Symptoms
The disease manifests itself in the form of spots on the skin.
First, several so-called maternal formations about 5 cm in size appear. Then, over the course of a week, a large number of similar spots of smaller sizes scatter throughout the body. The most vulnerable areas are the abdomen, shoulders and hips. Rashes are rare on the face and neck. All spots, both maternal and “baby” ones, have the same appearance: pink or with a yellowish tint, round in shape, flaky inside with a smooth rim. Often, apart from spots, this disease does not manifest itself in any way. Therefore, as soon as any characteristic formations are discovered on the body, you should immediately contact a special clinic to diagnose pityriasis rosea. Sometimes itching appears in the affected areas, and the lymph nodes on the neck and chin become enlarged. If a person’s immunity is severely weakened, severe fatigue, fever or general intoxication of the whole body appears. There are cases when the external manifestation differs from the usual: blisters or white nodules appear on the skin.
Diagnosis of the disease
Determining the correct diagnosis is sometimes difficult due to the absence of a pathogen. The disease can be confused with other lichen and toxicoderma.
The examination is a visual inspection. A qualified dermatovenerologist will take into account the characteristic placement of spots on the body, their appearance, shape, and based on this will make a diagnosis.
Tests that may also be prescribed:
- general urine and blood tests;
- microprecipitation reaction (diagnosis of syphilis);
- scraping from affected areas.
After diagnosis, the specialist will determine how to treat pityriasis rosea and will advise the patient in detail regarding lifestyle.
Make an appointment
Methods of infection
To date, there is no consensus on the methods of infection.
There is an assumption that the source of the disease is the herpes virus and that people with low immunity, those who have recently suffered viral infections, colds, and who are often hypothermic are primarily at risk of contracting Zhiber's disease. Women and children have a significantly higher risk of infection than men. Observations show that people over 40 years of age and infants practically do not become infected with this infection. Is this disease contagious? There is no clear answer to this question. There is an opinion that it can be transmitted through tactile contact or airborne droplets. A prerequisite for a person to become infected is the presence of a provoking factor. In practice, it has been noted that transmission of this virus from one person to another occurs infrequently.
Treatment
Only a qualified specialist can determine what exactly a person has become infected with.
First a visual inspection is carried out. However, this is not enough. This type of disease looks very similar to psoriasis, rubella or syphilitic roseola. To accurately diagnose and prescribe the correct treatment for lichen, the clinic prescribes a blood and urine test, takes a scraping, and the patient undergoes a special test. Gibert's disease does not require particularly complex treatment. The disease goes away in six to nine weeks. The spots gradually fade and stop peeling. For some time, marks remain on the skin, but they also disappear over time. To alleviate the symptoms, the doctor prescribes treatment: to relieve itching - antihistamines, to reduce peeling - various ointments. Multivitamin complexes are also prescribed to increase the patient’s immunity.
In addition to drug treatment of pityriasis rosea, a hypoallergenic diet is prescribed. All foods that can cause allergic reactions are excluded from the diet: citrus fruits, eggs, red fruits, chocolate, coffee, alcohol, honey, nuts.
It is also necessary to exclude physical activity, passing exams, limit communication in order to avoid getting into stressful situations, try to wear clothes made from natural fabrics, and wash only in the shower with mild detergents. It is also forbidden to expose the affected areas of the skin to direct sunlight, as this increases the peeling process and, accordingly, impedes healing. Any self-medication can lead to undesirable consequences, so consultation with a specialist is necessary.
Treatment at the Baltmed clinic
If you live in another city or you do not have the opportunity to visit the clinic, we suggest using an online consultation with a dermatovenerologist.
To get a consultation, you need to make an application to the clinic - write to the chat on the website (in the right corner of the screen) or call by phone. The consultation is carried out on the basis of the Personal Account, the patient communicates with the doctor via video link, and the patient also has the opportunity to attach tests and previous studies.
The cost of an online consultation is 1800 rubles, duration is 30 minutes.
Introduction
Lichen planus (LP) is a chronic inflammatory skin disease that is accompanied by damage to the skin and mucous membranes of the mouth and genitals.
The disease is characterized by papular rashes of various forms and nature and is most often accompanied by severe itching [1]. The prevalence of LP is unknown exactly, but the proportion of patients with this disease at an outpatient dermatologist appointment is 1.3–2.4%. The disease most often occurs in middle-aged people, but cases of the development of LP in children have been described. Women get sick as often as men [2]. Damage to the oral mucosa can develop in isolation or be combined with skin manifestations. Despite the fact that this disease sometimes affects small areas of the skin and mucous membranes, its impact on the quality of life is underestimated [3]. LP is characterized by a chronic course, and spontaneous resolution of the disease is rare [4, 5]. Sometimes different forms of LP may progress with progression of severity and, therefore, require lifelong monitoring and supportive therapy. The treatment of cutaneous forms of LP is most often carried out by dermatovenerologists, and with damage to the mucous membranes - by dentists.
The etiology of LP is still unknown. The pathogenesis of LP is also not entirely clear, but the disease is thought to arise from an immune response presumably involving CD4+ and CD8+ T lymphocytes producing cytokines, interleukin-2 and tumor necrosis factor, which cause a chronic inflammatory response and apoptosis of keratinocytes [6] . Therefore, it is not surprising that this disease is also associated with other diseases that have a common immunological basis [7]. LP is observed in families of different generations, which suggests the presence of a genetic predisposition to this disease [8, 9]. Indeed, genetic polymorphisms of various human leukocyte antigen (HLA) markers, gene polymorphisms of various HLA markers, as well as inflammatory cytokines and chemokines have been studied [10, 11].
The clinical manifestations of LP and their impact on patients are significant. It was shown that CLP significantly affected the quality of sleep, which led to the development of depression in patients [12]. It has also been shown that the longer the duration of subjective symptoms, the worse the quality of life and the higher the level of stress [13, 14]. Thus, the chronic course of LP and, especially, its exacerbation is associated with stress, anxiety, depression and, ultimately, with a deterioration in the patient’s quality of life.
LLP is characterized by a chronic relapsing course. The disease begins with the appearance of widespread rashes, severe itching, and weakness. Often the clinical picture of LP manifests itself acutely. Classic cases of LP are characterized by the presence of dermal-epidermal papules with a diameter of 1–3 mm with polygonal outlines, an umbilical central depression, the absence of peripheral growth, and the presence of a Wickham network caused by unevenly expressed hypergranulosis and visible in the depths of the papules after applying water or glycerin to the surface. Papules are characterized by a bluish-red or lilac color with a pearlescent tint and, when illuminated from the side, a shine. When the size of the elements reaches more than 3–4 mm, they, merging with each other, form larger lesions that take the form of plaques, various figures, and rings. Lichenoid papules are characterized by localization on the flexor surfaces of the forearms, lateral surfaces of the torso, anterior abdominal wall, oral mucosa, and genital mucosa. The front surface of the shin can be considered a favorite place. Lesions in LP can be localized or generalized and have the character of erythroderma. The most torpid course of LP occurs in patients with verrucous, hypertrophic and erosive-ulcerative forms, as well as in combination with diabetes mellitus, arterial hypertension and damage to the mucous membranes (Grinshpan-Wilapol syndrome) [15, 16].
Depending on the skin manifestations, the following forms of LP are distinguished: typical (classical), atypical, hypertrophic, pemphigoid, follicular, pigmented, erythematous, ring-shaped.
The mucous membranes are very often involved in the pathological process; they can be isolated or combined with skin lesions. Isolated lesions of the oral mucosa are observed in the presence of metal dentures. According to the clinical course of LP of the mucous membranes, varieties are distinguished: typical, exudative-hyperemic, bullous, hyperkeratotic [1].
The question of the genetic predisposition of patients to LP remains relevant. Previously obtained results suggest the presence of an associative relationship between LP and HLA complex antigens. The presence in the phenotype of the HLA B35 antigen, as well as combinations of HLA A2-B5, HLA A2-B35, HLA A3-B35, HLA A3-A19 and HLA B12-B35 can be considered as a factor in the development of LP. When studying the distribution of HLA class II specificities, the role of HLA-DRB1*10 predisposing to the development of LP was reliably identified. In turn, the specificities DQB1*11 and DRB1*15 (DR2) play a protective role against this disease [17–21].
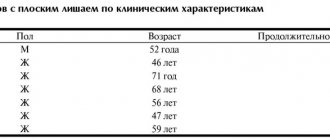
Clinical observation of LP
Patient K., born in 1956, was admitted to the skin department of the Kirov Regional Clinical Dermatovenerologic Dispensary on November 18, 2019 with complaints of rashes on the skin of the torso, limbs and oral mucosa. Severe skin itching occasionally bothers me. Notes a decrease in quality of life.
She considers herself sick since the spring of 2022, when rashes first appeared on the back of her feet. The disease is not associated with anything. The patient self-medicated, used an ointment containing betamethasone and antihistamines, but the effect was insignificant. In January 2022, she consulted a dermatologist at her place of residence. She was observed with a diagnosis of “ring-shaped erythema”. She received outpatient treatment with little effect. The disease was chronic. The patient noted that the rash did not go away completely, and the process began to become widespread. She was sent for further examination and treatment to the Kirov Regional Clinical Dermatovenerological Dispensary.
From the life history
. Born and lives in the Kirov region. Secondary specialized education. Does not work. Denies HIV, tuberculosis, hepatitis A, B, C, blood transfusions, previous sexually transmitted infections. Denies drug intolerance. Past illnesses: acute respiratory infections. There is no hereditary history of skin diseases. Denies injuries or surgeries. Denies bad habits.
Chronic diseases: cerebral atherosclerosis, discirculatory encephalopathy stage I, vestibuloataxic and neurosis-like syndromes. Hypertension of the 2nd degree, stage II, risk 3. Dyslipidemia. Varicose veins. Constantly takes medications: atorvastatin, cardiomagnyl.
Gynecological history: menopause since age 45. 8 pregnancies, 2 births.
General inspection.
The condition is satisfactory, consciousness is clear. Physical examination of organs and systems revealed no peculiarities. Heart rate 80 beats per minute. Blood pressure 140/70 mm Hg. Art. Physiological functions are normal.
Local status.
The pathological process is widespread, symmetrical, chronic in the acute stage. It is localized on the skin of the trunk, upper (mainly flexor surfaces) and lower extremities, and on the oral mucosa. It is represented by multiple small dense up to 0.1 cm in diameter, smooth hemispherical, slightly flattened shiny papules of pink-red color with a purple tint. The elements are arranged in a ring shape, with a diameter of more than 5 cm, in the central part of the lesions the skin is of normal color, the peripheral edge consists of adjacent nodules. There are scattered isolated papules with slight peeling on the surface. The Wickham grid sign was positive, and the Koebner phenomenon was also positive. On the mucous membrane of the cheeks and lower lip, small whitish papules are located symmetrically, merging with each other into a thin network. The mucous membranes of the genital organs are free from specific rashes. Dermographism pink. Peripheral lymph nodes are not enlarged (Fig. 1–4).
Clinical blood test
: leukocytes 6.7*109/l (eosinophils 4%, lymphocytes 40.4%), erythrocytes 4.66*1012/l, hemoglobin 137 g/l, platelets 243x109/l, ESR 17 mm/h. General urine analysis: straw-yellow, transparent, protein 0.026 g/l, specific gravity 1.020, glucose - negative, pH 5.5, leukocytes, erythrocytes were not detected. Biochemical blood test: ALT 21 U/l, AST 21 U/l, cholesterol 3.0 mmol/l, total bilirubin 12.1 µmol/l, glucose 5.3 mmol/l, creatinine 89 µmol/l, total protein 74 .3 g/l.
When taking fingerprint smears, Tzanck cells were not found.
HLA phenotype: A02, 09 (24), B12 (44), 35. DRB1* 01, 14.
Biopsy result
. Focal hyperkeratosis, moderately severe acanthosis, in places with a “sawtooth” configuration, focal hypergranulosis of the granular layer, vacuolar degeneration of keratinocytes of the basal and spinous layers, focal spongiosis. In the dermis there is a diffuse band-like lymphohistiocytic infiltrate, in close contact with the basement membrane zone with focal blurring of the dermo-epidermal border. The pathohistological picture is characteristic of LP (Fig. 5, 6).
Treatment was prescribed in accordance with the standard of specialized medical care for LP. The dose of methylprednisolone was prescribed: 4 mg orally according to the scheme (3-2-0) with a gradual reduction in the dose after discharge by 1 tablet once every 5 days until complete withdrawal. As replacement and concomitant therapy, including for the prevention of side effects, the following are prescribed: omeprazole, antihistamines, potassium preparations, calcium gluconate, preparations containing vitamins A and E, ferrous sulfate and vitamin C, hydroxychloroquine (according to 200 mg 2 times a day for 5 days, then a break of 2 days, courses of treatment are recommended to be repeated for 2 months). Local treatment: quenching with fucorcin solution, ointment with fluocinolone acetonide.
Treatment in the hospital lasted 14 days. The patient was discharged in satisfactory condition with improvement under dispensary observation by a dermatovenerologist at her place of residence.
How to avoid infection
Due to the fact that the nature of the occurrence of Gibert's disease has not been thoroughly studied, there are no methods to prevent this disease. The main recommendation is to monitor the state of the immune system, as it will help avoid infection.
Complications
The disease itself in most cases goes away without leaving a trace. However, sometimes complications arise in the form of eczema, staphylococcus or streptococcus; ring-shaped lichen can develop, which quite often becomes chronic and even after a few years a relapse can occur. Then treatment is done with antibiotics. To prevent such problems, we strongly recommend that you undergo comprehensive treatment in our clinic. Don't forget about your health and the health of your family!