What consequences can occur after mole removal?
What to do
if the removed mole starts to grow again?
These and other questions about the recurrence of nevi are answered by a specialist - Sergey Aleksandrovich Tverezovsky, oncologist surgeon, candidate of medical sciences, mammologist, oncodermatologist, doctor of the highest category.
When removing moles or other skin growths, the doctor always explains to the patient the preferred method of removal and its feasibility.
Excision of a mole with a scalpel along with a flap of skin is used extremely rarely - if the nevus has a large base area (exceeds 2.5 cm) or if there is relative doubt about its benignity. In the remaining 90-95% of cases of mole removal, the oncodermatologist uses laser or radio wave methods, or a combination of both.
What problems might the patient encounter?
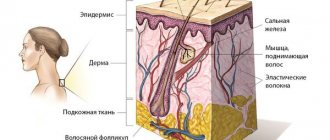
Causes of nevus recurrence
In most cases, the nevus appears again, because... the mole that existed before it was not completely removed. Some of the nevus cells remained in the skin and after some time began to actively produce brown pigment (melanin). This is what we see at the site of the mole some time after removal. At the same time, in my practice there are already 5 cases where a relapse of the nevus developed after complete removal of the mole. Why this happens and where nevus cells appear where there were none are questions that, so far, have no answer.
A scar appeared after mole removal
When excision with a scalpel, modern, atraumatic absorbable suture materials are used to eliminate a wound defect and, often, the patient cares for the wound independently.
In this case, the scars remain as aesthetically pleasing and delicate as possible, but nevertheless they are still scars. After removing a mole with a laser or electrocoagulator, the marks are usually invisible on the body (when nevi up to 5 mm are removed), or are visible, but are perceived not as scars and scars, but as minor changes in the skin (there are no associations with surgical procedures).
The appearance of a scar after mole removal depends on the properties of the patient’s skin, the size of the lesion being removed, its location, the duration of healing, and the characteristics of caring for the wound during healing.
The most unpleasant moment is the appearance of a keloid scar at the site of the removed nevus - this is a frequent reason for repeated visits and many questions. A keloid scar after removal of a mole occurs due to the predisposition of the patient’s skin, in certain areas of the body (sternum area, for example), when complications arise in the form of suppuration of the wound, or during prolonged healing due to improper care of the wound.
A keloid scar can be disturbing not only due to its sloppy appearance, but also due to pain or severe itching.
Modern technologies make it possible to correct a keloid scar. For example, we use injection correction in combination with surface laser resurfacing. If treated in a timely manner, one procedure is sufficient.
Is nevus recurrence dangerous?
In answering this question, the key point is the histological examination of the removed mole. If it was carried out and the benign quality of the formation was confirmed, a relapse is not dangerous to health.
If the removal was without histology, there is a possibility that the mole was malignant, i.e. melanoma. In this situation, the health risk increases in proportion to the lost time. The tumor remaining in the skin can begin to grow rapidly and metastasize.
In order not to create panic, I will emphasize: the likelihood of a situation with melanoma not being completely removed is not very high. However, it exists.
Are weeping moles dangerous?
If a mole on the surface of the skin begins to become weeping, this is a sign of abnormal behavior of a benign tumor; it may begin to transform into melanoma. Dangerous symptoms:
- fluid, ichor or blood oozes from under the formation;
- the formation of wet blisters on the surface of the formation and the area around it;
- changes in the size, shape and color of the nevus;
- inflammatory process with redness and swelling of the formation. The neglected condition leads to the release of pus with an unpleasant odor;
- long-healing wound;
- itching, burning, pain when touched;
- loss of hair from the birthmark, increase in the area of pigmentation.
If treatment is not started, characteristic symptoms may develop:
- increased fluid secretion;
- increased pain;
- rapid growth of nevus, change in skin color around;
- enlarged lymph nodes;
- the formation of ulcers on the surface, which can produce an unpleasant odor and pus;
- painful formations appear;
- bleeding;
- compacted structure of formations.
Melanoma grows by metastases, their signs:
- chronic obsessive cough;
- a sharp decrease in body weight;
- headache;
- muscle spasms.
The nevus begins to become wet due to the development of malignant melanoma, which manifests itself in different shades and asymmetrical shapes of nevi measuring more than 6 mm. Timely treatment will help avoid serious complications that can lead to death. The tumor can spread quickly, growing through several layers of the skin, traveling through the blood and lymphatic vessels. The liver, brain, and lungs are often affected.
If there was no histology...
Calmly remember whether the doctor performed any additional research methods. Dermatoscopy? Scraping or puncture?
If yes, with a probability of about 95%, everything is fine and this is really a relapse of the nevus, and not melanoma. It requires nothing more than observation and, most likely, will not grow or change.
If there were no other examinations or histology, it seems to me advisable to excise the relapse with mandatory histological examination.
Yes, this is not easy or pleasant, but only such a step can confirm the absence or presence of melanoma.
If a mole, which was removed without histology, not only appears again, but has grown to its previous size, you need to go to an oncologist URGENTLY.
What can the doctor recommend?
Any changes in the color, shape, size and consistency of a mole require urgent consultation with a dermatologist. The doctor will rule out malignancy of the tumor and determine what exactly caused its transformation.
Frequent trauma to a nevus increases the risk of its malignancy, so experts recommend removing neoplasms located in open areas of the body. Are you looking for where to get mole removal in the Bratislavskaya metro area? Contact our clinic! We receive experienced specialists and have the necessary equipment to carry out such a procedure. Its cost can be seen in the price list on the website or specified by phone.
All articles
5% discount Print coupon from our website
Ask your question on the website Get professional advice!
Briefly about the main thing:
Recurrence of nevus, i.e.
a brown spot at the site of removal may be hazardous to health in rare cases. The likelihood of developing melanoma after removal increases if neither dermatoscopy, nor scraping/puncture, nor histological examination were performed . If this is exactly what happened to you, please consult an oncologist about re-excision with histology.
If you still have questions about the removed mole, you can ask me in the online consultation section or come to an appointment at the address in St. Petersburg - Asafieva 7/1.
When the sun is the enemy
Probably everyone already knows that a chocolate tan has little to do with health. Ultraviolet radiation causes DNA damage and is the main cause of malignant skin tumors. The more time a person spends exposing his body to the rays, the higher the likelihood of unpleasant consequences. The activity of the sun is also important. It is no coincidence that dermatologists strongly advise not to be on the beach between 11 and 16 hours of the day, when it is most aggressive.
By the way, many scientists associate the risk of developing melanoma with the fact that in childhood and adolescence a person often received sunburn. They cause changes in melanocytes, the pigment cells of the skin, which over time lead to malignant conditions. This also explains the fact that in almost 50% of cases, melanoma develops on the legs - they are always open in children in the summer and are most exposed to solar radiation.
Lately, there has been more and more talk about the dangers of “artificial sun” – solariums. According to some reports, one session here (which is usually 5-10 minutes) is equal to a whole day on the beach! Some European countries (Germany, France and Austria) and the state of California (USA) have even banned the use of solariums for children under 18 years of age.
Of course, the sun is a source of vitamin D and a remedy for depression, but in large quantities it is the real enemy. Otherwise, the World Health Organization would not recognize ultraviolet radiation as a carcinogen on a par with arsenic, smoking and asbestos.
Symptoms of degeneration
Diagnostics to identify the malignant nature of the formation is carried out using laboratory tests. But the initial signs of degeneration are determined by some basic parameters. When a mole lightens, one may suspect the formation of pathological processes based on the following factors:
- Itching in the mole area.
- Changing its outlines.
- The occurrence of pain when pressing.
- Bloody discharge from the nevus.
- The appearance of a number of formations of the same type.
Such symptoms, observed along with a change in the color of the mole, are a serious reason to seek advice from a doctor.
Large moles on the body
Moles appear in the first year after birth or throughout life.
The size also varies, and the location on the body can be anywhere. There are several types of large moles:
- fibroepithelial - benign formations up to one and a half centimeters in size;
- Sutton's or halonevus - characterized by the presence of a colorless ring;
- melanocintar – flat moles that appear during hormonal changes;
- Becker - are more often observed in men, consist of epidermal cells;
- blue – nevus is bluish in color and small in size;
- basal – characterized by inactive pigmentation, colorless;
- warty - have a bumpy surface, consisting of tiny nodules;
- papillomatous – formed by the papilloma virus;
- red – associated with the growth of the capillary network;
- nevus of the sebaceous glands - formed due to an embryonic anomaly of tissue development;
- Port-wine stains are a vascular pathology inherent in newborns.
Some springs are completely harmless, while others can pose a danger, which is expressed in the risk of malignancy. Most of the formations must be removed. But only a doctor can determine what to do with a large mole.
Medical signs of degeneration
The acquisition of a lighter color by a mole may be a consequence of its degeneration. But there are other warning signs as well. Dermatologists have developed a special scheme that allows you to record all detected symptoms, which helps to timely track the degeneration of a mole into a malignant formation. It is called ACORD - after the first letters of the signs that should alert you:
A – asymmetry. Any two halves of a healthy nevus must be absolutely identical in shape, color, and structure.
K – edges. A sign of pathological changes are disturbances in the outline of the mole, the appearance of unevenness and blurriness.
O – coloring. Not only darkening, but also lightening of the nevus serves as an alarming signal. In a benign formation, the color is distributed evenly.
R – size. A mole that is too large in diameter or clusters of small skin growths merging together is cause for concern.
D – dynamics. This is a change in various parameters of the nevus (shape, size, color, etc.). Any pronounced dynamics forces us to pay closer attention to the mole.
How to remove more moles?
There are several ways to get rid of large nevi:
- 1. Radio wave surgery. Using a special knife, the doctor excises the formation without affecting healthy tissue. There is no risk of bleeding, disinfection is ensured, and no scars are left. The technique is safe and painless.
- 2. Electrocoagulation. Heat treatment with electric current. There may be some slight discomfort. The healing process is fast.
- 3. Laser coagulation. Modern safe and painless technique. The equipment is equipped with cooling systems, so the patient feels only a slight tingling sensation. The formation of scars is excluded.
- 4. Cryodestruction. Exposure of nevus to liquid nitrogen at extremely low temperatures. Regeneration takes longer than with other methods.
All methods, except cryodestruction, allow you to save tissue particles for sending for histology. Surgical removal is indicated for very large moles and suspected cancer. The doctor excises the pigment spot with further sutures or tissue replacement with a deep incision.
Treatment and prevention
If, in addition to lightening, no other changes occur in the nevus, then no special treatment is required. Therapy is limited to procedures that improve skin condition. This includes physical therapy and taking vitamins.
But when pathological processes develop in a mole that contribute to its darkening or lightening, complex treatment is prescribed. To identify the nature of the neoplasm, the doctor performs a puncture of the skin. If, under the influence of processes that have changed the mole, it has become malignant, external treatment is not carried out. After excision of a nevus, the risk of relapse and dangerous complications increases.
Medical statistics say that malignant degeneration of a mole occurs in 13% of cases, mainly in women.
A favorable prognosis for treatment of a cancerous tumor is possible only under the supervision of an experienced doctor. The doctor performs a histological analysis. It makes it possible to determine the degree of malignancy of the mole and prescribe the optimal course of therapy.