as it is caused by a fungus of the genus Microsporum, and is characterized by a more severe course.
- Ringworm is contracted through direct interaction with a sick person, for example, through handshakes and hugs. A fungus of the genus Trichophyton can parasitize humans. In this case, the term trichophytosis is used to refer to the disease.
- Infection through household and hygiene items: shared towels, soap, washcloth, comb, as well as dishes, shoes or clothing used by a sick person. Transmission of the fungus can occur by touching a surface that has been touched by someone infected with ringworm.
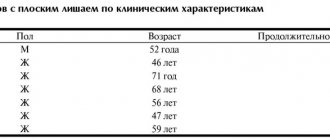
Lichen planus
Lichen ruber planus, described by Wilson in 1869, is a chronic inflammatory disease characterized by monomorphic papules on the skin and visible mucous membranes, most often on the oral mucosa and red border of the lips, accompanied by itching of varying severity. Today, this disease remains an urgent problem associated with the constant frequency of its detection, the lack of a unified pathogenetic concept, as well as the presence of severe forms and a chronic course, often resistant to therapy [1, 4, 6, 13]. In the general structure of dermatological morbidity, lichen planus (LP) accounts for 0.78–2.5%, among diseases of the oral mucosa - 35%. This disease occurs in all races, in all age groups and in both sexes, although the mucous membrane is more often affected in women from 40 to 60 years of age [1, 19].
Etiology and pathogenesis. In modern literature, various theories of the development of LP can be traced, such as viral, neurogenic, hereditary, intoxication and immunoallergic [1, 10, 15, 17].
The immunoallergic theory of the development of this pathology, based, according to various authors, on a decrease in the number of T cells in the patient’s blood and their functional activity, deserves the most attention at present. Some authors have shown a decrease in T-helper cells and an increase in the T-helper/T-suppressor ratio [11–14].
On the oral mucosa, manifestations of LP are associated with the presence of pathologies in patients with the gastrointestinal tract (gastritis, colitis, etc.), liver, and pancreas. Also, in a number of patients there is an undoubted connection between the development of the disease and vascular (hypertension) and endocrine (diabetes mellitus) pathology. Trauma to the oral mucosa, including those caused by dental pathology, has a certain significance in the development of the disease on the oral mucosa: sharp edges of teeth, poorly fitted removable plastic dentures, missing teeth, etc. [1, 6, 7].
Recently, there have been increasing reports of the development of lichen planus of the skin and oral mucosa in response to the action of certain chemicals on the body, including drugs. The so-called lichenoid reactions have been described in people whose work is related to the development of color film, who have contact with paraffinylenediamine, who have taken tetracycline (tetracycline lichen), para-aminosalicylic acid (PAS), gold preparations, etc. Thus, the disease in some cases may present is an allergic reaction to certain medicinal and chemical irritants.
Clinical manifestations of LP are characterized by the formation of a monomorphic rash, consisting of flat, polygonal, with a shiny surface and centrally recessed papules of pinkish-violet or crimson-reddish color, with a diameter of 2–3 mm. On the surface of the papules there is a peculiar shine with a waxy tint, which is especially noticeable in side lighting. Papules, merging, form small plaques, on the surface of which there are small scales. When the surface of papules and especially plaques is lubricated with vegetable oil, small whitish dots and intertwined web-like stripes appear through the stratum corneum (Wickham's symptom), this is due to uneven thickening of the granular layer of the epidermis. When pathological lesions resolve, persistent hyperpigmentation often remains. Dermatosis is accompanied by itching, often very intense, depriving patients of rest and sleep [1, 7–10, 15, 19].
LLP is localized on the flexor surfaces of the forearms, in the area of the wrist joints, on the inner surface of the thighs and extensor surfaces of the legs, as well as in the inguinal and axillary areas, and the oral mucosa. The pathological process usually does not involve the skin of the face, scalp, palms and soles. In the area of the extremities, the rash may have a linear (zoniform) arrangement.
About 25% of patients with LP have only lesions of the mucous membranes (mouth, glans penis, vestibule of the vagina) and are not accompanied by manifestations on the skin. On the mucous membrane of the cheeks, grayish-opaline dotted papules are formed, grouped in the form of rings, networks, laces, on the surface of the tongue - flat, whitish opal plaques with clear jagged edges, reminiscent of foci of leukoplakia, on the red border of the lips (usually the lower) - small purple ones plaques, slightly flaky, with a grayish-white mesh on the surface [1, 7–10, 15, 19].
Changes in nails with pronounced longitudinal striations, sometimes in the form of ridges, hyperemia of the nail bed with focal clouding of the nail plates of the hands and feet are observed in some patients with LP [1, 15].
LCP is characterized by an isomorphic reaction to irritation. Often, typical elements of dermatosis are located linearly at the sites of excoriation (Koebner phenomenon). The disease lasts a long time, often for many months. There have been cases of generalization of dermatosis with the development of secondary erythroderma (lichen ruber planus generalisata) [1, 7–10].
Several atypical forms of lichen planus are identified [2, 3, 17]:
- hypertrophic, warty form (lichen planus hypertrophicus, seu verrucosus);
- atrophic and sclerotic forms (lichen planus atrophicus, lichen planus sclerosus);
- pemphigoid, or vesicular, form (lichen ruber pemphi goides, seu bullosus);
- lichen ruber moniliformis (lichen ruber moniliformis);
- pointed, perifollicular form (lichen planus acuminatus, sen planopilaris);
- erosive-ulcerative form (mucous membrane).
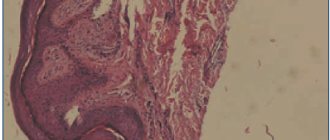
Diagnosis . With classic manifestations of LP, diagnosis is not difficult and it is established clinically. In doubtful cases, histological examination can help, where a typical mononuclear infiltrate will be present, disrupting the basal line of keratinocytes [1, 3].
In some patients, differential diagnosis of LP with psoriasis and syphilis is carried out, since lichen planus rashes on the skin may resemble psoriatic elements and syphilitic papules. However, papules in LLP have the characteristic color of the rash, a polygonal shape, an umbilical depression in the center of the papules, a Wickham grid, and the absence of the phenomena of stearin stain, varnish film and pinpoint bleeding allows us to differentiate lichen planus with psoriasis. Papules are round and hemispherical in shape, their “ham” color, density, positive serological reactions to syphilis make it possible to distinguish syphilitic papules. It may be difficult to make a diagnosis if the rash is localized on the oral mucosa.
The clinical picture of LP of the oral mucosa is differentiated from leukoplakia, lupus erythematosus, syphilitic papules and other diseases.
Leukoplakia, unlike LP, has keratinization in the form of a solid grayish-white plaque and does not have a patterned lesion.
In lupus erythematosus, the lesion is hyperemic, infiltrated, hyperkeratosis is present only within the focus of inflammation in the form of tender points, short stripes, sometimes merging along the edge of the lesion in the form of stripes and arcs; in the center of the lesion there is atrophy, which will not occur with LP.
Syphilis papules are usually larger, round or oval in shape, their surface is covered with a grayish-white coating, which is usually removed when injured, and pale treponemas are found on their surface. Positive serological reactions to syphilis [1, 3, 15, 19].
Treatment approaches
LLP is often a chronic but benign disease, sometimes asymptomatic, and does not require systemic treatment. However, taking into account the frequent chronicity of the process and the many severe and atypical forms, the complexity of its pathogenesis, successful treatment is possible only with complex and individualized treatment using modern tools and methods [4, 11, 16, 18].
It is especially important to consider the factors that contributed to the onset of the disease. It is necessary to eliminate risk factors - household and professional hazards, concomitant diseases, foci of focal infection. They carry out sanitation of the oral cavity and prosthetics. Food products should not cause irritation to the mucous membranes of the mouth. Attention is paid to previous treatment and drug tolerance [11].
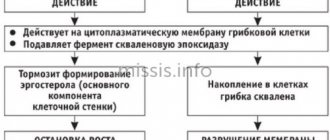
Due to the fact that the material basis of the disease is immune inflammation (delayed-type hypersensitivity reaction - DTH), correction of immunity is of particular importance and the disease itself responds well to immunosuppressants. To interrupt the cooperative connection of immunocompetent cells, glucocorticosteroids in combination with 4-aminoquinoline derivatives (hydroxychloroquine, chloroquine) are prescribed as basic therapy, especially for common and resistant forms. However, drugs that suppress immune processes should be used only in the presence of documented visceral damage or if the erosive process interferes with eating or speaking.
In the presence of intense itching, in the acute period of the disease, histamine H1 blockers and antiserotonin drugs and catecholamine blockers are indicated. Along with this, sedatives and antidepressants are prescribed to help normalize sleep and reduce itching.
Vitamin therapy has a beneficial effect on metabolic processes. The proliferation and differentiation of keratinocytes is influenced by vitamin A (daily dose for adults - 100,000 IU). Retinoids - derivatives of vitamin A (Tigazon, Neotigazon, Etretinate) reduce the intensity of the inflammatory reaction, affect the condition of cell membranes and normalize proliferation processes. Retinoids are effective against lesions of the oral mucosa and red border of the lips. In recent years, analogues of vitamin A - carotenoids - have been successfully used, especially in atypical forms, in particular erosive-ulcerative, as well as in cases of damage to the oral mucosa and genital organs.
Vitamin E (alpha-tocopherol acetate), used as an antioxidant and inhibitor of the cytochrome P450 system, allows for complex treatment with corticosteroids to reduce the daily dose and shorten the duration of steroid therapy. The multivitamin preparation Aevit is indicated for patients with a long-term chronic course of the disease, with verrucous forms and damage to the mucous membranes.
In chronic relapsing dermatosis, agents that improve oxygen supply to tissues are indicated.
External treatment with applications of corticosteroid ointments, solutions and shaken mixtures with menthol, anesthesin, citric acid, and antihistamines is prescribed for intense itching. Hypertrophic foci are destroyed by cryodestruction or electrocoagulation. Erosive-ulcerative lesions are subject to local treatment with epithelizing agents, including Solcoseryl, sea buckthorn oil, and rosehip oil.
Currently, the method of combined phototherapy (UVAB, ultraviolet irradiation) is successfully used. This therapy affects immune responses by damaging immune cells in the skin. At the same time, the superficial lymphocytic infiltrate in the dermis disappears, and the cellular composition in the epidermis is normalized.
Of the listed means and methods, only their rational choice - sequential stage-by-stage (course) application, taking into account the individual characteristics of the patient and the nature of the course of the disease - allows one to achieve positive results.
Recently, immunotropic therapy for lichen planus has been increasingly used, including the use of exogenous interferons (Reaferon, Interlock) and interferonogens (Neovir, Ridostin).
If the disease is suspected to be caused by any drug or chemical, its use should be discontinued. A thorough examination of patients is necessary to identify internal diseases. First of all, you need to examine the gastrointestinal tract, blood sugar levels, and neuropsychic state [1, 11, 15, 19].
In the absence of symptoms, treatment is not required. To reduce itching, antiallergic drugs are used. The doctor may also prescribe vitamins, sedatives, and physiotherapy.
Physiotherapeutic procedures include electrosleep, diadynamic paravertebral currents, and inductothermy of the lumbar region. Antipruritic shaken suspensions, corticosteroid ointments, 2–5% tar-naphthalan ointments are prescribed externally. The prognosis for life is favorable.
As with any chronic process, LP requires local and systemic therapy [15, 19].
Local drugs of choice are corticosteroids. Class I and II corticosteroids are prescribed. For verrucous process, occlusive dressings with class II corticosteroids are recommended. Intralesional administration of drugs is used, but this method should only be used for very persistent verrucous plaques.
Corticosteroids are effective for lichen planopilaris of the scalp, but they should be applied to the periphery of the plaque and not to its center. Also, betamethasone preparations in the form of foam are very suitable for this localization of the lesion.
For mucosal lesions, especially if they are erosive or ulcerated, triamcinolone pastes or gels are prescribed, which improves the condition in 65% of such patients after 2 weeks. The use of 0.025% fluocinolone based on 4% hydroxycellulose gel in combination with chlorhexidine and miconazole gel for an antifungal effect improved the condition in 50% of patients and served as a prevention of oral candidiasis.
You can rinse the mouth for 5 minutes with one soluble tablet (500 mcg) of betamethasone, originally intended for systemic use. However, this rinsing method is only useful for lesions that have eroded de novo and not for lesions that have eroded due to trauma.
Fluocinonide 0.025% 6 times a day for 2 months is active compared to placebo and without side effects. Betamethasone valerate in aerosol form was used for 2 months with good results in 8 of 11 patients. Clobetasol propionate 0.05% was recently found to be more effective than fluocinonide 0.05%.
Intralesional administration of corticosteroids has been used for lichen planus of the oral mucosa. The preferred drug is triamcinolone acetonide, which is prescribed at a dose of 5–10 mg/ml weekly or twice a week for 3–4 weeks [4, 18, 19].
Topical retinoids are used for lesions in the oral cavity. Fenretinide, for example, gave excellent results when used twice daily, with no local or long-term side effects. Retinoic acid 0.1%, tretinoin 0.025%, and isotretinoin gel 1% were all effective, but less effective than topical triamcinolone or flucinonide [19].
Systemic treatment
Cyclosporine A (CyA) specifically targets cell-mediated hypersensitivity reactions and is the drug of choice for LP. The initial dose is usually 5 mg/kg/day. It is reduced to 2 mg/kg/day as soon as possible: regimens with a treatment duration of more than 6 months should be avoided. Blood pressure should be monitored weekly and kidney function monthly. The best indication for the use of CyA is severe erosive LP.
Systemic corticosteroids may be used instead of CyA. Prednisone can be prescribed at a dose of 1 mg/kg/day (or a lower dose). The dose is reduced over 1 month. When the drug is discontinued, a rebound effect may occur. Common side effects of corticosteroids are common.
For erosive LP with chronic active hepatitis, azathioprine (50–100 mg/day) is recommended. Normalization of transaminase levels is usually accompanied by improvement of lesions in the oral cavity. However, if a patient has antibodies to the hepatitis C virus, all immunosuppressive treatments should be avoided, since immunosuppressive drugs may contribute to the development of liver cancer.
Other drugs that have been shown to be beneficial in reversing the clinical process of LP include thalidomide, hydroxychloroquine, retinoids, and levamisole.
Hydroxychloroquine is used at a dose of 200–400 mg/day for several months in patients who have lesions in the oral cavity. When analyzing the risk-benefit ratio, retinal side effects must be taken into account and carefully monitored.
For systemic treatment of LP, acitretin (0.25–0.75 mg/kg/day) and isotretinoin (0.25–0.50 mg/kg/day) are used. However, these drugs should not be prescribed to women of childbearing age due to their well-known teratogenicity [19].
In severe forms of erosive oral lichen planus that do not respond to traditional treatment, PUVA therapy (PUVA = Psoralens + UltraViolet A) can have a positive effect. A dose of 0.6 mg/kg 8-methoxypsoralen is administered orally 2 hours before irradiation with long-wave ultraviolet light. In one study, irradiation was administered 12 times at 2–3 day intervals for a total dose of 16.5 J/cm2. In another study, 20 sessions were performed, 3 per week, with a total cumulative dose of 35.9 J/cm2. After treatment, clinical symptoms and erosive lesions disappeared. Side effects are similar to those observed after whole body PUVA therapy [16, 19].
Evaluation of treatment effectiveness. Provided that the therapy is correctly selected, regression of the pathological process occurs within 1–2 weeks, the rash disappears after 1–1.5 months. Clinical cure (recovery) is characterized by the complete disappearance of papules, in the place of which hyperpigmented or depigmented spots remain. The latter can remain for an indefinite period of time (from several weeks to several months). Erosive-ulcerative, hypertrophic and atrophic forms of lichen planus are usually resistant to therapy, and the rashes persist for several months or even years.
Primary prevention consists of sanitation of foci of chronic infection, treatment of psychoneurological disorders; Overwork and stress should also be avoided. Prevention of exacerbations: prescribing water treatments - baths, showers (not recommended in the acute period of the disease), hydrogen sulfide and radon baths; diet (exclusion from the diet of coffee, spices, chocolate, honey, alcohol) [1, 10, 17, 19].
Literature
- Bazyka D. A., Bazyka A. D. Etiology, pathogenesis and therapy of lichen planus // Vestn. derm. and veins 1977, No. 11, p. 58.
- Gadzhimuradov M.N., Gunaeva A.A. Atypical forms of lichen planus: clinical manifestations, differential diagnosis and treatment // Clinical dermatology and venereology. 2009, No. 3, p. 85–80.
- Differential diagnosis of skin diseases. Ed. B. A. Berenbein and A. A. Studnitsyn. M., 1983. P. 269.
- Korsunskaya I.M., Nevozinskaya Z.I., Zakharova A.B., Konstantinov E.M., Andryushkova Yu.A. Experience in the treatment of lichen planus with the drug Glutoxim // Russian Journal of Skin and Venereal Diseases. 2008, No. 1, p. 44–46.
- Maksimovskaya A. N., Tsarev V. N., Guseinova S. S. Bacteriological basis for the treatment of lichen planus of the oral mucosa using laser radiation. In the book: Proceedings of the VI Congress of the Russian Dental Association. M., 2000, p. 275–277.
- Manukhina O. N. Clinical course of lichen planus of the oral mucosa against the background of decreased functional activity of the thyroid gland. M.: Science to Practice, 1998. pp. 145–147.
- Mashkilleyson A. L. Diseases of the mucous membrane of the oral cavity and lips. M.: Medicine 1963. P. 188.
- Pashkov B. M. Lesions of the oral mucosa in skin and venereal diseases. M.: Medicine 1963. P. 182.
- Petrova L.V. Features of the clinical course of lichen planus of the oral mucosa // Ros. magazine cutaneous veins bol. 2002; 3:28–31.
- Pototsky I.I. Directory of dermatovenerologist. Kyiv, 1985. P. 88.
- Rabinovich O. F. Immunological aspects of the pathogenesis of lichen planus of the oral mucosa (clinic, diagnosis, treatment). Diss. Dr. med. Sci. M., 2001, 190 p.
- Raikhlin A. N. Subcellular mechanisms of development of lichen planus of the oral mucosa and its treatment: Abstract of thesis. dis. ...cand. honey. Sci. M., 1986.
- Slesarenko N. A. Lichen planus (modern immunological and biochemical aspects) and methods of pathogenetic therapy: Abstract of thesis. dis. ...Dr. med. Sci. M., 1995.
- Spitsyna V.I. Pathogenesis of immunodeficiency in patients with lichen planus of the oral mucosa // Russian Dental Journal. 2002, No. 3, p. 30–34.
- Thomas P. Habiff. Skin diseases. Diagnosis and treatment. M.: “MEDpress-inform”, 2008. 672 p.: ill.
- Faizulin R. A. The use of dimocyphon and selective phototherapy of patients with lichen planus, taking into account immunological blood parameters: Abstract of thesis. dis. ...cand. honey. Sci. M., 1992. 21 p.
- Fedorov S. M., Selissky G. D., Timoshin G. G. Lichen planus // Skin diseases. M.: GEOTAR-Medicine, 1997. pp. 67–69.
- Khamaganova I.V. Advantan (methylprednisolone aceponate) in the complex treatment of lichen planus // Bulletin of Dermatology and Venereology. 2004, No. 3.
- Rebora A. Lichen planus. European guidelines for the treatment of dermatological diseases. Ed. A. D. Katsambasa, T. M. Lotti. M.: “MEDpress-inform”, 2008. pp. 371–374.
A. S. Bisharova, Candidate of Medical Sciences
GBOU DPO RMAPO Ministry of Health and Social Development of Russia, Moscow
Contact information about the author for correspondence
Symptoms and complications
This lichen is called ringworm because when it is infected, the hair on the head breaks off at a distance of about half a centimeter from the skin and appears as if it has been cut off. As a result, bald spots are formed and increase in size. Reddish spots with a bright ridge around the circumference form on the body, vellus hair breaks off at the site of the lesion, turning into nodules. It creates the feeling of a seal placed on the skin.
In people with weakened immunity and severe concomitant diseases, severe forms of trichophytosis occur:
- Infiltrative
, in which gray swollen spots appear on the skin, quickly increasing in size. The patient's temperature rises and the lymph nodes in the affected area become enlarged. - Purulent
, characterized by deep skin lesions with the release of pus and the appearance of ulcers on the surface of the lichen. Sometimes purulent contents appear in the form of yellow cloudy drops. Patients' general condition worsens, their temperature rises, and their lymph nodes become enlarged. Without treatment, blood poisoning may occur.
The fungus can affect various parts of the body, including the arms, legs, and face. Foci of the disease also form on the scalp, and in men - in the area of the mustache and beard. The disease often affects the nails, and the hands and feet may also be affected. Particularly unpleasant sensations are caused by the formation of plaques in the armpits or in the groin folds.
Ringworm is characterized by symptoms such as:
- burning and itching in the affected area;
- swelling, pain, purulent discharge that occurs in advanced cases;
- dandruff and focal baldness when spots are localized in the hairline area;
- general weakness and malaise.
In children, during exacerbation of the disease, episodes of fever, enlarged lymph nodes, and disturbances in the functioning of the digestive system are common. If the treatment is not started in a timely manner or is chosen incorrectly, the disease can become chronic.
Symptoms of lichen
What symptoms indicate that you have contracted lichen planus? It should be noted that lichen affects not only the skin of the body, but also mucous membranes, nails and even human hair. As a rule, any type of this disease begins with the appearance of the following symptoms:
- minimal increase in body temperature;
- the appearance of chills, mild headache, and sometimes nausea;
- later the temperature rises, and itching appears in certain places (face and body, less often - limbs);
- after a few hours, bubbles will appear at the site of redness, which soon burst and only a crust remains.
Diagnosis and treatment of ringworm
Before starting treatment, you need to make a correct diagnosis. Differential diagnosis is carried out by a dermatologist based on the patient’s complaints and existing symptoms.
In ringworm, the plaques are round, edged with vesicles or scales, and have a reddish spot in the center. To distinguish trichophytosis from other skin diseases, the spots are irradiated with a Wood's lamp. The illuminated lichen lesion has a bluish-green color. When skin particles are inoculated in the laboratory, “fluffy” colonies of the fungus grow.
Additionally, a special analysis is taken using the scraping method to determine the type of fungus.
Treatment of lichen in adults
The diagnosis of lichen planus is made by a dermatologist; only in some cases additional tests are necessary. If the diagnosis is made incorrectly, then treatment can bring a negative result, which can lead to the transition of the disease to the chronic stage.
Treatment of lichen planus should be comprehensive. Only a doctor can select a remedy that will help to cope with the disease as much as possible, taking into account the stage of infection and its extent within certain areas of the body.