Red moles (angiomas) are vascular neoplasms, the diameter of which ranges from several millimeters to several centimeters. Most often, angiomas appear during fetal development (congenital angiomas), but they can also occur after birth.
Small red moles can be localized on the stomach, arms, legs, back, chest, face, neck, and also on internal organs. Depending on the shape, there are three types of red moles: dotted, cavernous and stellate.
Why do red moles appear on the body?
Red moles are formed by a large number of microscopic blood vessels (hemangiomas) and lymphatic vessels (lymphangiomas). The main reason for the appearance of red moles is dysfunction of the circulatory and lymphatic systems. Angiomas are divided according to type:
| Types of angiomas | |
| Types of angiomas depending on the morphological structure | hemangiomas that develop from blood vessels |
| lymphangiomas, which form from lymphatic vessels | |
| Types of angiomas depending on the cellular structure | monomorphic, consisting of the same type of cells |
| polymorphic, which combine several cell types | |
| Types of angiomas depending on type | simple (capillary) angioma - occurs due to the proliferation of capillaries |
| branched angioma - a branched network of dilated capillaries | |
| cavernous angioma - wide spongy cavities filled with blood | |
| combined angioma, combining cavernous and simple types | |
| Types of angiomas depending on location | spine - predominant location in the thoracic and cervical regions, affecting one or more vertebrae |
| skin - red moles on the body | |
| brain - vascular angiomas in the brain substance | |
| liver - single or multiple vascular neoplasms located in different parts of the organ | |
| kidneys - angiomas are formed from the veins and arteries that supply the organ | |
The most common causes of angiomas on the body are:
- hormonal changes in women (during pregnancy, taking oral contraceptives);
- skin injuries;
- genetic characteristics of the organism;
- diseases of the gastrointestinal tract, liver and pancreas;
- long exposure to sunlight and frequent visits to the solarium.
How long should you not sunbathe after mole removal?
Within 14 days after laser removal of a mole, the epidermis forms under the scab. After the crust has fallen off, thin newly formed skin is visible at the removal site. The epidermis (surface layer) has not yet had time to accumulate melanin in the cells, a substance that protects our body from ultraviolet radiation. This means that this place becomes vulnerable and it is in this zone that processes of improper cell division can begin. Therefore, after laser removal of not only moles, but also other neoplasms or blood vessels on the skin, direct exposure to sunlight on this area should be avoided for at least 2 months. Or, while tanning, cover the areas with a fabric that reliably protects the area from the sun (cotton shirt and trousers).
What does the appearance of red moles on the body mean?
If red moles appear on the body, this may be a simple cosmetic defect, or it may indicate pathological processes occurring in the body. In some cases, the occurrence of angiomas indicates poor nutrition, prolonged exposure to the sun, and a sludge buildup in the body.
Red dots like moles may indicate increased estrogen levels in the body, liver dysfunction and increased insulin in the blood. In addition, in some cases, angiomas appear as a response of the body to a lack of iodine, magnesium, chromium, vitamins C and K.
5. How many days does it take for a wound to heal after a mole is removed?
After removal, a dry crust remains on the skin. This is coagulated tissue. Underneath, healing and restoration of the skin begins to take place. After 7-10 days, this crust falls off on its own. Under no circumstances should you tear it off prematurely. The primary formed scar after the scab has fallen off is still different from the surrounding tissue. Regeneration processes continue in it and complete restoration of the structure ends by the 20th day. The area may still differ in color from the surrounding tissue, since the pigment accumulated in the cells is not equally distributed. But after a month it will be impossible to distinguish the place where the removal took place.
What to do if red moles appear on the body?
If red moles appear on the body in large numbers, single angiomas increase in size, or trauma to the red mole occurs, you should consult a dermatologist. Diagnosis of angiomas that are located on the surface of the skin is usually done by visual examination and palpation.
If there is a suspicion of the presence of red moles in the internal organs, additional research will be required to detect them. Skeletal angiomas are determined using x-rays of the spine, ribs, pelvis, bones and skull. Angiography (contrast X-ray examination of blood vessels) allows identifying red moles in the lungs, kidneys, brain and other internal organs. The structure of the angioma and the features of its location are determined by ultrasound examination.
After the diagnosis, the dermatologist will determine whether it is necessary to treat the red mole. So, the absolute indication for removing red moles is their rapid growth.
In addition, indications for treatment of angiomas are:
- localization in the neck and head;
- disruption of the functioning of the internal organ in which the angioma is located;
- extensive tissue damage around the red mole.
Treatment of red moles involves their removal, which can be done in various ways. Treatment methods for angiomas include:
- laser therapy;
- radio wave method;
- cryotherapy (removal of angiomas using liquid nitrogen);
- diathermoelectrocoagulation (cauterization with electric current);
- hormone therapy;
- ligation of the arteries that feed the angioma;
- surgery.
Effective therapy for red moles can only be prescribed by a dermatologist. Treatment of angioma with folk remedies is not recommended.
Diagnosis of moles during pregnancy
What to do if you notice the appearance of new age spots on the skin or an old mole has enlarged during pregnancy?
It is necessary to make an appointment for an in-person consultation with a dermatologist.
The doctor will conduct a visual examination of the pigment formation, assess its condition and appearance.
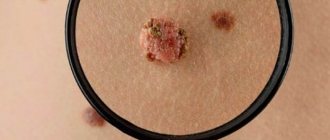
Dermoscopy is mandatory to determine the possible pathogenicity of the nevus.
Dermatoscopy is a non-invasive method for the differential diagnosis of pigmented skin lesions and early diagnosis of malignant melanoma.
This technique is also known as dermoscopy, reflected light microscopy, and epiluminescence microscopy.
Dermatoscopy is an integral part of the dermatological examination of the skin.
Today, the dermatoscope is considered the “dermatologist’s stethoscope.”
In addition to the diagnosis of pigmented and non-pigmented skin tumors, the method will be able to establish the diagnosis of infectious, parasitic and inflammatory lesions of the dermis.
In the field of dermato-oncology, dermatoscopy contributes to preoperative planning for the removal of pigmented skin lesions.
Helps you choose the best treatment option and subsequent care.
The main task of a dermatological examination is to find out the following points:
- whether the lesion is melanocytic or non-melanocytic;
- whether the formation is benign, suspicious or malignant.
In modern dermatology, digital dermatoscopy is more often used.
Where diagnostics displays the results of the procedure on a computer monitor.
This allows you to create reports with patient data and images of his pigmented lesions.
This makes it easier to make a diagnosis and makes it possible to consult with other specialists.
Another advantage of this method is that the images can be printed and given to the patient.
Alternatively, the digital images can be transferred to a CD and sent to the appropriate physician.
Are red moles dangerous?
Unlike melanoma (a malignant tumor), angioma is a benign formation. Single red moles on the body that do not increase in size and do not cause discomfort do not require treatment and are not dangerous.
But in some cases, red moles can lead to complications. Internal angiomas, depending on their location, can cause shortness of breath, difficulty breathing, epilepsy, impaired vision and hearing. In addition, angiomas can lead to complications if:
- red mole growing;
- there is a possibility of injury;
- many red moles appeared on the body;
- there is a risk of the mole transforming into a malignant formation.
Symptoms of malignancy
In order not to miss signs of a change in a mole, you need to constantly monitor its condition. You should periodically undergo preventive examinations with a dermatologist or independently examine yourself using a mirror.
Symptoms indicating possible malignancy include:
- change in contours: they become jagged, irregular, blurry;
- a sharp change in volume and shape: a significant increase in size over several months;
- the appearance of new shades: probably an intensification of color (becomes sharply black) or lightening, mottling;
- loss of symmetry of the mole;
- the appearance of a light or red border around the formation;
- hair loss in the area;
- the surface suddenly began to become wet, erosions, pus or bleeding appeared;
- the formation has become dense (rocky);
- the element began to become covered with horny scales.
Preventing the appearance of red moles
It is impossible to prevent the occurrence of congenital angiomas. A congenital red mole in a child is most often a short-term formation and disappears by the age of 5-7 years. Therefore, if the child does not complain of pain or itching in the area of the angioma, there is no need to worry.
In order to avoid the occurrence of angiomas after birth, it is necessary to follow these recommendations:
- avoid prolonged exposure to direct sunlight and frequent visits to the solarium;
- follow a sleep and nutrition schedule;
- lead a healthy lifestyle.
If you have a red mole, it is important to monitor its development and contact a dermatologist at the first signs of injury or change in size. With timely consultation with a doctor, it is possible to prevent complications of angiomas and, if necessary, begin therapy on time.
7
2
8
Article rating:
4 out of 5 based on 50 ratings
Author: Christopher Vasily Alekseevich
Dermatologist, pediatric dermatologist. Highest category. Work experience 24 years.
Is this dangerous for the woman and the unborn child?
If multiple moles and papillomas appear during pregnancy, they most likely do not pose a danger to the baby and mother.
Convex nevi usually appear in pregnant women in the abdominal area, under the mammary glands in the form of small formations on a stalk.
To confirm their benign growth, you need to seek help from a dermatologist.
He will evaluate the quality characteristics of the growth and will be able to give objective advice on care, recommend the method and time of its removal.
In case of malignant growth of a mole, there is a danger for the baby and mother. Indicates the development of melanoma. This cancer is characterized by its aggressive growth and early metastasis. It is important to regularly monitor the condition of new and old nevi.
If we are talking about infection with the human papillomavirus, then the strains that cause the appearance of plantar or vulgar types of warts, the typical location of which are the heels, soles, arms (hands) and other parts of the body, do not pose a danger to the child. If we are talking about genital warts as the most typical manifestation of urogenital papillomavirus (HPV), there is a danger to the baby in the form of papillomatosis of the upper respiratory tract.
For the mother, genital warts can threaten further erosion of the cervix and the development of cancer.
Papillomas that appear as a result of friction of the skin on clothing will go away on their own after childbirth. Such formations do not pose any danger.
Other skin diseases in pregnant women
Less common skin conditions during pregnancy are pemphigoid rash and intrahepatic cholestasis.
- Gestational pemphigoid rash
is an autoimmune disease that appears in the second or third trimester or after childbirth. Symptoms of this condition include blisters on the abdomen or other parts of the body. Increases the risk of premature birth or having a low birth weight baby. - Intrahepatic cholestasis of pregnancy
is a liver condition that appears in the third trimester. It is characterized by severe itching on the palms of the hands, soles of the feet or torso, and occurs without a rash.
If unusual sensations on the skin, itching or rashes appear, you should consult a doctor to find out the cause of the phenomenon and begin treatment on time.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Vein changes
Varicose veins often develop during pregnancy.
Spider veins are small red vessels that most often appear on the face, neck and arms. These skin changes occur due to changing hormones and increased stress on the legs, vagina and rectum. They go away after childbirth.
To minimize the risk of developing pathology and alleviate symptoms, you need to take the following precautions:
- do not sit or stand for a long time, combine feasible physical activity with rest;
- spread your legs when forced to sit for a long time;
- Perform seated leg raises whenever possible;
- consult with your doctor to select a set of physical exercises to prevent blood stagnation in the vessels;
- monitor digestion, avoiding constipation.
Is it safe to remove moles?
Today you can often see offers to remove moles using the laser method in a cosmetology office. For safety reasons, this is absolutely not worth doing. To carry out high-quality nevus removal, you should contact specialized medical institutions, where the procedure is performed by experienced medical workers. It is possible to immediately send the material for histological examination. Beauty salons do not provide this service. If a mole is suspected of being oncological, it is not recommended to use the laser method, which does not allow taking a tissue sample.
If the technology is followed, the nevus removal procedure is absolutely safe. The laser acts locally only on tumors, without heating neighboring organs and tissues.
What can cause a mole to start growing?
There are several factors that can cause nevus cells to divide, i.e. mole cells.
The first factor is exposure to ultraviolet radiation
.
The fact is that the brown pigment melanin, which is produced by nevus cells, is designed to protect us from excessive exposure to ultraviolet radiation. The mechanism of this action is quite complex, but we need to emphasize that the more melanin in our skin, the less damaging the sun is. Thus, nevus cells begin to divide to produce more brown pigment and better protect us from ultraviolet radiation. Outwardly, this is manifested by the appearance of new moles and the growth of those that already exist.
The second known factor is pregnancy
.
During this difficult period in a woman’s life, the hormonal levels in the body change - a lot needs to be rebuilt and prepared for the birth of a child. We will not go into details about what hormones the body produces and in what quantities during pregnancy. Let us only note that they also influence the cells of the mole and very often cause them to divide and the mole to grow.
Third, fourth, fifth, etc. factors have a significantly smaller evidence base and I will simply list them separated by commas - puberty, therapy with anti-inflammatory hormones or growth hormone.
Clinical studies have shown that in about 16% of nevi, microscopic changes in structure can be detected within a very short time - from 2.5 to 4.5 months. This fact suggests that there are other reasons for the growth of nevi (moles), but unfortunately, their role has not yet been studied.
Locations
An increase in the growth of moles is observed in people aged 0 to 20 years, and then from 45 years and older. The rest of the time they appear, but not as actively as in the first and last phases of life. Typically, red moles appear on the upper body, arms, legs and shoulders. Their favorite places are also the head, feet, and hands. They can be located throughout the body, and it is impossible to predict their subsequent locations. Their red color comes from the accumulation of small blood vessels at the base, which supply them with blood.
Laser mole removal how to care
After laser mole removal, the following is recommended:
Immediately after removal, slight swelling and redness may be observed around the wound, which goes away within 1-3 days.
Take care of the crust that has formed after removal so that it does not fall off or tear off prematurely. It protects the wound from infection. Wear clothing that protects this area and do not scratch it.
If symptoms such as redness of the skin around the crust, swelling, pain, sanguineous or purulent discharge appear, immediately contact the clinic where the mole was removed with a laser .
While the crust protects the wound, there is no need to treat it with anything additional. After the scab has separated, to accelerate epithelization, you can apply a cream with dexpanthenol, solcoseryl, etc.
Follow the restrictions: solarium and insolation for up to 2 months; do not go to the bathhouse, sauna, or bath for 14 days; Avoid alcohol intake for the first 3 days; During the period until the scab falls off, cosmetics are not applied to this area.
Laser mole removal takes a long time to heal.
The healing time depends on the size of the mole, location, and individual characteristics of the regenerative processes.
If they are small in size, up to 0.5 cm, moles heal in 10-14 days; if they are larger than 1 cm, regeneration takes up to 3-4 weeks.
In places with good blood supply and in open areas of the body, healing is faster, up to 14 days. In places that are subject to friction (belt, bra line, groin area), get wet (perineum, armpits), have thick skin and poor blood flow (sole, palm), healing takes up to 4 weeks.
Increase in the size of nevi
There is no need to worry if moles appear during pregnancy. After all, the process is normal and does not require any special measures. But you need to pay attention to the formations that undergo changes when carrying a child. A woman should be wary if:
- changes in shade;
- increase in size;
- the appearance of pain syndrome;
- detection of itching and burning;
- transformation of flat formations into hanging ones.
The nature of the changes should be determined by the doctor during the examination.
Any changes should prompt the woman to visit a doctor. It’s better not to panic in advance, because new properties are often caused by increased hormone levels.
Many women do not know who to contact with a problem when a mole has enlarged. First of all, it is necessary to notify the obstetrician-gynecologist who is observing the woman. You can also contact a dermatologist or oncologist yourself.
The doctor must examine the formation. Based on it, you can determine the type and nature of the mole.