Urea is an organic substance found in body tissues and fluids. Many cosmetic brands use it in the production of skin and hair care products. Its main task is to maintain an optimal level of moisture in the epidermis and body cells. It is this property that is valued by people who want to preserve youth and beauty for a long time. Helps cells recover, heals wounds, has exfoliating and analgesic properties. This list of actions is used to create many cosmetic products.
Why add it to cosmetics?
Urea is responsible for protein synthesis and supplying the body with nitrogen. In cosmetology, synthetic derivatives of carbon dioxide and ammonia compounds – urea – are used.
- The chemical compound has a hygroscopic function. Retains moisture in body tissues and prevents dehydration.
- Moisturizes. It increases the level of moisture in the deep layers of the epidermis, therefore it is used by people with dry skin and for diseases accompanied by increased dryness - eczema, psoriasis.
- Formation of a protective barrier. Promotes accelerated renewal at the cellular level, creates an invisible film.
- Serves as a conductor of nutrients. Helps beneficial compounds penetrate deep into tissues, nourishing them from the inside.
- Exfoliating effect. Urea serves as a natural exfoliant. Removes keratinized layers of the epidermis along with dirt, dust, and promotes renewal.
- Heals wounds. It has anti-inflammatory and regenerating properties, thanks to which damage to the skin heals faster.
Urea promotes penetration of actives into the skin
Urea not only moisturizes the skin, but optimizes its water balance, and this is an invaluable service! Do not forget that creams and gels containing urea prevent the skin from losing moisture: in the summer without such care it is simply a disaster.
Urea promotes the healing of small wounds, so it is always included in pharmaceutical ointments, creams for cracked feet, after shaving and hair removal lotions.
Particular attention should be paid to the delicate exfoliating effect of urea: it does not look like peeling, but the skin looks fresh and elastic. This is especially important for acne; moisturizing and gentle exfoliation eliminate blackheads and inflammatory elements. If you want a light peeling effect, then enhance the urea with lactic acid; together they wonderfully prettify the skin.
Where is urea added?
- Moisturizing creams for face and body. Helps maintain optimal moisture levels, preventing overdrying.
- Body care lotions. They contain up to 10% urea, thanks to which they moisturize even very dry skin on the elbows and knees.
- Hair products. Add shine and elasticity.
- Deodorants. Urea has an antiseptic effect, which helps prevent the appearance of unpleasant sweat odor.
- Toothpaste. Prevents the growth and reproduction of bacteria that cause the development of oral diseases.
- Cosmetics for the area around the eyes. Moisturizes thin, sensitive skin, relieves puffiness, prevents the formation of small expression wrinkles.
- Anti-aging serums. Promotes the production of your own collagen and elastin, which rejuvenate, give elasticity and smoothness.
- Moisturizing creams for face and body. Helps maintain optimal moisture levels, preventing overdrying.
- Body care lotions. They contain up to 10% urea, thanks to which they moisturize even very dry skin on the elbows and knees.
- Hair products. Add shine and elasticity.
- Deodorants. Urea has an antiseptic effect, which helps prevent the appearance of unpleasant sweat odor.
- Toothpaste. Prevents the growth and reproduction of bacteria that cause the development of oral diseases.
- Cosmetics for the area around the eyes. Moisturizes thin, sensitive skin, relieves puffiness, prevents the formation of small expression wrinkles.
- Anti-aging serums. Promotes the production of your own collagen and elastin, which rejuvenate, give elasticity and smoothness.
Contraindications
The compound is on the list of safe substances, but there are still some restrictions on its use.
- It is not recommended for use by people with oily skin prone to increased acne formation. In this case, it can lead to an increase in the number of acne.
- Very sensitive skin. If the first signs of irritation appear, you should immediately stop using cosmetics containing urea. Ulcers may appear.
- Children's age up to 3. Such drugs are strictly contraindicated for children.
- Infectious diseases.
Benefit
Cosmetics containing synthetic urea can significantly improve skin condition . It has been scientifically proven that it can relieve inflammation and successfully fight many viruses and various harmful bacteria. Its beneficial properties are used for such problems as:
- Prevention of skin aging . When a product with urea is applied to the skin, it penetrates into the skin, since the skin has a unique ability to absorb medicinal substances. As a result, moisture is retained and skin dryness is reduced.
- Increasing skin immunity . When using decorative cosmetics for the face with urea, the skin becomes resistant to external irritants, such as wind, cold, and ultraviolet rays.
- Pain relief . When applied to the face, hands or feet, painful symptoms disappear almost instantly. The skin becomes much softer and velvety.
- Exfoliation effect . Urea actively removes dead particles of the epidermis along with accumulated dirt, and with a combination of urea and lactic acid, you can achieve an even better result.
- Skin damage . For wounds, scratches, and burns, the drug with urea helps restore it and carefully removes damage to the skin.
What do cosmetologists say?
When the concentration of urea in the body decreases, the upper layers of the epidermis dry out, increased peeling occurs, and aging accelerates. Cosmetics use a synthetic substance with a low molecular weight. This allows them to penetrate deeper into the layers of the epidermis, taking water molecules with them.
American and French scientists have conducted a number of studies on cosmetics. The results showed that after applying preparations containing urea, the epidermis remains protected from the harmful effects of the environment for several hours. They also protect against fungal and bacterial infections.
Experts favor products containing urea. But they should be used with caution. If the slightest irritation occurs, you should refrain from using them. Cosmetologists also say that you should not expect a miracle from ordinary creams if the skin is too dry and dehydrated. In this case, you will need a whole range of cosmetic preparations and regular use for a long time.
Topical use of urea in skin care: a review
Leonardo Celleno, Catholic University of the Sacred Heart, Rome, Italy, WILEY Dermatological Therapy, July 19, 2022, DOI: 10.1111/dth.12690
Impaired barrier function has been associated with a number of skin diseases, including xerosis, atopic dermatitis and psoriasis. Urea, a component of the skin's natural moisturizing factor, plays an important role in maintaining skin hydration and integrity. Several studies have examined the effects of urea in clinical settings. In this article, we summarize the available clinical evidence on the effects of urea in maintaining skin health and treating skin diseases. At lower doses (≤10%), topical urea preparations act as a skin moisturizer, while at higher concentrations (>10% urea), urea-based preparations have a keratolytic effect. (eg, Aquapiling (aquapiling.net)) Urea is also useful in combination therapy with anti-inflammatory and antifungal drugs due to its activity as a penetration enhancer.
KEYWORDS
atopic dermatitis, ichthyosis vulgaris, keratolytic agent, moisturizer, onychomycosis, psoriasis, topical urea, xerosis
The role of the skin is to protect the body from harmful environmental influences while maintaining appropriate mechanical properties, including elasticity. Healthy skin is characterized by effective control of water loss, allowing it to maintain a good level of hydration and therefore a strong physical and chemical barrier (Verdier-Sévrain & Bonté, 2007).
Urea is a polar, hygroscopic molecule produced endogenously by the human body and found naturally in the skin. Urea is formed from the metabolism of proteins and other organic nitrogen compounds and is excreted in urine and sweat (Kapuscinska & Nowak, 2014; Mosher, 1933). As one of the components of natural moisturizing factor (NMF), urea helps maintain healthy skin hydration levels. Despite the constant discovery of new ingredients and new skin care formulations, urea still remains one of the most useful molecules available to dermatologists due to its molecular and functional characteristics. In this article, we present a review of the clinical evidence supporting the use of urea to maintain skin integrity and treat diseases associated with skin barrier dysfunction.
The stratum corneum (SC), the outermost layer of the skin, protects the body from external agents and controls exchanges with the environment, especially transepithelial water loss (TEWL). The structural organization of the stratum corneum and the presence of hygroscopic molecules, collectively called NMF, allow the stratum corneum to retain water, thus keeping the epidermis hydrated and elastic. The stratum corneum consists of terminally differentiated keratinocytes called corneocytes, which are arranged in dense layers and are united by corneodesmosomes. Corneocytes are embedded in a hydrophobic lipid extracellular matrix, the keratinized cell envelope (Pouillot, Dayan, Polla, Polla, & Polla, 2008). Although the barrier created by the stratum corneum is similar in structure to a brick wall, it is more dynamic and complex in nature (Elias, 1983). In fact, the keratinized cell membrane surrounding the nondividing keratin-filled corneocytes represents an active environment consisting of enzymes involved in epidermal differentiation and NMF formation (Pouillot et al., 2008).
Adequate levels of hydration are necessary to maintain skin mechanical properties such as strength, flexibility, and elasticity (Mojumdar, Pham, Topgaard, & Sparr, 2017). In vivo, normal hydration levels range from 30–50% of the dry weight of the stratum corneum (Caspers, Lucassen, Carter, Bruining, & Puppels, 2001). Water found in the stratum corneum is mainly absorbed by corneocytes, which can increase their weight when swollen by up to 50% (Richter, Müller, Schwarz, Wepf, & Wiesendanger, 2001; Mojumdar et al., 2017). Under low relative humidity (RH) conditions, the stratum corneum is brittle and brittle, becoming more elastic as relative humidity increases (Mojumdar et al., 2017). Changes in relative humidity also alter the mobility of keratin filaments present in corneocytes, thereby supporting the role of water in keratin plasticization (Mojumdar et al., 2017).
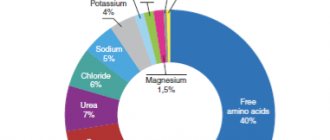
NMF is critical to maintaining a healthy stratum corneum as it plays an important role in skin hydration (Robinson, Visscher, Laruffa, & Wickett, 2010). A decrease in NMF levels causes water loss in the stratum corneum and reduces the elasticity of the epidermis (Verdier-Sévrain & Bonté, 2007). NMF consists of molecules that are formed from the breakdown of proteins or are secreted by the sebaceous and sweat glands. The detailed composition of NMF is depicted in Figure 1. Degradation of filaggrin, a keratin-aggregating protein of the keratinized cell membrane that is formed during keratinocyte differentiation (Simon et al., 1996; Kezic, Kammeyer, Calkoen, Fluhr, & Bos, 2009), results in the formation of hygroscopic amino acids and other by-products including urea (Björklund et al., 2014). In a healthy stratum corneum, urea corresponds to 7% NMF, a percentage that decreases with age (Verdier-Sévrain & Bonté, 2007).
NMF components (%)
Clockwise: free amino acids; pyrrolidonecarboxylic acid; lactate; Sahara; urea; chlorides; sodium; potassium; ammonia, uric acid, glucosamine, creatinine; calcium; phosphates; citrate and formate.
FIGURE 1 Chemical composition of NMF. Data from (Verdier-Sévrain & Bonté, 2007)
The moisturizing effects of urea have been studied in vivo for many years (Serup, 1992; Bettinger, Gloor, Gehring, & Wolf, 1995; Treffel & Gabard, 1995; Loden, 1996, 1997; Kuzmina, Hagströmer, & Emtestam, 2002); Grether-Beck, Mühlberg, Brenden, & Krutmann, 2008; Borelli, Bielfeldt, Borelli, Schaller, & Korting, 2011). Pan and colleagues analyzed these clinical data in 2013 (Pan, Heinecke, Bernardo, Tsui, & Levitt, 2013). Urea has been noted to reduce transepidermal water loss (Loden, 1996, 1997; Borelli et al., 2011), improve hydration (Borelli et al., 2011) and water retention (Treffel & Gabard, 1995). In addition, urea can increase the amount of free water under high humidity conditions (Bettinger et al., 1995) and act as a powerful skin moisturizer and exfoliant (Serup, 1992).
Of note is the fact that all of these clinical studies used topical cream, emulsion or foam formulations with a urea concentration of 10% or less. No adverse events were reported, confirming the safety of topical urea-based products.
Urea increases the water content of the stratum corneum, acting as a humectant but also by maintaining the fluidity of the stratum corneum (Albèr et al., 2014; Mojumdar et al., 2017). By measuring corneometry, Albèr et al. found that urea promoted skin hydration even when used in a formulation with reduced water activity (Albèr et al., 2014). A subsequent study examined the molecular characteristics of keratin and macroscopic properties of the stratum corneum (SC) after the addition of urea to dehydrated SCs and corneocytes and found that the changes were similar to those occurring with increasing relative humidity in the absence of urea (Mojumdar et al., 2017) . These data support the hypothesis that urea acts as a natural endogenous humectant, replacing water under low-humidity conditions and maintaining fluid levels within the stratum corneum (Mojumdar et al., 2017). At higher concentrations (>10%) (eg Aquapiling (aquapiling.net)) urea has an emollient/keratolytic effect. The first evidence came from Swanbeck's studies in the 60s. These studies showed that preparations with high concentrations of urea could be used to treat ichthyosis and other hyperkeratotic conditions (Swanbeck, 1968a, 1968b; Swanbeck & Rajka, 1970). Swanbeck suggested that at high concentrations, urea is able to dissolve keratin, promoting the destruction of hydrogen bonds. Further studies showed that urea can cause conformational changes in keratin, causing denaturation of the protein structure (Pan et al., 2013).
In addition to its moisturizing properties, preserving the fluidity of SK and promoting keratin denaturation, urea is also able to participate in the regulation of gene expression (Friedman, von Grote, & Meckfessel, 2016). In a study by Grether-Beck et al. indicates that urea induces the expression of epidermal genes (Grether-Beck et al., 2012). Although more research is needed to better understand the involvement of urea in the regulation of gene expression in SK, the active role of urea as an inducer of epidermal gene expression may explain the beneficial effects of urea in preserving skin barrier function.
Keratinization disorders are characterized by qualitative or quantitative changes in the structure of the stratum corneum. Urea, used alone or in combination therapy, improves the treatment of pathological conditions including xerosis, atopic dermatitis, ichthyosis vulgaris, psoriasis and onychomycosis (Pan et al., 2013).
Xerosis or dry skin may be the result of dehydration or changes in lipid production. Dehydrated skin, typical of older people, whose tissues lack water - thin, weak and fragile. Low sebum levels and abnormal lipid levels in the epidermis (as in atopic dermatitis) make the skin tender, opaque, red, and hypersensitive to external agents. In both cases, topical formulations containing urea play an important role in the treatment of diseases. When used in low doses (mostly <10%, one study used 40% urea), urea regulates transepidermal water loss (TEWL) and restores the ability of the stratum corneum to mobilize and maintain hydration (Pan et al., 2013; Danby et al., 2016). Moisturizers containing urea improve fissure healing in diabetic patients (Federici, Federici, & Milani, 2015; Gin et al., 2017). Open heel cracks allow bacteria to enter and can lead to infections and further complications. Additionally, a skin care routine that includes a moisturizing step stops the progression of dry skin diseases, including epidermal hyperproliferation and inflammation (Friedman, von Grote, & Meckfessel, 2016).
From top to bottom, left to right: topical urea formulations; ≤10% urea, moisturizing effect, positive effect on xerosis, AD, IV, psoriasis; ≥10% urea, keratolytic effect, positive effect on psoriasis, onychomycosis; useful in quality; monotherapy; combination therapy, urea – enhances the penetration of corticosteroids, salicylic acid and antifungal drugs.
FIGURE 2 Overview of known effects of topical urea formulations in clinical settings. AD, topical dermatitis; IV, ichthyosis vulgaris
Skin barrier dysfunction has been associated with an increased risk of developing atopic dermatitis (AD) (Egawa & Kabashima, 2018). A weakened skin barrier makes it easier for allergens and other external agents to penetrate and predisposes the body to inflammation. If skin inflammation persists, barrier function is further compromised (Egawa & Kabashima, 2018). AD is the most common inflammatory skin disease, affecting up to 30% of children worldwide (Bieber, 2008). AD is a cutaneous manifestation of a genetic predisposition to allergies and is characterized by highly itchy and recurrent skin lesions on dry skin (Egawa & Kabashima, 2018). Adequate hydration of the stratum corneum appears to be critical in preventing AD, as the use of moisturizers in neonates reduces the prevalence of the disease (Horimukai et al., 2014; Simpson et al., 2014).
Several clinical trials have examined the clinical effects of topical urea formulations in AD (Pan et al., 2013). At a concentration of 10%, urea has been found to improve skin hydration and reduce transepidermal water loss (TEWL) in patients with AD (Sasaki, Tadaki, & Tagami, 1989). However, two recent studies suggest that urea increases skin hydration in AD without reducing TEWL (Hoppe et al., 2015; Ahmad Nasrollahi et al., 2018). These conflicting results can be explained by the low concentration of urea used in the formulations used (only 5%).
Clinical benefit of urea in AD has been observed when used alone and in combination with hydrocortisone or betamethasone-17 valerate (Bohnsack, Tausch, Gassmuller, & Rippke, 1997; Wilhelm, Scholermann, & Bohnsack, 1998; Loden et al., 2002; Wirén et al. al., 2009; Pan et al., 2013). It should be noted that combination therapy with urea was more effective than treatment with hydrocortisone or betamethasone-17-valerate alone (Pan et al., 2013). A recent Cochrane review confirmed that for AD, treatment with moisturizers and topical corticosteroids is more effective than treatment with topical corticosteroids alone (Van Zuuren, Fedorowicz, & Arents, 2017). A systematic review confirmed the beneficial effects of moisturizers on AD but warned of the need for more focused studies that would allow direct comparisons of moisturizers (Lindh & Bradley, 2015). Meanwhile, available evidence supports the use of urea-containing moisturizers as first-line therapy for AD (Lindh & Bradley, 2015).
Ichthyosis vulgaris (IV) is a genetic disorder with a prevalence of 1:300 caused by loss-of-function mutations in the filaggrin gene (FLG) (Brown & McLean, 2012). IV is characterized by flaky, dry skin with symmetrical white or gray scales. Peeling occurs due to the absence of filaggrin protein in the stratum corneum, which causes low cellular regeneration of the stratum corneum and chronic accumulation of keratin. A recent systematic review concluded that urea-containing drugs should be used as first-line therapy for ichthyosis vulgaris (Lindh & Bradley, 2015). Maintenance therapy using 10% urea is noninferior to therapy containing 1% hydrocortisone, 2% salicylic acid, or paraffin moisturizers (Pan et al., 2013).
Psoriasis is a chronic inflammatory skin disease with a worldwide prevalence of 2% (Parisi, Symmons, Griffiths, & Ashcroft, 2013). Psoriasis is characterized by the development of erythematous scaly plaques that result from increased keratinocyte proliferation and altered epidermal differentiation (Zhang et al., 2009). Clinical trials have been conducted to study the effects of urea on psoriatic skin (Pan et al., 2013). One study found that, when used at a concentration of 10%, urea reduced transepidermal water loss (TEWL) and increased stratum corneum hydration (Sasaki, Tadaki, & Tagami, 1989). Subsequently, Hagemann and Proksch also found that urea induces epidermal differentiation (Hagemann & Proksch, 1996). When used at concentrations ranging from 10 to 40%, alone or in combination with bifonazole or dithranol, most studies reported improvement in desquamation and clinical status in patients with psoriasis (Pan et al., 2013). (for example, Aquapiling (aquapiling.net))
At a concentration of 40%, urea shows clinical effects in the treatment of fungal nail infections such as onychomycosis (Pan et al., 2013). Topical treatment with fluconazole 1% and urea 40% is more effective than fluconazole alone in the treatment of onychomycosis (Bassiri-Jahromi, Ehsani, Mirshams-Shahshahani, & Jamshidi, 2012). Urea enhances the penetration of the antifungal agent and thus enhances the therapeutic effect (Pan et al., 2013). (for example, Cream-paste for corns Aquapiling (aquapiling.net))
Urea can be considered a penetration enhancer due to its ability to facilitate the transport of molecular flow through the nail and skin (Trommer & Neubert, 2006). These molecules include the aforementioned antifungal drugs, as well as other compounds used in the treatment of skin diseases, such as corticosteroids (Trommer & Neubert, 2006). An earlier study by Ayres and Hooper examined the potentiating effects of urea on skin penetration of cortisol (Ayres & Hooper, 1978). The authors observed that a topical formulation containing 1.0% cortisol and 10% urea delivered eight times more cortisol to the skin than a topical cream used as a control (1.0% cortisol cream mixed with water). Subsequent studies showed that urea enhances the penetration of hydrocortisone, progesterone and leuprolide through the subcutaneous tissue (Trommer & Neubert, 2006). It is noteworthy that in an in vitro study examining transcutaneous diffusion of progesterone, urea increased progesterone penetration by 2.5-fold (Valenta & Wedenig, 1997).
The mechanism by which urea increases the permeability of the stratum corneum is not fully understood, but it is thought to be related to the ability to increase the water content absorbed by corneocytes, which is a direct consequence of its high water-binding capacity (Mueller et al., 2016). At higher doses, the keratolytic action of urea may also play a role in enhancing drug penetration (Trommer & Neubert, 2006). Because of its recognized action as a chemical penetration enhancer, urea should be used in conjunction with topical corticosteroids, salicylic acid, or antifungals to improve drug delivery and treatment outcomes.
Urea is a well-known moisturizer and keratolytic agent. Urea has been used safely for over a century to support skin health and treat a range of skin conditions. Clinical studies have confirmed the positive effect of urea in diseases associated with skin barrier dysfunction. When used in different concentrations, urea has different effects (Fig. 2). Lower concentrations of urea (≤10%) are associated with a moisturizing effect, whereas higher concentrations (>10%) have an emollient/keratolytic effect. As a skin penetration enhancer, urea facilitates the crossing of the skin barrier by other molecules and thus improves the action of drugs used in combination therapy. Topical formulations containing urea are available in a variety of concentrations and provide clinicians with a wide range of alternatives to enhance the treatment of skin conditions and improve patient well-being.
Medical writing and editing support was provided by Raquel Carvalhosa, Ph.D., and . Financial support for the compilation and editing of medical texts was provided by.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ORCID Leonardo Celleno https://orcid.org/0000-0002-7129-198X
REFERENCES
Ahmad Nasrollahi, S., Ayatollahi, A., Yazdanparast, T., Samadi, A., Hosseini, H., Shamsipour, M., … Firooz, A. (2018). Comparison of linoleic acid-containing water-in-oil emulsion with urea-containing water-in-oil emulsion in the treatment of atopic dermatitis: A randomized clinical trial. Clinical Cosmetic and Investigational Dermatology, 11, 21–28. https://doi.org/10.2147/CCID.S145561 Albèr, C., Buraczewska-Norin, I., Kocherbitov, V., Saleem, S., Lodén, M., & Engblom, J. (2014). Effects of water activity and low molecular weight humectants on skin permeability and hydration dynamics—a double-blind, randomized and controlled study. International Journal of Cosmetic Science, 36(5), 412–418. https://doi.org/10.1111/ics.12136 Ayres, P. J., & Hooper, G. (1978). Assessment of the skin penetration properties of different carrier vehicles for topically applied cortisol. British Journal of Dermatology, 99(3), 307–317. https://doi.org/10.1111/j. 1365-2133.1978.tb02002.x Bassiri-Jahromi, S., Ehsani, A.H., Mirshams-Shahshahani, M., & Jamshidi, B. (2012). A evaluation comparative of combination therapy of fluconazole 1% and urea 40% compared with fluconazole 1% alone in a nail lacquer for treatment of onychomycosis: Therapeutic trial. Journal of Dermatological Treatment, 23(6), 453–456. https://doi. org/10.3109/09546634.2011.588191 Bettinger, J., Gloor, M., Gehring, W., & Wolf, W. (1995). Influence of emulsions with and without urea on water-binding capacity of the stratum corneum. Journal of the Society of Cosmetic Chemists, 46(5), 247–254. Bieber, T. (2008). Atopic dermatitis. New England Journal of Medicine, 358(14), 1483–1494. https://doi.org/10.1056/NEJMra074081 Björklund, S., Andersson, J. M., Pham, Q. D., Nowacka, A., Topgaard, D., & Sparr, E. (2014). Stratum corneum molecular mobility in the presence of natural moisturizers. Soft Matter, 10(25), 4535–4546. https://doi. org/10.1039/C4SM00137K Bohnsack, K., Tausch, I., Gassmuller, J., & Rippke, F. (1997). Efficacy on the symptom “dry skin” and long-term dermal tolerance of Laceran lotion 10% urea in patients with atopic dermatitis. Zeitschrift für Hautkrankheiten, 72, 34–39. Borelli, C., Bielfeldt, S., Borelli, S., Schaller, M., & Korting, H. C. (2011). Cream or foam in pedal skin care: Towards the ideal vehicle for urea used against dry skin. International Journal of Cosmetic Science, 33(1), 37–43. https://doi.org/10.1111/j.1468-2494.2010.00576.x Brown, S. J., & McLean, W. H. I. (2012). One remarkable molecule: filaggrin. The Journal of Investigative Dermatology, 132(3 Pt 2), 751–762. https://doi.org/10.1038/jid.2011.393 Caspers, P. J., Lucassen, G. W., Carter, E. A., Bruining, H. A., & Puppels, G. J. (2001). In vivo confocal Raman microspectroscopy of the skin: Noninvasive determination of molecular concentration profiles. The Journal of Investigative Dermatology, 116(3), 434–442. https://doi. org/10.1046/j.1523-1747.2001.01258.x Danby, S. G., Brown, K., Higgs-Bayliss, T., Chittock, J., Albenali, L., & Cork, M. J. (2016). The effect of an emollient containing urea, ceramide NP, and lactate on skin barrier structure and function in older people with dry skin. Skin Pharmacology and Physiology, 29(3), 135–147. https://doi.org/10.1159/000445955 Egawa, G., & Kabashima, K. (2018). Barrier dysfunction in the skin allergy. Allergology International, 67(1), 3–11. https://doi.org/10.1016/j.alit. 2017.10.002 Elias, P. M. (1983). Epidermal lipids, barrier function, and desquamation. The Journal of Investigative Dermatology, 80(Suppl), 44s–49s. Federici, A., Federici, G., & Milani, M. (2015). Use of a urea, arginine and carnosine cream versus a standard emollient glycerol cream for treatment of severe xerosis of the feet in patients with type 2 diabetes: A randomized, 8 month, assessor-blinded, controlled trial. Current Medical Research and Opinion, 31(6), 1063–1069. https://doi.org/10. 1185/03007995.2015.1037731 Friedman, A. J., von Grote, E. C., & Meckfessel, M. H. (2016). Urea: A clinically oriented overview from bench to bedside. Journal of Drugs in Dermatology: JDD, 15(5), 633–639. Gin, H., Rorive, M., Gautier, S., Condomines, M., Saint Aroman, M., & Garrigue, E. (2017). Treatment by a moisturizer of xerosis and cracks of the feet in men and women with diabetes: A randomized, double-blind, placebo-controlled study. Diabetic Medicine, 34(9), 1309–1317. https://doi.org/10.1111/dme.13402 Grether-Beck, S., Felsner, I., Brenden, H., Kohne, Z., Majora, M., Marini, A., … Krutmann, J. (2012). Urea uptake enhances barrier function and antimicrobial defense in humans by regulating epidermal gene expression. Journal of Investigative Dermatology, 132(6), 1561–1572. https://doi. org/10.1038/jid.2012.42 Grether-Beck, S., Mühlberg, K., Brenden, H., & Krutmann, J. (2008). Urea plus ceramides and vitamins: Improving the efficacy of a topical urea preparation by addition of ceramides and vitamins. Der Hautarzt; Zeitschrift Fur Dermatologie, Venerologie, Und Verwandte Gebiete, 59(9), 717–718, 720–723. https://doi.org/10.1007/s00105-008-1594-z Hagemann, I., & Proksch, E. (1996). Topical treatment by urea reduces epidermal hyperproliferation and induces differentiation in psoriasis. Acta Dermato-Venereologica, 76(5), 353–356. Hoppe, T., Winge, M. C. G., Bradley, M., Nordenskjöld, M., Vahlquist, A., Törmä, H., & Berne, B. (2015). Moisturizing treatment of patients with atopic dermatitis and ichthyosis vulgaris improves dry skin, but has a modest effect on gene expression regardless of FLG genotype. Journal of the European Academy of Dermatology and Venereology, 29(1), 174–177. https://doi.org/10.1111/jdv.12333 Horimukai, K., Morita, K., Narita, M., Kondo, M., Kitazawa, H., Nozaki, M., … Ohya, Y. (2014 ). Application of moisturizer to neonates prevents development of atopic dermatitis. The Journal of Allergy and Clinical Immunology, 134(4), 824–830.e6. https://doi.org/10.1016/j.jaci.2014.07.060 Kapuscinska, A., & Nowak, I. (2014). The use of urea and its derivatives in the cosmetics industry. CHEMIK, 68(2), 91–98. Kezic, S., Kammeyer, A., Calkoen, F., Fluhr, J. W., & Bos, J. D. (2009). Natural moisturizing factor components in the stratum corneum as biomarkers of filaggrin genotype: Evaluation of minimally invasive methods. British Journal of Dermatology, 161(5), 1098–1104. https:// doi.org/10.1111/j.1365-2133.2009.09342.x Kuzmina, N., Hagströmer, L., & Emtestam, L. (2002). Urea and sodium chloride in moisturisers for skin of the elderly—a comparative, double-blind, randomized study. Skin Pharmacology and Applied Skin Physiology, 15(3), 166–174. https://doi.org/10.1159/000063545 Lindh, J. D., & Bradley, M. (2015). Clinical effectiveness of moisturizers in atopic dermatitis and related disorders: A systematic review. American Journal of Clinical Dermatology, 16(5), 341–359. https://doi.org/10. 1007/s40257-015-0146-4 Loden, M. (1996). Urea-containing moisturizers influence barrier properties of normal skin. Archives of Dermatological Research, 288(2), 103–107. Loden, M. (1997). Barrier recovery and influence of irritant stimuli in skin treated with a moisturizing cream. Contact Dermatitis, 36(5), 256–260. Loden, M., Andersson, A.-C., Anderson, C., Bergbrant, I.-M., Frödin, T., Ohman, H., … Lindberg, M. (2002). A double-blind study comparing the effect of glycerin and urea on dry, eczematous skin in atopic patients. Acta Dermato-Venereologica, 82(1), 45–47. Mojumdar, E. H., Pham, Q. D., Topgaard, D., & Sparr, E. (2017). Skin hydration: Interplay between molecular dynamics, structure and water uptake in the stratum corneum. Scientific Reports, 7(1), 15712. https:// doi.org/10.1038/s41598-017-15921-5 Mosher, H. H. (1933). Simultaneous study of constituents of urine and perspiration. Journal of Biological Chemistry, 99, 781. Mueller, J., Oliveira, J. S. L., Barker, R., Trapp, M., Schroeter, A., Brezesinski, G., & Neubert, R. H. H. (2016). The effect of urea and taurine as hydrophilic penetration enhancers on stratum corneum lipid models. Biochimica et Biophysica Acta (BBA) - Biomembranes, 1858(9), 2006–2018. https://doi.org/10.1016/j.bbamem.2016.05.010 Pan, M., Heinecke, G., Bernardo, S., Tsui, C., & Levitt, J. (2013). Urea: A comprehensive review of the clinical literature. Dermatology Online Journal, 19(11), 20392. Parisi, R., Symmons, D. P. M., Griffiths, C. E. M., & Ashcroft, D. M. (2013). Global epidemiology of psoriasis: A systematic review of incidence and prevalence. Journal of Investigative Dermatology, 133(2), 377–385. https://doi.org/10.1038/jid.2012.339 Pouillot, A., Dayan, N., Polla, A. S., Polla, L. L., & Polla, B. S. (2008). The stratum corneum: A double paradox. Journal of Cosmetic Dermatology, 7(2), 143–148. https://doi.org/10.1111/j.1473-2165.2008.00379.x Richter, T., Müller, J. H., Schwarz, U. D., Wepf, R., & Wiesendanger, R. (2001). Investigation of the swelling of human skin cells in liquid media by tapping mode scanning force microscopy. Applied Physics A, 72(S1), S125–S128. https://doi.org/10.1007/s003390100750 Robinson, M., Visscher, M., Laruffa, A., & Wickett, R. (2010). Natural moisturizing factors (NMF) in the stratum corneum (SC). I. Effects of lipid extraction and soaking. Journal of Cosmetic Science, 61(1), 13–22. Sasaki, Y., Tadaki, T., & Tagami, H. (1989). The effects of topical application of urea cream on the function of pathological stratum corneum. Acta Dermatol-Kyoto, 84(4), 581–586. Serup, J. (1992). A three-hour test for rapid comparison of effects of moisturizers and active constituents (urea). Measurement of hydration, scaling and skin surface lipidization by noninvasive techniques. Acta Dermato-Venereologica. Supplementum, 177, 29–33. Simon, M., Haftek, M., Sebbag, M., MontéZin, M., Girbal-Neuhauser, E., Schmitt, D., & Serre, G. (1996). Evidence that filaggrin is a component of cornified cell envelopes in human plantar epidermis. Biochemical Journal, 317(1), 173–177. https://doi.org/10.1042/bj3170173 Simpson, E. L., Chalmers, J. R., Hanifin, J. M., Thomas, K. S., Cork, M. J., McLean, W. H. I., … Williams, H. C. (2014). Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. Journal of Allergy and Clinical Immunology, 134(4), 818–823. https:// doi.org/10.1016/j.jaci.2014.08.005 Swanbeck, G. (1968a). A new treatment of ichthyosis and other hyperkeratotic conditions. Acta Dermato-Venereologica, 48(2), 123–127. Swanbeck, G. (1968b). Carbamide cream for dry and hyperkeratotic skin. Läkartidningen, 65(22), 2286–2290. Swanbeck, G., & Rajka, G. (1970). Antipruritic effect of urea solutions. An experimental and clinical study. Acta Dermato-Venereologica, 50(3), 225–227. Treffel, P., & Gabard, B. (1995). Stratum corneum dynamic function measurements after moisturizer or irritant application. Archives of Dermatological Research, 287(5), 474–479. Trommer, H., & Neubert, R. H. (2006). Overcoming the stratum corneum: The modulation of skin penetration. A review. Skin Pharmacology and Physiology, 19(2), 106–121. https://doi.org/10.1159/000091978 Valenta, C., & Wedenig, S. (1997). Effects of penetration enhancers on the in-vitro percutaneous absorption of progesterone. Journal of Pharmacy and Pharmacology, 49(10), 955–959. https://doi.org/10.1111/j.2042-7158. 1997.tb06023.x Van Zuuren, E. J., Fedorowicz, Z., & Arents, B. W. M. (2017). Emollients and moisturizers for eczema: Abridged Cochrane systematic review including GRADE assessments. British Journal of Dermatology, 177(5), 1256–1271. https://doi.org/10.1111/bjd.15602 Verdier-Sévrain, S., & Bonté, F. (2007). Skin hydration: A review on its molecular mechanisms. Journal of Cosmetic Dermatology, 6(2), 75–82. https://doi.org/10.1111/j.1473-2165.2007.00300.x Wilhelm, K. P., Scholermann, A., & Bohnsack, K. (1998). Efficacy and tolerance of a topical preparation containing 10% urea in patients with atopic dermatitis. Aktuelle Dermatologie, 24, 26–30. Wirén, K., Nohlgård, C., Nyberg, F., Holm, L., Svensson, M., Johannesson, A., … Lodén, M. (2009). Treatment with a barrier-strengthening moisturizing cream delays relapse of atopic dermatitis: A prospective and randomized controlled clinical trial. Journal of the European Academy of Dermatology and Venereology, 23(11), 1267–1272. https://doi.org/10. 1111/j.1468-3083.2009.03303.x Zhang, X.-J., Huang, W., Yang, S., Sun, L.-D., Zhang, F.-Y., Zhu, Q.- X., ... Liu, J.-J. (2009). Psoriasis genome-wide association study identifies susceptibility variants within LCE gene cluster at 1q21. Nature Genetics, 41(2), 205–210. https://doi.org/10.1038/ng.31
Foot cream EVO with urea 10%
Available in tubes of 50 g. Price – 80 – 120 rubles.
It has a slightly runny, greasy consistency. On the feet it is completely absorbed in about 10-15 minutes. Moisturizes dry, cracked heels. Makes it smooth, without rough burrs. Of course, it doesn’t get rid of rough corns, but overall it does a good job of moisturizing. The only downside is that it runs out quickly.
Characteristics of the substance
Urea is a derivative of carbonic acid with a melting point of 132.7 degrees Celsius , highly soluble in water, methanol, ethanol. It was first discovered in urine, so it was called urea. It is the final product of protein breakdown in the human body, the body of most animals, and fungi. Its chemical properties resemble amides of carboxylic acids, but with more pronounced nucleophilic properties of the nitrogen atom.
Urea is widely used in agriculture as a feed additive and as a nitrogen fertilizer, as well as in the medical and cosmetic industries for the production of moisturizing creams.
The humectants included in such products have the unique ability to increase or retain water in the upper layer of the skin. Some of them are hygroscopic, meaning they can absorb water. These substances include urea, or urea in other words.
Night face cream with urea Balea Nachtcreme mit 5% Urea
Volume – 50 ml. Cost – 200-250 rubles.
Contains 5% urea, shea and olive oils, vitamin E. It has a light texture, not too greasy like other night creams. After applying it, a slight tingling sensation may be felt for 5-7 minutes. The next morning the skin feels great - the color becomes even and acquires a smooth texture. You can feel the moisturizing effect.
Possible harm
Urea, despite its beneficial properties, can be harmful:
- Cause allergies. Urea is a fairly strong allergen and can cause a rash, severe irritation, and itchy skin. Peeling is also possible.
- Increase sebum secretion. Those with oily skin types should not use cosmetics containing urea in large quantities, as urea causes increased sebum production.
- Cause acne. Pimples on the skin may appear due to increased sebum secretion or be a consequence of allergies.
Cream for very dry skin Emolium Cream
Volume – 75 ml. Price – 500 – 550 rub.
Contains shea and macadamia butter, 3% urea. Developed in collaboration with dermatologists. It has a light, non-greasy consistency and is well absorbed. It is even indicated for use in atopic and other dermatitis. Perfectly moisturizes very dry skin, the effect after application lasts for a long time.
Facial scrub Clean Line
Volume – 50 ml. Cost 75 – 90 rub.
This remedy enjoys mixed popularity. Some people adore it, others criticize it for its too large particles of seeds that scratch the skin. The scrub has a creamy texture with an unobtrusive aroma. Contains soybean and corn oils and lots of abrasive ground kernels. The manufacturer positions it as a panacea for cleansing the deep layers of the epidermis, but it is unlikely that the scrub is capable of this. An undoubted advantage is the absence of a feeling of tightness and dryness. Removes dead cells very well.