Every person has moles, and if they don’t get in the way or are not in visible places, we simply don’t notice them. But it happens that a mole makes itself felt - it hurts, itches, or even falls off. In this case, a trip to a dermatologist is inevitable, because such formations are classified as oncogenic, i.e. capable of developing into cancer.
Dermatological diseases and peeling moles
A very large group of reasons for peeling skin over moles.
The most common:
- allergic processes;
- genetic – ichthyosis;
- psoriasis;
- pityriasis versicolor;
- seborrhea;
- contact dermatitis.
The list can be continued for a very long time.
It is important to remember one thing: if dermatological pathology manifests itself as peeling and affects areas of the skin with moles, then this is a reason to consult a dermatologist and undergo a course of treatment.
Problems usually arise among those who do not want to be examined by a specialist and try to cure themselves.
Allergies
are a very common cause in modern civilization.
Character traits:
- the skin turns red;
- small urticaria-type rashes or large, dense papules appear;
- the involved areas itch, itch unbearably;
- As the allergy resolves, fairly large areas of peeling may remain at the site of the rash, including moles.
The beginning of the process after contact with an allergen (which one is an individual matter) indicates in favor of an allergic component.
Ichthyosis
This genetic pathology is not that uncommon.
There are cases in dermatological practice when large areas of the dermis of children peel off along with the moles located on them.
External signs depend on the severity of the disease: from dry skin to deep cracks.
Psoriasis
Another common reason for peeling.
Moreover, such a process is a characteristic sign of this disease.
The scales peel off almost like flakes.
But since only the epithelium of the stratum corneum (which is continuously renewed) disappears, the moles located deeper (nevi) do not disappear anywhere.
True, they can hide under plaques and become invisible.
Pityriasis versicolor
This is a fungal disease, the sign of which is a limited area of peeling, as if consisting of several spots.
The shape is round, the edges are uneven, scalloped.
The formation is painless, but in some people it itches.
Naturally, the focus of pityriasis versicolor can occur above the mole.
If it is also small in size, then sometimes it seems as if a mole is peeling off.
Although this is not true.
Seborrhea
A common phenomenon is when sebum synthesis is too active.
Quite often such problems arise on the head.
Foci of different sizes are formed, covered with loose yellowish scales, which literally peel off in layers.
Seborrhea occurs in children and adults.
The affected surface shines and peels, which is why it becomes a frequent reason for contacting dermatologists.
Contact dermatitis
Most often, these will be local allergic reactions in response to contact with allergenic fabric, detergent residue, grass, and so on.
They differ in that itching, redness and peeling occur to a limited extent.
Only on the surface of the body that came into contact with the allergen.
First aid
When a mole falls off, it is necessary to prevent the development of complications even before seeking professional help. Manipulations depend on the type of mole damage.
- If a mole partially falls off.
To avoid infection of the wound, it is necessary to wipe it with hydrogen peroxide. This must be done immediately, especially if blood begins to ooze from it. After treating the wound, it is sealed with a plaster and the site of the injury is immediately shown to the doctor. - Complete falling away.
With this type of injury there may be some bleeding. First of all, it needs to be stopped. To do this, apply a sterile swab soaked in hydrogen peroxide to the damaged area. You need to keep it for at least half an hour, periodically changing it to a new one. Then a tampon soaked in an antiseptic is applied to the wound for 5 minutes. After all the manipulations, close the wound with a plaster and consult a doctor. It is necessary to get an appointment with a dermatologist in the next few hours, if possible. It is very good if the fallen mole or part of it is preserved. This will significantly improve the quality of diagnostic results and laboratory tests (for cancer cells). It is best to deliver the skin element to the laboratory in saline solution. If this is not available, a salt solution will do. It should not be highly concentrated, otherwise the results may be inaccurate. The nevus is placed in gauze soaked in liquid and submitted for testing in this form.
Problems with a mole
The greatest danger that nevi pose is the risk of degeneration of benign pigmented neoplasms into an aggressive tumor of melanocytes - melanoma.
This cancer accounts for only 4% of all skin tumors.
However, the particular aggressiveness and tendency to metastasize make melanoma a very dangerous process.
The high incidence of skin cancer is not associated with melanocytes, but descavamation is very characteristic of them.
When to see a doctor
If a mole, for no apparent reason, has dried out or changes in size or color have occurred, this is an alarming signal to immediately contact a doctor who will examine the formation and determine whether there is an indication for removal. Signs include:
- excessive peeling, dryness, roughness of the growth;
- if a benign formation does not meet the standards - an irregular shape, compaction has appeared, a change in the surface of the growth;
- if blood oozes from the mole, pus or ichor is secreted, there is an unpleasant odor;
- growth, the area around becomes denser;
- there is pain when touched;
- changes color to red, black or white;
- severe itching.
If a dangerous sign is present, removal is prescribed to help avoid the development of complications and prevent skin cancer.
Non-melanocytic processes during desquamation
Their source is the cells of any of the layers of the dermis or epidermis.
Let's look at the most common causes of cancer processes that are not directly related to moles.
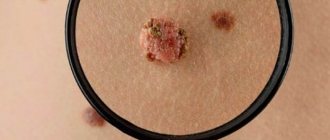
Seborrheic keratosis, seborrheic wart or keratoma.
It starts with a small spot covered with yellowish scales.
It grows gradually and after a few decades reaches 6 cm in diameter.
Because of its coloring and loose scales, seborrheic keratoma is sometimes mistaken for a mole that has begun to grow and peel off.
Is it time to sound the alarm?
Moles, or, in scientific terms, nevi, are present on the body of every person. It is believed that the bulk of them, up to 90%, appear by the age of 25. But they can also arise later - under the influence of various events. For example, a typical phenomenon is when they literally break out during pregnancy. Sometimes moles, on the contrary, disappear over time. They can be yellow, brown, black. This is all within normal limits and there is nothing to worry about.
But it happens that a mole begins to grow unevenly or changes color, its surface becomes “polished” or it begins to bleed - that is, changes occur in it. Another option is the appearance of a new mole of an unusual appearance. It is precisely such incomprehensible neoplasms that require close attention.
Papillomatosis as a cause of peeling
A very common process, often provoked by human papillomaviruses.
Outwardly it looks like a small outgrowth of skin, single or multiple.
People sometimes call this formation a pedunculated mole, although papillomas are not classified as pigmented formations.
Unfortunately, they can become malignant and transform into squamous cell skin cancer.
The most common malignant cause of peeling is basal cell carcinoma.
This is a relatively rare metastatic tumor.
It grows slowly and often appears on the scalp, face and other exposed parts of the body.
One form, nodular basal cell carcinoma, may contain patches of melanin, which makes it resemble a large, growing mole.
Areas of peeling are observed around the pigment spot, crusts are formed, and the color of the node becomes uneven.
For squamous cell carcinoma, desquamation is not as common.
This process often occurs with lesions at the site of previously benign tumors.
For example, where there was recently a hanging mole.
Separately, it is worth dwelling on hemangiomas.
These are vascular, benign tumors that in the early stages look like a reddish spot and can easily be confused with a mole.
Often found in children.
Typical location:
- on the lip;
- on the skin of the back;
- on the genitals (labia, vulva, foreskin of the penis).
Hemangiomas of the abdomen and extremities are less common.
Peeling is not typical for them.
It may indicate either a near resolution of the process (spontaneous recovery from hemangiomas is not uncommon) or a progression of the pathology.
Why do moles fall off?
First you need to find out whether it was a mole. Perhaps it was another formation: age spots, crusts due to injuries, in places of scratching, fungal infections, etc. can form on the skin. Since not every nevus is convex, a mole cannot fall off on its own, because the formation is part of the skin. Formations on the skin that tend to fall off are called keratomas. They are darker than nevi. The older the person, the greater the likelihood that the keratoma will fall off. But if it turns out that it is the mole that has fallen off, then you need to identify the reasons:
- Hormonal surges.
When hormonal imbalance occurs, a mole forms. When it normalizes, the mole dies. Such phenomena are not uncommon during age transitions, during pregnancy, or when taking hormonal medications. - Traumatic factors.
Excessive tanning in direct sunlight, cuts to the mole, or friction of clothing against the nevus can cause the mole to peel off. - Necrosis.
The formation will fall off if it does not receive the substances necessary for normal functioning. For example, long moles are at risk: they become twisted, blood flow is disrupted and the nevus dries out. - Tumor.
The mole causes discomfort, itches and develops into melanoma. Cellular growth occurs, the mole dries out and falls off. This is the most dangerous reason.
Melanocytic processes during desquamation of a mole
Let us remember that melanoma accounts for only 4% of malignant skin tumors.
However, even this possibility must be taken into account.
Almost all melanomas develop from nevi (moles).
When this happens, five visually detectable parameters of pigment formation change:
- Asymmetry appears.
- The edge is “blurred”.
- The color changes - it lightens or darkens, the nevus can become spotted.
- The diameter increases.
- Changes increase (the focus evolves) over a relatively short period of time, several weeks or days.
At the same time, the degenerating mole itches, hurts, is easily injured, and at times peels off.
However, desquamation is not typical for most melanomas.
Should I delete
Removal of a scaly spot is indicated when a transformative process into a malignant tumor is identified or a nevus is located in a place that spoils a person’s appearance. There are several effective methods that can be used to get rid of dangerous or unwanted stains:
- Laser removal. The impact of the laser helps the mole fall off. Among the advantages of the method are the absence of scars and pain during the procedure.
- Radio wave removal. Using a radio knife, the doctor excises the formation and cauterizes the vessels to prevent bleeding.
- Cryodestruction method. Liquid nitrogen freezes cells and blood vessels, causing the nevus to disappear. Used for small formations.
- Electrocoagulation. Excision occurs using alternating or high-frequency current, which cauterizes vessels and tissues, as a result the growth dies and falls off.
- Removal using a scalpel. The method is used for large formations. The disadvantage of surgical intervention is the presence of scars and scars after the operation. It is not recommended to remove nevi located in a visible place with a scalpel. Among the advantages is the low cost of the procedure.
The need for removal and the choice of method are determined by the doctor based on the examination.
Diagnosis of peeling moles
You should always contact a dermatologist when:
- the mole grows rapidly, increasing in size daily or weekly;
- the structure of the nevus changes - it thickens, becomes hard, or vice versa, disintegrates, falls apart;
- peeling above it covers new areas or, on the contrary, becomes concentrated, limited and transformed into crusts;
- a mole was injured with bleeding (even if the bleeding stopped quickly);
- the spot hurts and itches a lot;
- the nevus falls off on its own, as if peeling off;
- and in any other cases when a mole behaves suspiciously or a patch of peeling appears on the body.
Every year or every 6 months, all people who have many moles (more than 50) need to see a dermatologist.
And if they also begin to peel off, then you need to make an appointment immediately.
Diagnosis is quite simple: dermatoscopy.
An experienced dermatologist examines the suspicious area of skin under multiple magnification and good lighting.
And, if he finds signs of infiltrating growth, he suggests removing such a focus.
However, there are indications for removal for ordinary, benign nevi.
When they are potentially dangerous by degenerating into a cancerous tumor.
The appearance of a crust on a mole
The growth on the nevus may be white or brown. This crust appears when there is an injury or burn. If a mole begins to crumble, the result may be skin cancer. You cannot peel off the crust yourself, as this can lead to infection of the skin. To exclude nevus transformation, it is necessary to undergo dermatoscopy by a dermatologist or oncologist. This is the diagnosis of skin lesions using special optical equipment - the procedure is absolutely painless, does not require preparation and takes no more than 10 minutes.
If the doctor finds suspicious symptoms, a biopsy will be required. In this case, a small area of skin is taken for analysis in the laboratory.
Mole removal methods
Seborrheic keratosis and other benign formations that are assessed as dangerous are usually excised. Removal serves as a prevention of degeneration or as a method of combating the early stages of dysplasia. The doctor chooses the method in accordance with the nature of the growth.
Popular and effective methods of destruction:
- laser removal. The instrument is a high power beam of light. It destroys cells, evaporating them from the surface of the skin. The advantage is maintaining the integrity of neighboring healthy tissues. Laser radiation parameters are selected individually for each patient. A crust remains at the treatment site, which comes off on its own after 7-14 days. During the procedure there is no pain and no bleeding. The laser prevents the formation of new elements. Disadvantage – lack of material for histology due to its complete destruction;
- cryodestruction. It is used in cases where the body of the growth is located in the upper layers of the epidermis. The dermatologist treats it with liquid nitrogen, which is applied to the surface and removed after 3 minutes. During the process, pain and discomfort are felt. In the first days, decomposition of the pigment is noted, the formation of a crust, which will come off after a few weeks;
- radio wave therapy. The rough element is cut off from the surface using a non-traumatic method. The main advantage is the cauterization of tissue during the incision, which prevents bleeding. Thanks to coagulation, the wound heals quickly. The technique cannot be used by patients in a feverish state, with herpes and a pacemaker;
- diathermoelectrocoagulation. The skin lesion is cut off with a red-hot metal loop. Then the area of the skin affected is cauterized with a coagulator. As a result, there is no blood and the risk of infection is reduced. A crust remains at the treatment site and comes off naturally. A small mark may remain;
- surgical destruction. The most reliable way to remove a large or hanging mole. It is prescribed to the patient when other methods are powerless or a change has begun at the cellular level (the onset of melanoma). The doctor works with a scalpel, cutting off the problematic growth and the tissue underneath it. After healing, a scar remains on the surface, increasing the chance of stopping the cancer.
The speed of healing depends on many factors: location (head or torso), chosen technique, size of the mole. Do not touch with your hands or remove the crust that has formed to protect against infection.
Possibility of unforeseen consequences
Laser correction of moles is one of the safest ways to get rid of nevus, avoiding complications and unforeseen consequences. A beam of directed light radiation literally evaporates the pigmented cells of moles, which is visually manifested by the complete removal of the epidermal formation in just a few minutes. Minimization of negative consequences occurs due to the following objective factors.
- The laser beam acts in a strictly targeted and selective manner, without injuring healthy skin structures, which allows the technique to be used even to remove the smallest nevi in the eyelid area and mucous membranes;
- There is virtually no risk of infection, since the laser exhibits a powerful antibacterial and antimicrobial effect, protecting the wound surface from infection;
- Laser destruction is not accompanied by bleeding or hemorrhage, since during the manipulation process all blood capillaries supplying the body of the mole undergo thermal coagulation;
- The laser activates regenerative processes in the skin, which significantly accelerates wound healing;
- The technique is low-traumatic, which avoids the formation of connective tissue and all the negative consequences associated with this factor.
Despite the safety of the method, it should be borne in mind that before the procedure it is necessary to carefully study the list of contraindications, since the consequences and complications of laser correction most often result from neglect of this list, which includes the following conditions:
- Pregnancy;
- Acute infectious process;
- Oncology of any localization;
- Inflammation in the intended area of laser exposure;
- Period of menstruation in women;
- Immunodeficiency;
- Exacerbation of chronic pathologies;
- Hyperthermia.
Risks of the appearance and development of melanoma
One of the main factors in the development of melanoma is an increase in the duration of exposure to ultraviolet radiation in people whose skin is not genetically adapted to it. As a rule, this type includes people with white skin that is not prone to tanning. Representatives of dark and dark skin, on the contrary, suffer from melanoma much less frequently (10-20 times less often). In addition to genetic predisposition, there are other risk factors:
- Physical – ionizing radiation, trauma, excessive insolation, fluorescent lighting;
- chemical – contact with nitric acid, benzene, coal and pharmaceuticals;
- biological - with alcohol and certain medications (for example, estrogen-containing hormonal drugs).
External biological characteristics of the body that increase the risk of developing melanoma also include: the first two skin phototypes (in which the skin is light and prone to sunburn), the presence of freckles and lentigo, a family history, and immune disorders. Based on the above factors, 3 risk groups are distinguished, which are more likely to undergo screening examinations according to indications.
How to distinguish a seborrheic mole from dangerous symptoms
A rough mole can frighten the wearer with its unusual appearance. Outwardly, it may resemble melanoma; only a doctor and diagnostic measures can accurately determine the type of tumor.
The main differences between seborrheic keratosis and an oncological tumor:
| Factor | Keratosis | Melanoma |
| Risk group | People over 30 years of age whose skin is susceptible to aging. | Can be diagnosed at any age. The patient may be a small child, an able-bodied adult, or an elderly person. |
| Form | A round or oval growth with clear boundaries. It has the ability to grow and thicken up to 1-2 cm. | Formation over 6 mm. |
| View | Flaky mole. Flat or slightly convex appearance. It may look waxy, as if painted on the body. | A spot or raised element that is in the stage of active growth. |
| Symmetry | Complied with. | Violated. |
| Color | Uniform or interspersed with white and black. | It changes and takes on several shades. |
| Borders | Smooth. | Vague with jagged edges. |
The dry growth is dense to the touch, like a dangerous nevus, but it does not hurt when touched, at rest. A painful syndrome can develop when irritated or damaged, then the skin around it itches, and secondary infection can occur.
If a person is accustomed to unusual spots on the body, he may miss cancer. Patients with keratosis are recommended to regularly visit a dermatologist and undergo diagnostics.
Melanoma is on the rise. Its increase occurs quickly: by 1-2 mm per month or more.
Medical classification of melanomas
To determine the stage of melanoma, the Unified Staging System is quite informative, which distinguishes 4 stages - according to the thickness of the tumor and the depth of its invasion according to Clark:
- 1 – tumor thickness up to 1.5 mm with invasion level 2-3;
- 2 – tumor thickness up to 4 mm and invasion level 4-5;
- 3 – regional presence of metastases about 3 centimeters in diameter;
- 4 – distant metastases.
Melanoma can occur in both cutaneous and extracutaneous forms (10-20%) - with localization on the mucous membrane of the esophagus, rectum, genitals, eye mucosa, etc. The proportion of cutaneous forms is incomparably greater - 70-80%, but poses no less a threat for a large number of people around the world.
Preventing and reducing the risk of melanomas
The postulates in the prevention of skin melanoma are: screening, limiting damaging factors, removing altered pigment formations.
Screening includes non-invasive diagnostic methods - dermatoscopy or epiluminescence microscopy annually, and for risk groups at least 2 times a year. Eluminescent microscopy is a non-invasive method for studying skin formations in a special immersion environment that can save a digital image, enter it into a database and track changes by comparing it with existing and subsequent images.
Primary prevention is to avoid the damaging effects of ultraviolet radiation, chemicals and other external factors. Secondary prevention is the removal of all moles suspicious for malignancy.
Tips that can prevent the development of melanoma are quite simple and effective. Will help reduce the risk of mole degeneration:
- wearing dark, thick clothing;
- eating vitamin D;
- removal of altered or injured moles.
The widespread use of screening and preventive measures will have a beneficial effect on the timely diagnosis and treatment of this dangerous disease.
Briefly about the main thing:
Itching alone is EXTREMELY rarely a sign that a mole has turned into melanoma. Most often it is caused by other reasons. In addition, the malignancy of the mole should be accompanied by symptoms other than the feeling that the mole itches
.
If you still have questions, the following will help you:
- In-person appointment with an oncologist
(St. Petersburg) - Mole removal
with histology (St. Petersburg) - My online consultation (from anywhere in the world)