Every person has moles, and if they don’t get in the way or are not in visible places, we simply don’t notice them. But it happens that a mole makes itself felt - it hurts, itches, or even falls off. In this case, a trip to a dermatologist is inevitable, because such formations are classified as oncogenic, i.e. capable of developing into cancer.
What is a mole
The content of the article
A mole is a formation on the skin colored by the pigment melanin. The color of the mole can vary, ranging from light to dark brown. Other names for moles are nevus, birthmark. A person can have 30 birthmarks or more. They can be different in shape and size.
Nevi begin to appear from the age of two and continue to gradually form throughout life. Their appearance depends not only on heredity, but also on exposure to ultraviolet radiation and hormonal imbalances in the body for various reasons.
A formation that has not undergone certain changes is considered benign, and in the absence of various types of discomfort does not require consultation with a dermatologist. However, most often moles are harmless and do not pose any threat to human life. However, if the nevus begins to manifest itself, this may be the beginning of a dangerous disease called melanoma.
According to statistics, problematic moles are more common in men than in women. And on the hands the percentage of malignant formations is several times lower than on other areas of the skin.
Papillomatosis as a cause of peeling
A very common process, often provoked by human papillomaviruses.
Outwardly it looks like a small outgrowth of skin, single or multiple.
People sometimes call this formation a pedunculated mole, although papillomas are not classified as pigmented formations.
Unfortunately, they can become malignant and transform into squamous cell skin cancer.
The most common malignant cause of peeling is basal cell carcinoma.
This is a relatively rare metastatic tumor.
It grows slowly and often appears on the scalp, face and other exposed parts of the body.
One form, nodular basal cell carcinoma, may contain patches of melanin, which makes it resemble a large, growing mole.
Areas of peeling are observed around the pigment spot, crusts are formed, and the color of the node becomes uneven.
For squamous cell carcinoma, desquamation is not as common.
This process often occurs with lesions at the site of previously benign tumors.
For example, where there was recently a hanging mole.
Separately, it is worth dwelling on hemangiomas.
These are vascular, benign tumors that in the early stages look like a reddish spot and can easily be confused with a mole.
Often found in children.
Typical location:
- on the lip;
- on the skin of the back;
- on the genitals (labia, vulva, foreskin of the penis).
Hemangiomas of the abdomen and extremities are less common.
Peeling is not typical for them.
It may indicate either a near resolution of the process (spontaneous recovery from hemangiomas is not uncommon) or a progression of the pathology.
What is melanoma: dangerous signs of degeneration of moles
Melanoma is a skin tumor that is classified as malignant, in other words, it is skin cancer. A tumor can appear anywhere, but a mole is especially often the source of cancer.
You should urgently see a dermatologist if:
- The mole has changed. For example, it turned black or began to grow;
- It falls off piece by piece and is crushed;
- It is found in places where underwear touches, a belt, or rubs with clothing, and therefore itching and redness of the area around the mole appears.
If a mole falls off on your body, do not ignore this symptom - see a dermatologist as soon as possible.
Non-melanocytic processes during desquamation
Their source is the cells of any of the layers of the dermis or epidermis.
Let's look at the most common causes of cancer processes that are not directly related to moles.
Seborrheic keratosis, seborrheic wart or keratoma.
It starts with a small spot covered with yellowish scales.
It grows gradually and after a few decades reaches 6 cm in diameter.
Because of its coloring and loose scales, seborrheic keratoma is sometimes mistaken for a mole that has begun to grow and peel off.
Why do moles fall off?
First you need to find out whether it was a mole. Perhaps it was another formation: age spots, crusts due to injuries, in places of scratching, fungal infections, etc. can form on the skin. Since not every nevus is convex, a mole cannot fall off on its own, because the formation is part of the skin. Formations on the skin that tend to fall off are called keratomas. They are darker than nevi. The older the person, the greater the likelihood that the keratoma will fall off. But if it turns out that it is the mole that has fallen off, then you need to identify the reasons:
- Hormonal surges.
When hormonal imbalance occurs, a mole forms. When it normalizes, the mole dies. Such phenomena are not uncommon during age transitions, during pregnancy, or when taking hormonal medications. - Traumatic factors.
Excessive tanning in direct sunlight, cuts to the mole, or friction of clothing against the nevus can cause the mole to peel off. - Necrosis.
The formation will fall off if it does not receive the substances necessary for normal functioning. For example, long moles are at risk: they become twisted, blood flow is disrupted and the nevus dries out. - Tumor.
The mole causes discomfort, itches and develops into melanoma. Cellular growth occurs, the mole dries out and falls off. This is the most dangerous reason.
Dermatological diseases and peeling moles
A very large group of reasons for peeling skin over moles.
The most common:
- allergic processes;
- genetic – ichthyosis;
- psoriasis;
- pityriasis versicolor;
- seborrhea;
- contact dermatitis.
The list can be continued for a very long time.
It is important to remember one thing: if dermatological pathology manifests itself as peeling and affects areas of the skin with moles, then this is a reason to consult a dermatologist and undergo a course of treatment.
Problems usually arise among those who do not want to be examined by a specialist and try to cure themselves.
Allergies
are a very common cause in modern civilization.
Character traits:
- the skin turns red;
- small urticaria-type rashes or large, dense papules appear;
- the involved areas itch, itch unbearably;
- As the allergy resolves, fairly large areas of peeling may remain at the site of the rash, including moles.
The beginning of the process after contact with an allergen (which one is an individual matter) indicates in favor of an allergic component.
Ichthyosis
This genetic pathology is not that uncommon.
There are cases in dermatological practice when large areas of the dermis of children peel off along with the moles located on them.
External signs depend on the severity of the disease: from dry skin to deep cracks.
Psoriasis
Another common reason for peeling.
Moreover, such a process is a characteristic sign of this disease.
The scales peel off almost like flakes.
But since only the epithelium of the stratum corneum (which is continuously renewed) disappears, the moles located deeper (nevi) do not disappear anywhere.
True, they can hide under plaques and become invisible.
Pityriasis versicolor
This is a fungal disease, the sign of which is a limited area of peeling, as if consisting of several spots.
The shape is round, the edges are uneven, scalloped.
The formation is painless, but in some people it itches.
Naturally, the focus of pityriasis versicolor can occur above the mole.
If it is also small in size, then sometimes it seems as if a mole is peeling off.
Although this is not true.
Seborrhea
A common phenomenon is when sebum synthesis is too active.
Quite often such problems arise on the head.
Foci of different sizes are formed, covered with loose yellowish scales, which literally peel off in layers.
Seborrhea occurs in children and adults.
The affected surface shines and peels, which is why it becomes a frequent reason for contacting dermatologists.
Contact dermatitis
Most often, these will be local allergic reactions in response to contact with allergenic fabric, detergent residue, grass, and so on.
They differ in that itching, redness and peeling occur to a limited extent.
Only on the surface of the body that came into contact with the allergen.
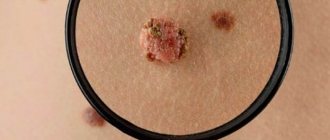
The appearance of a crust on a mole
The growth on the nevus may be white or brown. This crust appears when there is an injury or burn. If a mole begins to crumble, the result may be skin cancer. You cannot peel off the crust yourself, as this can lead to infection of the skin. To exclude nevus transformation, it is necessary to undergo dermatoscopy by a dermatologist or oncologist. This is the diagnosis of skin lesions using special optical equipment - the procedure is absolutely painless, does not require preparation and takes no more than 10 minutes.
If the doctor finds suspicious symptoms, a biopsy will be required. In this case, a small area of skin is taken for analysis in the laboratory.
Melanocytic processes during desquamation of a mole
Let us remember that melanoma accounts for only 4% of malignant skin tumors.
However, even this possibility must be taken into account.
Almost all melanomas develop from nevi (moles).
When this happens, five visually detectable parameters of pigment formation change:
- Asymmetry appears.
- The edge is “blurred”.
- The color changes - it lightens or darkens, the nevus can become spotted.
- The diameter increases.
- Changes increase (the focus evolves) over a relatively short period of time, several weeks or days.
At the same time, the degenerating mole itches, hurts, is easily injured, and at times peels off.
However, desquamation is not typical for most melanomas.
First aid
When a mole falls off, it is necessary to prevent the development of complications even before seeking professional help. Manipulations depend on the type of mole damage.
- If a mole partially falls off.
To avoid infection of the wound, it is necessary to wipe it with hydrogen peroxide. This must be done immediately, especially if blood begins to ooze from it. After treating the wound, it is sealed with a plaster and the site of the injury is immediately shown to the doctor. - Complete falling away.
With this type of injury there may be some bleeding. First of all, it needs to be stopped. To do this, apply a sterile swab soaked in hydrogen peroxide to the damaged area. You need to keep it for at least half an hour, periodically changing it to a new one. Then a tampon soaked in an antiseptic is applied to the wound for 5 minutes. After all the manipulations, close the wound with a plaster and consult a doctor. It is necessary to get an appointment with a dermatologist in the next few hours, if possible. It is very good if the fallen mole or part of it is preserved. This will significantly improve the quality of diagnostic results and laboratory tests (for cancer cells). It is best to deliver the skin element to the laboratory in saline solution. If this is not available, a salt solution will do. It should not be highly concentrated, otherwise the results may be inaccurate. The nevus is placed in gauze soaked in liquid and submitted for testing in this form.
Diagnosis of peeling moles
You should always contact a dermatologist when:
- the mole grows rapidly, increasing in size daily or weekly;
- the structure of the nevus changes - it thickens, becomes hard, or vice versa, disintegrates, falls apart;
- peeling above it covers new areas or, on the contrary, becomes concentrated, limited and transformed into crusts;
- a mole was injured with bleeding (even if the bleeding stopped quickly);
- the spot hurts and itches a lot;
- the nevus falls off on its own, as if peeling off;
- and in any other cases when a mole behaves suspiciously or a patch of peeling appears on the body.
Every year or every 6 months, all people who have many moles (more than 50) need to see a dermatologist.
And if they also begin to peel off, then you need to make an appointment immediately.
Diagnosis is quite simple: dermatoscopy.
An experienced dermatologist examines the suspicious area of skin under multiple magnification and good lighting.
And, if he finds signs of infiltrating growth, he suggests removing such a focus.
However, there are indications for removal for ordinary, benign nevi.
When they are potentially dangerous by degenerating into a cancerous tumor.
How to detect melanoma at an early stage
Since melanoma is dangerous, a person needs to take strange growths very seriously, be it a mole, wart, or pimple. Under no circumstances should you delay visiting a doctor, since in just a couple of months radical treatment may turn out to be useless, and the specialist will only offer maintenance therapy.
Diagnosis of melanoma includes:
- Dermatoscopy. Suspicious moles and areas of skin are examined through a dermatoscope - a special microscope that allows you to study the skin in incident light (electroluminescence effect).
- Smear-imprint. Used if there are cracks or ulcers on the surface of the formation. The smear looks for tumor cells.
- Biopsy. Allows you to accurately determine the type of tumor: malignant or benign. To do this, the tumor area is examined under a microscope.
- Computer, magnetic resonance or positron emission tomography. Any of the tests to check other organs for the presence of metastases.
- Sentinel lymph node biopsy. Helps clarify the diagnosis and determine whether there are metastases. Typically, tumor cells are retained in the nearest lymph node, which is why it is checked for the presence of metastases.
Special biopsy method
Carrying out a biopsy is a controversial issue in the case of melanoma, since injuring the tumor can cause its rapid growth. In some cases, an excisional biopsy is resorted to. The surgeon excises the tumor, capturing 2-10 mm of healthy skin around it. While the patient is being sutured, the lesion is urgently sent for histology, often right in the operating room. If the diagnosis is confirmed, the surgeon immediately begins a repeat operation. The task is to remove all the tumor that could grow deep into the skin. Here everything depends on the results of histology, which determines the stage of the disease.
Why does melanoma occur?
The exact causes of melanoma are still unknown. The main risk factor is prolonged exposure to ultraviolet radiation. To reduce your risk of skin cancer, you need to reduce your time in the sun. Although completely avoiding this does not provide 100% protection against melanoma. Dermatologists advise limiting your stay during dangerous hours - from 11 to 16 hours of the day, and also the time - no more than 30 minutes (if longer, you need to apply protective products with SPF50+).
Visiting a solarium also increases the risk of developing melanoma. According to research, in young people under 35 years of age, artificial tanning can increase the likelihood of skin cancer by 75%. In terms of the risk of developing melanoma, tanning beds are on the same level as smoking as a cause of lung cancer.
Moles as a reason
In 50% of cases, cancer forms from existing moles. The more there are, the higher the risk of encountering melanoma. The process can be triggered by injury, frequent exposure to ultraviolet radiation, or changes in hormonal balance. For this reason, it is necessary to periodically examine moles for any changes. Suspicion should be raised by:
- active growth for a couple of weeks or months;
- changes in color, shape or borders;
- the appearance of small moles and spots nearby;
- the appearance of blood from a mole for no reason;
- crusts, ulcerations;
- pain and itching in the mole area.
Risk factors (who is at risk)
About 10% of people with melanoma have a family history of melanoma. According to research, if two or more close relatives have experienced skin cancer, the likelihood of developing it increases significantly. People at risk include:
- with pale skin that is difficult to tan;
- a lot of freckles;
- red or blond hair;
- blue eyes;
- burn scars;
- diseases of the immune system (HIV);
- exposed to chemicals.
How does laser mole removal work?
The procedure for removing moles is standard and includes several stages:
- Examination of the skin by a dermatologist to exclude the presence of signs of melanoma. There is a classification of 5 criteria for which the doctor must examine and check the formation. Shape, size, color, surrounding tissue, density. Sometimes dermatoscopy (examination of an element under multiple magnification) can be used for diagnosis. Having completely convinced that the formation is benign, the specialist begins the removal procedure itself.
- Consultation before the procedure. The dermatologist talks about how the procedure will take place and the symptoms that will accompany it. Possible complications and limitations that will occur after the manipulation.
- Signing the patient's informed consent for the administration of anesthetic and laser vaporization.
- Next, he proceeds directly to removing the mole. The area is treated with a skin antiseptic. An anesthetic injection is given. After complete freezing, the mole is removed within healthy tissue using a CO laser. Repeated treatment with a disinfecting solution is carried out.
- Recommendations for care.
Treatment: removal or observation?
Benign neoplasms of the skin do not require removal, but surgery can be performed for aesthetic reasons, as well as in situations where the nevus is located in an open area of the body, is exposed to ultraviolet radiation, or is injured by parts of clothing or jewelry.
Removal of benign black moles that are not melanoma-dangerous is carried out in the following ways:
- Surgical removal;
- cryodestruction;
- electrocoagulation;
- radio wave removal;
- laser removal.
Melanoma-dangerous nevi can only be removed surgically. The operation is performed in the presence of an oncologist and involves healthy skin. The removed tissues are necessarily sent for histological examination. Melanoma-dangerous nevi can also be removed in aesthetic medicine clinics if the medical institution has a dermatologist oncologist on staff. The operation is performed in a classical way; cryodestruction and other modern technologies are not used.
If malignant degeneration of the neoplasm is diagnosed, complex antitumor therapy is indicated, which includes surgical removal with wide coverage of adjacent tissues, radiation and chemotherapy.