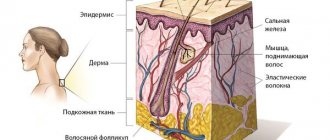
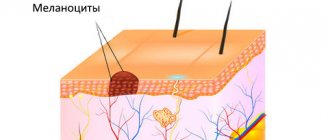
Birthmarks, moles of various sizes and shapes or nevi are accumulations of melanocytes - pigment cells. By producing melanin, these cells protect human skin from exposure to ultraviolet radiation. The skin contains two types of pigments:
- eumelanin (black pigment): promotes protection against UV rays and is a so-called “photoprotector”;
- Pheomelanin (red pigment): Often found in red-haired people, blondes and fair-skinned people, it leads to sunburn by contributing to UV damage to the skin.
Usually, nevi appear on the skin of a child, before he reaches two or three years of age (but can also develop in utero), and initially they are a small-sized pigment spot, although sometimes there are giant ones - up to 25-40 cm in diameter. Very often this formation occurs in women who are in an interesting position, which is most likely due to changes in hormonal levels.
Most often, the size of the nevus does not exceed one and a half centimeters in diameter, and its shape is an oval or a perfectly smooth circle. After its “owner” reaches puberty, it stops growing, and when the wearer reaches 40-50 years of age, it loses pigmentation, noticeably turns pale and becomes almost invisible.
Symptoms of blue nevus
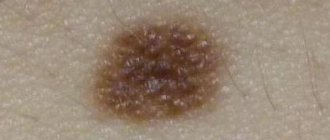
Blue nevus can appear in people of any age group, but most often it is first discovered in middle age. It usually does not cause patients any particular discomfort (except for a cosmetic defect when it is localized on the face and is large in size). Blue nevus has the following clinical characteristics:
- intradermal nodule;
- round, spindle-shaped or elliptical shape;
- light gray, dark blue, blue-black or blue color;
- uneven color;
- clear contours;
- smooth, hairless surface;
- the size rarely exceeds a centimeter (although there are blue nevi larger than 3 cm);
- protrudes slightly above the skin or does not rise above it at all;
- the consistency is elastic and dense;
- most often localized on the buttocks and limbs;
- can form on the mucous membranes of the mouth, vagina, and cervix.
Types of manifestation
This formation can have different structure, size and color:
- by structure: they are flat, warty, in the form of nodules, with a rough surface;
- by color: color varies from light brown to burgundy and black;
- by size: there are small (up to one and a half cm), medium (up to 10 cm), large (up to 20 cm) and giant (more than 20 cm in diameter) nevi.
Approximately 50% of cancerous tumors (melanomas) are formed from previous nevi and birthmarks, so if you notice these age spots, do not self-medicate and be sure to consult a dermatologist, oncologist or surgeon.
Remember: the presence of 15-20 nevi on the skin increases the risk of malignant melanoma three times! A dangerous signal is redness and soreness of the nevus, changes in its contours and size, the appearance of hair spots on the surface, flaky scales of the epidermis, bleeding, itching.
Diagnosis of blue nevus
In most cases, one visual examination by a dermatologist is sufficient to accurately verify the diagnosis. In unclear and controversial clinical cases, the following examination is recommended:
- dermatoscopy (under magnification, the boundaries, depth and structure of pigment formation are studied more carefully);
- siascopy (assessment of the structure and distribution of melanin);
- ultrasonography of the nevus (to exclude infiltrative growth of a malignant nevus);
- histological examination of biopsy specimens (rarely) or surgical material (detects characteristic accumulations of melanocytes in the deep layers of the dermis; with a simple blue nevus, the cells are rich in melanin, and with a cellular nevus, islands of large cells with a small amount of pigment are observed);
- determination of tumor markers SU100 and TA90 (to exclude the development of melanoma).
Prevention of melanoma
To avoid skin cancer, you should follow some rules:
- do not be in the open sun, especially from 10 to 16-17 hours;
- do not visit the solarium;
- wear wide-brimmed hats in the summer heat and, if possible, wear clothes made of light materials that cover the places where there are nevi;
- Do not injure the area of the pigment spot, do not irritate it with chemicals.
Do not forget: the use of ointments, creams and sprays against UV radiation does not provide one hundred percent protection against the appearance of melanoma! Take care of yourself, and if a problem occurs, contact your doctor immediately.
Therapist of the highest category, cardiologist, gastroenterologist. Menzhevitskaya Tatyana Ivanovna
Treatment of blue nevus
As a rule, doctors choose a wait-and-see approach. Patients only need to visit a dermatologist or oncologist regularly for examination. Removal of a blue nevus is necessary only if localization is unsuccessful, causing permanent injury to the formation, and if a number of alarming signs appear:
- a significant increase in its value;
- color change;
- blurred contours;
- the appearance of itching or pain.
To remove a blue nevus use:
- electrocoagulation
- cryodestruction;
- laser;
- radio wave method;
- traditional surgical excision (the nevus is removed along with 5–8 mm of intact skin surrounding it and subcutaneous fat).
Website of dermatovenerologist Betekhtin M.S.
When examining a patient, you can often find skin changes that the patient was not aware of or that did not bother him. This accidental finding was an anemic nevus in a patient who came for an examination of melanform nevi.
Anemic nevus
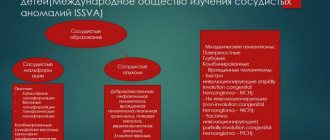
Anemic nevus is a congenital vascular anomaly that clinically manifests itself as a light spot. The reason for this is the increased sensitivity of blood vessels to catecholamines, which cause vasospasm. Judging by the reports of some authors, anemic nevus is not a common condition, occurring in 1-2% of the population (1). Early publications indicated a higher incidence of such nevus among women. But a review of the literature related to anemic nevus arising from neurofibromatosis type 1 describes an equal frequency among women and men (2). Anemic nevus can be detected at birth or in early childhood.
Evidence of vasospasm, the main cause of the appearance of nevus, is a number of the following observations. In anemic nevus, intralesional administration of bradykinin, acetylcholine, serotonin, nicotine, 5-hydroxytryptamine and histamine does not cause the expected vasodilation or redness in the affected area. If the nevus is located on the arm, sympathetic axillary blockade of the affected arm or intradermal administration of an alpha-blocker (pilocarpine) causes erythema to appear at the site of the nevus. It is also assumed that in the pathogenesis of nevus there is an abnormality in the production of endothelial adhesion molecule (expression of E selectin).
Clinically, an anemic nevus appears as an oval or linear pale spot with clear, irregular borders, which may be surrounded by satellite spots. The rashes can be single or multiple and can be located on any part of the skin, but most often they are located on the upper chest. Friction or other mechanical stress on the surrounding skin may make the stain more noticeable. Clinical manifestations of an anemic nevus usually exist without changes throughout life, and in the absence of the syndromes described below do not affect the state of health and life expectancy. If you have an anemic nevus in a child with multiple “coffee spots,” you should remember about neurofibromatosis type 1. Two prospective studies reported a 50% incidence of anemic nevus in neurofibromatosis type 1 (1,2). Anemic nevus, occupying large areas, is usually observed in close association with capillary malformations of the port-wine stain type, a phenomenon attributed to somatic recombination. Anemic nevus in combination with telangiectatic nevus may be associated with abnormalities in the development of cerebral vessels - cerebral hemiatrophy (Dyke-Davydov-Masson syndrome) (4). Anemic nevi have also been described in patients with pigmentovascular phakomatosis, a syndrome characterized by vascular and melanoform nevi (5,6). Pigmented vascular phakomatosis type IIa (according to Hazegawa and Yasuhara) is associated with primary choroidal melanoma (7).
Differential diagnosis should be made with achromic nevus, pityriasis versicolor, vitiligo, post-inflammatory hypopigmentation, tuberous sclerosis (ash leaf spots), progressive macular hypomelanosis and scars. A number of simple diagnostic procedures can clarify the diagnosis of anemic nevus. With diascopy, the nevus becomes indistinguishable from the surrounding skin, which turns pale when pressed with glass. Because There is no loss of melanin in an anemic nevus, then examination under a Wood’s lamp makes the nevus invisible, unlike true depigmenting conditions. Friction, cold or heat do not cause changes in these nevi. When attempting to induce dermatographism by drawing a line through the nevus and surrounding skin, erythema occurs only on the surrounding skin and not on the nevus itself.
Treatment for anemic nevus is not required. If necessary, the patient can apply camouflage agents. There is no cure.
1. Marque M, Roubertie A, Jaussent A, Carneiro M, Meunier L, Guillot B, et al. Nevus anemicus in neurofibromatosis type 1: a potential new diagnostic criterion. J Am Acad Dermatol. 2013 Nov. 69(5):768-75. [Medline].
2. Hernández-Martín A, García-Martínez FJ, Duat A, López-Martín I, Noguera-Morel L, Torrelo A. Nevus anemicus: a distinctive cutaneous finding in neurofibromatosis type 1. Pediatr Dermatol. 2015 May-Jun. 32 (3):342-7. [Medline].
3. Ferrari F, Masurel A, Olivier-Faivre L, Vabres P. Juvenile xanthogranuloma and nevus anemicus in the diagnosis of neurofibromatosis type 1. JAMA Dermatol. 2014 Jan. 150(1):42-6. [Medline].
4. Ruggieri M, Polizzi A, Strano S, Schepis C, Morano M, Belfiore G, et al. Mixed vascular nevus syndrome: a report of four new cases and a literature review. Quant Imaging Med Surg. 2016 Oct. 6(5):515-524. [Medline].
5. Ahkami RN, Schwartz RA. Nevus anemicus. Dermatology. 1999. 198(4):327-9. [Medline].
6. Castori M, Rinaldi R, Angelo C, Zambruno G, Grammatico P, Happle R. Phacomatosis cesioflammea with unilateral lipohypoplasia. Am J Med Genet A. 2008 Feb 15. 146A(4):492-5. [Medline].
7. Tran HV, Zografos L. Primary choroidal melanoma in phakomatosis pigmentovascularis IIa. Ophthalmology. 2005 Jul. 112(7):1232-5. [Medline].
Is it possible to remove moles?
This decision is preceded by a consultation with a qualified dermatologist, dermoscopy and biopsy. If the research results confirm the presence of atypical cells, then the next step is removal of the melanoma. Dermatologist-surgeons can offer several options for the procedure:
- traditional surgical methods;
- modern electrocoagulation using the Surgitron device;
- cryodestruction. Freezing the tumor with liquid nitrogen at a temperature of 196˚.
Dermatologists categorically prohibit burning, tearing out or cutting off moles on their own. Such trauma increases the chances of developing melanoma.
How are nevi (moles) formed and what is their danger?
Nevi appear from pigment cells (melanocytes) at the border between the dermis and the epithelial layer of the skin. Due to external factors (ultraviolet) or internal (hormones), melanin accumulates in a certain area, forming a flat or convex brown neoplasm - a mole.
Nevi themselves are not dangerous. But if the neoplasm is constantly injured (for example, rubbed by clothing), ultraviolet light or chemicals come into contact with it, then there is a risk of the mole degenerating into melanoma (skin cancer).
How to prevent melanomas
- Minimizing the influence of ultraviolet radiation during active hours. Dermatologists do not recommend opening areas with moles between 11 a.m. and 4 p.m. Active sun rays can trigger the degeneration of ordinary pigmented areas into melanoma. If you need to go outside at this time, cover your skin with nevi with light, light fabrics and hats.
- Use of sunscreens. For people of the first and second color types, it is mandatory to use cosmetics with spf 30. Creams, mousses, and sprays create a protective film against ultraviolet radiation for 30-60 minutes.
- Avoid traumatizing moles. If the nevus is located in such an area that it is constantly injured (rubbed by a shirt collar, scratched when shaving, pressed by straps and underwear straps), then it is better to have it removed by a dermatologist.
- Get your moles examined annually by a dermatologist. If you have fair skin with multiple nevi, then dermatologists advise undergoing a dermatological examination every six months. An unscheduled visit to a specialist is needed when the nevus begins to bleed or hurt.
For your peace of mind, a dermatologist will diagnose the mole, talk about the causes, symptoms, methods of treatment and prevention of melanoma-dangerous nevi. Sign up for a consultation by phone: 483-21-78
What are the complications?
There are several life-threatening complications associated with Ota9 nevus. One risk factor includes the development of malignant melanoma, although cases are rare. A total of 60 cases of malignant melanoma arising from nevus of Ota have been described, including 10 cases involving the skin, 12 cases involving the meningus, and 40 cases involving the eye9.
In general, this melanocytosis is described as not life-threatening, but patients may suffer from emotional and psychosocial stress associated with the aesthetic defect caused by Ota nevus11,12.
What are moles?
Every child is unique, and every mole is too. From the name you can easily guess that moles are spots that are on the baby’s skin from birth. There is also a theory that identical “marks” on the body were a sign of the same genus. Some moles form before the baby is born and are immediately visible. Others are present on the skin “in theory,” but only appear some time after birth.
Moles can differ significantly from each other in appearance: some can be flat, others can be convex, some can be regular in shape, others can have uneven edges. Colors can vary from yellowish and brown to red and blue.
Most often, moles on the skin are not dangerous. Some even shrink in size or fade completely over time. In rare cases, moles can be a symptom of an underlying disease. In any case, if your baby's moles cause you concern, consult your pediatrician.
What is nevus of Ota?
Nevus of Ota is a dermal melanocytosis, first described by Hulk in 1860 and then expanded by Ota and Tanino in 19391, 10.
Clinically, it is distributed along the ophthalmic and maxillary divisions of the trigeminal nerve and presents as a bluish or gray patch on the skin2. In addition, it can also affect the mucous membrane of the eardrum, nasopharynx and palate3.
About 50% of cases are congenital, resulting from abnormal migration of melanoblastic neural tube cells along the first and second divisions of the trigeminal nerve during embryogenesis10.
Other cases occur during puberty and adulthood.
Initial hyperpigmentation may appear as a light-colored patch that worsens as the patient ages.