Discomfort, bruising and swelling after contouring
Edema is the excessive accumulation of fluid in extracellular tissues. It is a standard reaction of soft tissues to damage and accompanies most medical interventions, including contouring. Normally, swelling after contouring should go away within a few days (up to 2 weeks), but it can persist longer. The percentage of development of undesirable consequences as a result of correction of cosmetic defects with fillers is small, but not only the doctor, but also the patient should be aware of them.
To one degree or another, swelling after contouring of the cheekbones, lips and other areas almost always develops; the question is how severe it is. Tissues react with swelling to microtraumas; the ability of the filler to accumulate and retain moisture also plays a role. The normal period for swelling to resolve is several days, up to two weeks; if the swelling lasts longer, most likely:
- there is an individual reaction of the body, in particular, a previously unknown allergic reaction;
- the drug was chosen incorrectly;
- the cosmetologist used an excessive amount of gel;
- the doctor performed the manipulation incorrectly.
Hematomas (bruises) occur due to microtrauma of blood vessels as a result of injections. Minor bruising is normal during injection procedures. Severe manifestations are usually associated either with vascular insufficiency or with the low qualifications of the doctor who performed the procedure. To ensure that swelling with hematomas goes away as quickly as possible, various local and systemic agents are used (in particular, products with heparin, Traumeel ointment, compresses).
If your face hurts and feels tight after contouring , you can talk about an individual reaction to the injection of filler. This symptom is usually associated with swelling 1-2 days after the procedure and subsequently goes away on its own. Regular painkillers will help relieve pain.
Relevance
Every year the popularity of such a branch of medicine as injection cosmetology is steadily increasing.
According to ASAPS (The American Society for Aesthetic Plastic Surgery), between 2014 and 2022 alone, the number of procedures using hyaluronic acid (HA) fillers increased by more than 58% [1]. The widespread use of such interventions makes it important for doctors to know not only about the benefits of a particular filler, but also about possible complications, side effects and methods for their correction. It is important to increase patient awareness of the potential risks associated with such injections. In modern literature, various reports of side effects after injection contouring are increasingly being published, most of which include hematomas, asymmetries, skin ischemia and necrosis, infections and allergic reactions [2].
Currently, various types of injectable fillers are used in cosmetological practice, which can be classified according to their origin (the most popular of them are HA in various modifications, calcium hydroxyapatite, poly-L-lactic acid, collagen) and the time of persistence in tissues (temporary, semi-permanent and constant) [3, 4].
Despite statements by manufacturers and various authors that HA fillers are as safe as possible in terms of immunogenicity or that the occurrence of such complications is extremely rare, side effects of this kind are still periodically observed. Systematic reviews have shown that all known HA-based fillers on the market are capable of causing early and late side effects. Their true prevalence is unknown but appears to be significant. The nature of most late side effects is inflammatory and immune-mediated. The most common occurrences are edema, granulomas, carcinophobic disorders and cellulite. Autoimmune reactions and immediate hypersensitivity are more rare [5].
In recent years, there has been great interest in studies of cases of delayed and persistent inflammatory reactions that occur after the administration of various excipients. According to some authors, infectious diseases [6], trauma [7], and vaccination [8] can be trigger factors.
Currently, the role of biofilm formation at the injection sites of fillers is being actively studied, because More and more researchers suggest that many cases of delayed complications arise due to its formation, and not due to the development of allergic reactions or other inflammatory response [9, 10].
Biofilms are a collection of microorganisms whose cells form three-dimensional structures by adhering to each other or to various surfaces. These microorganisms are capable of forming a matrix of extracellular polymeric substances (carbohydrates) around their colonies, which complicates the bioavailability of antibiotics and forms local resistance to them. There are five stages of biofilm formation: initial attachment, irreversible attachment, maturation I, maturation II, and dispersal. It is in the dispersion phase that the biofilm most actively forms its protective barrier.
After their formation, biofilms remain dormant (low-grade infection), but their activation with the occurrence of inflammatory reactions can be caused by trauma, hematogenous infection or iatrogenic manipulations [11].
Identification of biofilms is difficult. Cultures from biofilm-infected tissue are usually negative. Some authors consider fluorescence hybridization using peptide nucleic acid to be the most accurate in situ method [12].
Although HA-based fillers belong to the class of non-permanent fillers, a number of them are able to persist in tissues for 6 to 36 months [13], which provides bacteria with enough time to organize into biofilms.
As a clear illustration of the delayed immunoinflammatory response to the injection of HA filler, we present the following clinical case.
Clinical example
Patient N., 45 years old. She contacted the Department of Dermatology and Cosmetology of the JSC Institute of Plastic Surgery and Cosmetology with complaints of periodic swelling of the middle third of the face and pain in the area of the nasolacrimal groove and cheeks, pronounced pigmentation in the periorbital area after the injection of HA filler (Fig. 1).
From the anamnesis (according to the patient): about 1.5 years ago, 1 ml of HA filler was injected into the area of both nasolacrimal grooves and nasolabial folds. After the procedure, satisfactory correction was noted. 6 months after the injection of fillers, the patient suffered from severe infectious mononucleosis (she was hospitalized with meningitis). During hospitalization, she first noted the sudden appearance and intensification of swelling, pain, redness and hardness in the area of the nasolacrimal grooves and cheeks. The swelling increased during the day (Fig. 2).
In connection with this, an emergency consultation with a maxillofacial surgeon was carried out and a diagnosis of T78.3 (angioedema) was made. After drips with prednisone (three times), the patient noted an improvement. The swelling has decreased significantly.
After being discharged from the hospital a month later, the patient again noted swelling, pain, redness and hardness in the area of the nasolacrimal grooves and cheeks. She also began to notice the appearance and increase of diffuse symmetrical pigmentation in the periorbital area. The patient independently prescribed a course of antibiotic therapy, which she completed without effect. She also independently administered a single intramuscular injection of prednisolone (90 mg). After which she noted a significant decrease in symptoms.
Having associated her condition with filler injections, the patient turned to a doctor who had previously injected filler for its enzymatic resorption. After which, within six months, the negative symptoms resolved and were no longer observed.
Six months ago, the patient again turned to a cosmetologist to correct problem areas (nasolacrimal groove, cheeks, nasolabial folds).
The same filler used earlier was reinjected. After which, within 3 days, swelling, pain, and redness reappeared in the treated areas. When contacting a cosmetologist, intramuscular injection of dexamethasone and enzymatic resorption of the filler with hyaluronidase (one-time) were performed. A month later, the patient again noted the occurrence of periodic facial swelling in the area of filler injection, which was relieved by intramuscular administration of dexamethasone.
Objectively: at the time of examination there is no swelling of the face; painful lumps in the area of the nasolacrimal grooves (mainly on the right), the medial part of the cheeks and nasolabial folds are palpated. There is pronounced pigmentation of the periorbital and buccal area.
According to ultrasound examination, in the projection of the nasolacrimal grooves and nasolabial folds, residual inclusions of the drug are determined, which according to the ultrasound picture are characteristic of HA-based fillers. There is a local area of infiltrative changes (without a pronounced increase in blood flow) in the subcutaneous fatty tissue of the nasolacrimal groove on the right.
Diagnosis: L08.9 – Local infection of the skin and subcutaneous tissue, unspecified.
Treatment: amoxicillin + clavulanic acid 875 mg/125 mg once a day for 12 days; dexamethasone orally 1 mg/day for 20 days with a gradual reduction in dosage.
In the first 5 days of treatment, while taking the main medications, daily physiotherapy was carried out, consisting of the following sequence of procedures: ultrasound with dexamethasone, then pharmacophoresis with Longidase. Over the next 7 days, against the background of continued antibiotic therapy, enzymatic resorption of filler residues was carried out with hyaluronidase at a dilution of 3000 IU per 4 ml, using the technique of multiple injections and wide infiltration not only with the treatment of key areas, but also with the capture of surrounding intact areas (twice with an interval of 3 days) .
At the end of the course of treatment, a control ultrasound was performed, which revealed no signs of inflammation or residual filler fragments.
During therapy, a complete reduction of all the above-described clinical symptoms was noted. By the end of the course of therapy, there was a pronounced lightening of the pigmentation foci (Fig. 3).
Discussion
Potentially, any biomaterial injected and in contact with blood can sooner or later cause a wide range of side effects, both local and systemic. To date, there is not enough research and clinical experience regarding the treatment of these conditions. Management of both acute and systemic reactions is often difficult and requires an integrated approach using anti-inflammatory and sometimes immunosuppressive therapy. This problem requires further observations, development of diagnostic criteria and sound therapeutic protocols.
Conclusion
This clinical case is of potential interest for cosmetologists, dermatologists, plastic surgeons, and physiotherapists as an example of diagnosis, prevention and treatment of such pathological conditions.
Inflammatory processes at injection sites
A minor inflammatory reaction is considered a variant of the norm - it develops as a result of a foreign substance entering the body (despite the complete biocompatibility of hyaluronic acid with the human body, fillers trigger standard protection against “external invasions”). If the process takes place in 1-3 days, everything is fine, if it persists for a longer period:
- an infection has penetrated into the tissue - with injections (due to improper treatment of the skin before injections, or the use of a low-quality drug or consumables);
- the injection provoked an exacerbation of the infection, which was “dormant” in the tissues;
- There are autoimmune pathologies, against the background of which, as a result of the injection of filler, the patient begins to experience uncontrolled inflammatory reactions in the treatment areas.
To effectively treat a pathological condition, it is important to accurately determine the cause of its development; based on the results, the patient may be prescribed antibiotics, NSAIDs, antihistamines or steroids.
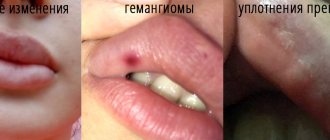
Lumps, lumps, fibrosis, granulomas
Consequences such as granulomas, fibrosis, compactions, lumps, contour plastic surgery usually result from non-compliance with hygiene rules, the use of uncertified fillers or the illiterate work of a doctor. Fibrous capsules are also formed due to the wrong choice of filler type or dosage; they should be treated with antibiotics and anti-inflammatory drugs. Lumps and lumps can resolve on their own; granulomas can be removed surgically.
What is facial contouring?
Facial contouring is a modern non-surgical method for correcting age-related changes, asymmetry, scars and adding volume to those parts of the face where it is lacking. It involves the use of special fillers with different compositions, which are drugs administered subcutaneously, intradermally or periosteally by injection. To perform them, ultra-thin needles of 27-30 G are used.
The essence of the method is to introduce a gel-like filler directly under the wrinkle, thereby creating a kind of depot of the drug. Thanks to this, it seems to push the tissue out, which leads to the smoothing of wrinkles, folds, and scars. If the task of contour plastic surgery is to create additional volume of the lips, cheekbones, temples, and chin, then the drug is administered evenly over the entire area of the corrected area of the face.
With the help of modern fillers it is possible to obtain an immediate effect, namely:
- improve facial contour and restore its clarity by eliminating tissue ptosis;
- reduce the depth of nasolabial folds and tear grooves;
- smooth out wrinkles and creases, including deep ones in the area between the eyebrows, forehead, and around the mouth;
- adjust the size of cheekbones, cheeks, temples;
- eliminate signs of facial asymmetry;
- smooth out dystrophic scars and scars, including post-acne;
- eliminate dark circles and hollows under the eyes;
- increase the volume of the lips and improve their shape, raise the corners;
- correct the shape of the nose (straighten the back even if there is a pronounced hump, improve the shape of the wings and tip of the nose);
- increase the volume of the chin, which is especially important for men.
Contour plastic surgery for the purpose of rejuvenation should be performed no earlier than 35-40 years. But to correct facial asymmetry, scars and add volume to lips or cheekbones, it can also be used at a younger age.
Today, facial contouring is a worthy alternative to plastic surgery and more traumatic cosmetic procedures. Its advantages include:
- absolute safety, especially when using biodegradable fillers;
- instant result that can be assessed immediately after the procedure, although the final effect is formed 1-2 weeks after contouring;
- duration of the effect (in most cases, the achieved result lasts 1-2 years);
- obtaining a natural effect, so others will never guess that the youth of the face is maintained with the help of a doctor;
- no need for anesthesia, which sharply reduces the number of contraindications for facial contour correction;
- no risk of scarring;
- the ability to solve a large number of problems in one session: enlarge lips, correct cheekbones, eliminate wrinkles, etc.;
- the simplest and shortest rehabilitation period possible.
At the same time, contour correction of the face with fillers is indeed one of the safest procedures. It has an extremely small number of contraindications, including:
- acute infectious diseases and exacerbations of chronic diseases;
- inflammatory processes in the area of correction;
- the presence of permanent (non-absorbable) fillers in the tissues;
- pregnancy and lactation;
- psychological disorders;
- taking antiplatelet agents and anticoagulants;
- oncological diseases;
- bleeding disorders;
- tendency to form keloid scars;
- allergy to any of the filler components.
Contouring is not recommended if you have recently undergone facial resurfacing or chemical peeling.
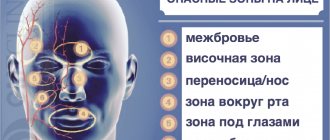
Vascular injuries (ischemia, embolism) after contour plastic surgery
Compression of blood vessels occurs when low-viscosity filler enters the vascular lumen or the drug is administered too deeply. During the day, pain increases, unhealthy redness may appear, severe swelling develops, and then necrosis with tissue scarring. This is the most severe, although rare, complication. Reasons for its appearance:
- a significant volume of gel was injected in close proximity to the vessel, as a result of which it strongly compressed it and closed the passage for blood;
- the filler entered directly into the vascular lumen, as a result of which it closed and the blood flow stopped.
Embolism and ischemia are characteristic of areas with an active blood supply - the nasolabial triangle, lips. The injured area is very painful, the area deprived of normal blood supply turns white, and a burgundy or blue mesh forms around it.
This condition requires an immediate response. Only a doctor can stop the situation, for which there are special protocols for administering the enzyme hyaluronidase and other methods of medical care to the patient.
Gel protrusions and migration
Migration, protrusion of the gel after plastic surgery is an extremely unpleasant reaction. The gel begins to appear outward, forms unevenness and blackheads, and with very thin skin it can appear as purple or blue spots. The reason for this phenomenon is insufficiently deep injection of filler. If the master injects the gel too deeply, the drug may begin to move to neighboring tissue areas and distort their proportions. The problem can be solved by introducing hyaluronidase, a component that breaks down and removes incorrectly administered hyaluronic acid.
Complications due to the use of non-absorbable gels for contouring
Biopolymer and silicone non-absorbable fillers are prohibited in most countries, but some homeworkers work with them. Patients are tempted by the affordable price and the “forever” result, and completely in vain. Over time, non-absorbable drugs begin to shift relative to the original injection area, distorting facial features. Inflammation and chronic infections often develop, and the body may simply begin to reject the drug. To remove gels, complex and expensive plastic surgeries are required, so do not skimp on beauty and health - in the end you will have to pay a lot more.
In order to avoid unwanted effects after contouring, trust only professionals, strictly follow all doctor’s recommendations, and if you have any disturbing symptoms, do not hesitate to immediately contact the clinic.
Be beautiful and healthy with GMTClinic!
Pain during contouring - myth or reality?
Thanks to unscrupulous players in the beauty market, potential clients have the impression that lip correction using fillers is a pleasant and painless procedure. But in reality this is absolutely not the case. Even the use of special anesthetic gels does not relieve pain. Subcutaneous manipulation with a needle is, to put it mildly, unpleasant, especially on such a sensitive area as the lips. Even those who have a fairly high pain threshold experience discomfort.
Manufacturers of lidocaine fillers claim that their solutions can reduce sensitivity by 35–40%. Cosmetologists also talk about positive experiences and slight swelling. But stories about serious complications that arise specifically from lidocaine-containing drugs are regularly covered in the media. Although we are mostly talking about overdoses or violations of sanitary standards.
An initial consultation with your doctor before the procedure is a wise thing to do. It is necessary to discuss with a specialist the selection of the drug, execution technique and contraindications. The doctor will take into account the individual characteristics of your body. This will help reduce the risk of side effects and eliminate allergic reactions.