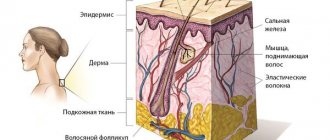
A pigmented nevus (birthmark) is a benign skin neoplasm that occurs as a result of disruption of the normal structure of melanocytes—pigment cells containing melanin. They originate from the neural fold and, during embryogenesis, move to the basal (germ) layer of the skin of various parts of the human body. When the normal maturation or migration of these cells is disrupted, a congenital form of nevus occurs. Such deformed melanocytes (nevocytes) do not have processes, are characterized by poor metabolism and are capable of excessive pigmentation of the skin.
Moles, or pigmented nevi, occur in 90% of people
Melanoform nevus was assigned an ICD 10 code – D 22.
What are nevi?
- It can occur anywhere on the body and in any age group. It is most often found on the skin from birth, and increases in proportion to the child’s growth (in case of excessive growth, immediate consultation with an oncologist is required).
- One of the most common skin formations (80-90% of the population). Occurs more often in women. In representatives of dark races, pigmented nevi are less common than in whites.
- It does not cause discomfort to a person and has no symptoms even in case of degeneration (10-20%). For this reason, self-monitoring and periodic (once a year) examination by an oncologist are recommended.
- In older people, pigmented nevi are more common due to age-related skin characteristics.
- Moles are extremely sensitive to external influences (direct sunlight, for example). They have a tendency to malignancy, especially in constantly injured areas. The only treatment option is surgical removal of the formation.
Types of epidermal nevi
There are several clinical types of epidermal nevi. This classification is not definitive, since epidermal moles can be hard, linear and inflamed at the same time.
Soft papillary nevus of the epidermis . This is most often a small flesh-colored or gray formation with a soft, velvety surface. Individual papules forming clusters resemble senile warts.
Hard papillary nevus.
Unilateral, segmented, most often located on the trunk and limbs. These are tall or flat, raised discolorations of normal skin, light or dark brown, with a papillary surface.
Inflammatory linear verrucous epidermal nevus.
This is a special form of epidermal nevus with inflammation and severe itching. ILVEN may worsen and disappear, especially in the form of psoriasis-like psoriasis.
According to the conclusions of the study. Altman and Mehregan, diagnostic criteria for such moles include a number of features:
- early onset is noted - in 75% of cases before 5 years,
- more common in females (4 times more often);
- frequent localization on the left lower limb and buttocks;
- itching is usually present;
- histopathological appearance resembling psoriasis - a characteristic pattern of parakeratotic areas with visible psoriasis-like epidermal hyperplasia, mild spongy edema and exocytosis of lymphocytes;
- Such nevi have no tendency to spontaneous regression and resistance to treatment.
The lesions are linear, pruritic, erythematous lesions with a flaking surface and may resemble psoriasis lesions with a linear pattern. They are distinguished from psoriasis by the absence of Munroe microcirculation and the lack of epidermal involucrin expression in ILVEN. The connection with psoriasis is confirmed by the participation of the cytokines IL-6, IL-1, TNF-alpha, ICAM-1 in the pathogenesis.
Horny nevus (nevus corniculatus)
. This is the rarest form of epidermal nevus. The clinical picture shows very intense keratosis with the formation of thick papillary growths and filamentous formations. Histopathological examination shows foci of acantholysis with depressions in the epidermis filled with dense keratin.
Pediatric epidermal nevus.
This variety is characterized by congenital hemidysplasia, unilateral ichthyosis and limb defects. All of these disorders can occur, but it can only be the cutaneous form. The lesions are located unilaterally and do not extend beyond the midline of the body, with the most common lesions being the flexor folds. They have the character of erythematous lesions covered with yellow hyperkeratotic scales and sometimes with horny plugs. This type of mole occurs only in women because the gene responsible for the condition is located on the X chromosome.
Epidermal nevus syndrome, which is a combination of epidermal nevus with other developmental defects, has been clinically identified.
There are 4 clinical variants of the syndrome (Michalovsky classification):
- four-symptom form - lesions of the skin, bones, nerves and eyes.
- three-symptomatic form - skin, bone and nervous changes.
- two-symptomatic form - skin and bone changes.
- monosymptomatic form - the presence of a linear papillary epidermal nevus.
Kinds
Classification of melanocytic nevi according to J. Bhawan (1979) depending on the origin:
| View | Subspecies |
| Epidermal | Intraepidermal, borderline, complex. This group also includes special forms: spindle cell or epithelioid, nevus of balloon-forming cells, halonevus |
| Dermal | Mongolian spot, nevus of Oto, nevus of Ito and blue |
| Mixed dermal and epidermal | Combined |
| Melanoma precursors | Congenital, dysplastic |
Formations of epidermal origin are usually acquired and occur in adolescence.
Size classification:
- small (0.5–1.5 cm) – only observation is indicated;
- medium (1.5–10 cm), planned surgical removal of the tumor is optimal;
- large (over 10 cm) planned palliative therapy is indicated (surgical treatment due to the large area is not always indicated);
- giant – occupy one or more anatomical areas; Only palliative therapy and observation are indicated (surgical treatment is not used).
Treatment
Treatment is indicated for dysplastic, nodular and giant pigmented nevi due to their possible malignancy • Indications for excision of any pigmented formation •• Change in color, size, shape and consistency •• Pain syndrome •• Regional lymphadenopathy • Further therapy after excisional biopsy of a healthy area skin are prescribed based on the results of histological examination and localization of the formation.
ICD-10 • D22 Melanoform nevus • I78.1 Non-tumor nevus • Q82.5 Congenital non-tumor nevus
Application. Sturge-Weber syndrome (185300) is classified as phakomatoses, characterized by a triad: congenital cutaneous angioma (flaming nevus), usually along the trigeminal nerve, often unilateral; homolateral meningeal angioma with calcification and neurological signs; angiomas of the choroid, often with secondary glaucoma; in incomplete forms, any two or more signs are possible, sometimes with angiomas of a different localization “encephalotrigeminal angiomatosis” Sturge-Weber disease “nevoid amentia.”
Causes
There are the following reasons for the occurrence of these neoplasms:
- Congenital features. Violation of cell migration and their redistribution between the dermis and epidermis. In children, pigmented nevi are mostly caused by precisely this mechanism.
- Genetic predisposition. Associated with impaired proliferation of epidermal and dermal cells due to hereditary defects in cell structure.
- Impact of environmental factors. First of all, these include the effect of direct sunlight. In this case, a restructuring of the cellular structure of the nevus may occur and the neoplasm may degenerate into malignant forms such as melanoma. The second most important factor is the unfavorable background radiation.
- Traumatic injuries. Scratching the tumor, damaging it with clothes and shoes, as well as damage due to mechanical friction of skin areas against each other.
- Incorrect treatment. If the treatment approach is incorrect, a relapse of the disease may occur. This also includes attempts at self-medication (cauterization with acid, for example).
- Ethnicity. The factor is associated with the peculiarity of the redistribution of melanocytes in different races. In particular, people with pale skin and blond hair have the worst prognosis (high risk of degeneration).
- Disruption of the endocrine system (for example, changes in hormonal levels during pregnancy). Indirectly affects the formation of pigmented nevi or their degeneration, since a restructuring of all metabolic processes in the body (including the skin) occurs.
- Eating disorders. This factor is related to the development of almost any formation in the human body.
There is no single reason for the appearance of one or another variant of pigmented nevus; its occurrence is often associated with the related action of a number of factors.
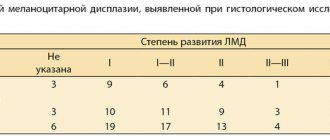
Material and methods
From June 2009 to April 2014, in the surgical department of the Central Clinic of the Literary Fund, for the purpose of prevention and early diagnosis of skin melanoma, 82 pigmented formations with a clinical diagnosis of dysplastic nevus were excised. The diagnosis was made based on clinical signs: irregular nevus shape, very dark or uneven color. By collecting anamnesis, the researchers tried to find out whether the nevus had existed since childhood or appeared in adulthood, and whether there had been any changes in it in the last 1-5 years. Inspection of nevi was carried out in good lighting; a dermatoscope was used if necessary to differentiate a nevus from non-melanocytic skin formations (keratomas, hemangiomas, dermatofibromas, etc.). It should be noted that recently the possibilities of dermatoscopy have expanded and with some experience it can help in the differential diagnosis of benign nevus and early melanoma, therefore dermatoscopy should be in the arsenal of a dermatologist when examining melanocytic formations.
Excision of dysplastic nevi with subcutaneous tissue was carried out on an outpatient basis under local anesthesia, at a distance of 0.4-1.0 cm from the visible boundaries. Histological examination was carried out in the Clinical Diagnostic Department of OJSC "Medicine", if necessary, the preparations were reviewed at the Moscow Research Institute of Orthopedics. P.A. Herzen.
Often patients refrained from excision of the nevus, explaining that it did not bother them. In these cases, we scheduled a repeat examination after 6 months. If changes in the nevus were detected over the elapsed period, surgery was re-offered; if there were no changes, further observation was continued. We recommended that all patients with dysplastic nevi avoid prolonged sun exposure, protect their skin from the sun with clothing, and use sunscreen.
It should be noted that almost all dysplastic nevi in our observations were discovered during a routine examination by a surgeon, oncologist or dermatologist. The patients themselves did not consult doctors about dysplastic nevi, since they did not bother them. Therapists also rarely referred patients with dysplastic nevi to an oncologist. All this can be explained by the fact that both patients and doctors believe that all flat pigmented formations are benign and do not pay attention to them. Foreign authors also note that doctors and patients have a misconception about dangerous pigmented formations [11]. It is necessary to ensure that doctors and patients pay attention not to papillomatous nevi, which are benign, but to flat pigmented formations that have an unusual shape and dark or uneven color.
Characteristics of various types of pigmented nevi
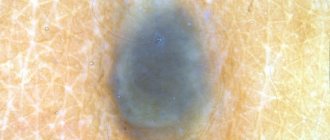
Border
It is formed in utero (often it does not appear immediately, but 1-2 months after birth). There is no favorite localization; it occurs on any area of the skin. The risk of transformation into a malignant form is high. The prognosis is favorable with proper treatment.
Appearance (pictured):
- flat lesion of round or oval shape;
- color from dark brown to black, uneven color (pigmentation intensifies at the edges in the form of concentric rings);
- size from a few millimeters to 4-5 cm;
- the surface is smooth, the boundaries are clear;
- hair may grow on the surface of the formation;
- single or multiple;
- sometimes there is slight infiltration around the formation.
Intradermal
It usually occurs between 10 and 30 years of age. Favorite localization is the face, neck, torso. The prognosis is favorable. The risk of malignancy is low.
Intradermal nevus has clear boundaries and is dark in color.
Appearance:
- papule or node with a diameter of up to 1 cm (protrudes above the surface of the skin);
- spherical or hemispherical shape;
- color dark brown or black.
Difficult
Occurs in people of all ages. Favorite localizations are the face, scalp and torso. The prognosis is favorable, the risk of malignancy is average.
Appearance:
- up to 1 cm in diameter;
- covered with hair;
- located at skin level;
- has a light brown tint.
spindle cell
It is also called Spitz nevus. It predominates in children; it practically does not occur in older people. Favorite localization – face, legs. The prognosis is favorable (prone to involution), the risk of degeneration is low.
Appearance:
- often single;
- round or oval shape;
- the surface is smooth (less often it can be warty);
- color from pink to dark brown;
- diameter on average 1-2 cm;
- affects deep-lying layers, therefore it can bleed when injured.
Balloon cell nevus
It occurs more often in young people. There is no favorite localization. The prognosis is conditionally favorable due to rapid growth, the risk of malignancy is average.
Externally:
- has the appearance of a spot, does not protrude above the skin;
- color from yellow to dark brown;
- has clear boundaries (yellow rim around the formation).
How to distinguish a regular mole from a dysplastic nevus?
Atypical nevi have a number of characteristic features that can occur either individually or in combination with each other.
| Round, symmetrical shape | Uneven edge and/or asymmetrical shape |
| Completely flat or completely raised above the skin | One part can be raised, the other flat (fried egg) |
| Uniform color or shades of brown | Black, red, brown at the same time |
| Size less than 6mm | Size over 6mm |
| Localization on any part of the body | Rarely located on the face |
Signs of malignant degeneration
Signs of the transition of a typical pigmented nevus to melanoma are as follows:
- change or heterogeneity in color;
- rapid growth;
- dropouts (appearance of small dots around the central focus);
- blurred or broken boundaries;
- ulceration, bleeding, hyperemia;
- enlargement of regional lymph nodes.
It is difficult to distinguish melanoma from a nevus by external signs; a doctor’s examination is required
To determine treatment tactics, consultation with an oncologist and a surgeon is indicated.