Demodicosis is a disease that develops as a result of the spread of waste products of the pathogenic Demodex mite. The mite is localized on the skin of the face, eyelids, in the area of the superciliary arches, forehead, chin, near the ear canal and in the nasolabial folds. The disease is chronic and worsens during the off-season. In this case, the tick is not transmitted by airborne droplets, but progresses on the skin when the body malfunctions and the immune system decreases. You can also become infected with demodicosis through direct contact with a carrier of the disease or through bedding or clothing. Cases have been recorded in which domestic animals are carriers of Demodex mite disease.
The tick functions by feeding on sebaceous secretions or keratinized particles of the human epidermis. In this case, the tick has an oblong body that is covered with scales. Its presence can only be detected through laboratory testing, which involves analyzing the epidermis.
When is it necessary to take a demodex test?
Skin scraping for Demodex is carried out if there is a suspicion of damage to the epidermis by a mite of the Demodex family, which mainly affects people with metabolic disorders, a weakened immune system, adolescents, pregnant women, the elderly, problems with the gastrointestinal tract, chronic lung diseases or after emotional stress, nervous overstrain. Since this parasite feeds on sebum, its movement is reflected on the skin in a visible way.
The first signs of mite damage are peeling and redness of the epidermis, as well as the appearance of itching after the use of medicinal or cosmetic products or contact with a cold environment. Small pimples, ulcers or blackheads begin to form on the skin, which can be localized not only on the face, but also spread to other parts of the body. Sometimes demodicosis affects the eyelashes, which manifests itself in severe itching, swelling and the appearance of a viscous substance on the eyes in the morning, as well as the appearance of white scales at the roots of the eyelashes. The spread of the mite leads to rapid eye fatigue and swelling, which is similar to an allergic reaction.
If left untreated, the mite begins to multiply, which leads to enlarged pores on the skin and increased oiliness. Due to the presence of a large number of tick feces, the face takes on an earthy-gray tint. It becomes difficult for the patient to express emotions using facial expressions. In the evening, severe itching develops on the skin and in the eyelash area. Facial swelling occurs, which is expressed in an increase in the size of the nose or general swelling.
When the mite infests the hair follicles, partial baldness and damage to the eyelashes are observed. Nodules (papules) form on the skin and it becomes lumpy. At the same time, eyelashes fall out (without roots), hyperemia appears around the eyes.
Detailed description of the study
The problem of skin diseases caused by parasites is associated with their widespread distribution. Demodicosis is one of these diseases, its frequency is about 2-5% among the world's population. It is in eighth place among skin diseases in terms of occurrence. In addition, by affecting the skin of the face, demodicosis can lead to social maladjustment of patients and a decrease in their quality of life.
Demodicosis is a disease caused by mites of the genus Demodex. There are about 70 species of this genus, but only two are associated with this disease: Demodex folliculorum (longus), found in the follicular infundibulum, and Demodex brevis, found in the sebaceous and meibomian glands. The first of these, Demodex folliculorum, lives in hair follicles, while Demodex brevis lives in the sebaceous glands associated with hair follicles. Both are found primarily on the face, near the nose, eyelashes and eyebrows, but they are also found in other places on the body.
The viability of the tick remains outside the human body if factors such as constant humidity, darkness, and room temperature are observed. In such conditions, he can live for more than 8 days. The optimal temperature for tick life is considered to be 30-40°C; when it drops to 14°C, it goes into suspended animation, and at 52°C it dies. In an aquatic environment, it remains viable for up to 20-25 days. Favorable habitats for ticks are: vegetable oil, petroleum jelly or fat.
The Demodex mite is believed to be an opportunistic organism and lives on the skin of approximately 90% of people. In a normal state of immunity, these mites do not leave the boundaries of the surface layer of the skin, or rather the basement membrane. Mites live in hair follicles, feeding on secretions produced during normal skin function. If the normal functioning of the skin is disrupted in the form of changes in the secretion of the sebaceous glands, an increase in the amount of sebum; disruption of the endocrine, immune and nervous systems, as well as with prolonged external use of corticosteroids, the protective reaction of the skin changes. This promotes the reproduction of representatives of the genus Demodex.
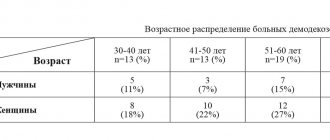
The disease occurs everywhere. The greatest activity of Demodex mites is observed in the spring and summer. This is due to an increase in ambient temperature. The prevalence of ticks depends on age. Thus, in the age group up to 20 years, demodicosis is detected in 20% of people who applied for frequent symptoms of this disease, in the period from 30 to 45 years - in 43%, and by 70 years of age - in 95-100%.
Clinical manifestations of demodicosis may include the following changes on the skin:
- Asymmetrical red spots;
- Spider veins;
- The appearance of areas of dryness and flaking of the skin;
- Lesions or diffusely altered skin thickening;
- Nodular formations are pink or red.
Often the symptoms of demodicosis are similar to the clinical picture that occurs with various skin diseases (acne vulgaris, rosacea, perioral dermatitis).
Mites can also cause damage to the eyelids, cornea and conjunctiva of the eyes (blepharokeratitis, blepharoconjunctivitis). When the eyes are affected, hyperkeratosis is noted with the presence of scales and a “collar” around the eyelashes, dysfunction of the meiboic and sebaceous glands. Patients complain of itching, a sensation of a foreign body in the eyes, swelling, burning and hyperemia of the edges of the eyelids and conjunctiva. The disease often remains unrecognized in time due to similar symptoms to a number of other skin and eye pathologies. Examination of eyelashes and skin scrapings helps determine the presence of these mites.
How to prepare for analysis
To obtain reliable information about the presence of a parasitic mite on the eyelashes or facial skin, the following rules must be followed before taking the test:
- Do not wash your face with products containing a high alkaline content for 24 hours before the test;
- stop using decorative and medicinal cosmetics, ointments and creams two days before visiting a doctor;
- Avoid contact with eyelashes with shampoo two days before the test;
- You cannot use eye drops the day before the procedure, with the exception of drops that are prescribed for serious eye diseases.
The parasitic mite is most active in the evening hours, as it does not tolerate ultraviolet light. Therefore, the most favorable time to submit a scraping for demodex is the evening hours. But in medical laboratories, material is collected for demodex in the morning, which can make it difficult to identify the causative agent of the disease, provoke its active reproduction and aggravate the patient’s condition.
Patient preparation
It is recommended to perform a demodex test in the morning.
To obtain an error-free and reliable result, it is necessary not to wash your face a day (or better yet, 2-3 days) before taking the test, not to put drops in your eyes and not to use decorative cosmetics, especially mascara.
Try to avoid getting shampoo, soap and other chemicals in your eyes. Previous course of antimicrobial therapy may also influence the outcome.
It is quite difficult to identify demodicosis in a patient, because the mite itself is active at night and is afraid of sunlight, so in order not to create additional obstacles to the detection of demodex, it is necessary to prepare in accordance with the above recommendations.
If these rules are neglected, there is a possibility of incorrect diagnosis.
How to test for demodex
The method of collecting material for scraping for demodex depends on the location of the mite and is carried out strictly in laboratory conditions.
Facial skin scraping involves examining particles of the epidermis that are taken from the affected areas. The doctor, using a scalpel or eye spoon, scrapes off the diseased particles of the epidermis or takes the contents of the pimple for examination. Testing for Demodex from eyelashes involves examining several of the patient's eyelashes. For analysis, the doctor takes four eyelashes from the lower and upper eyelids. Taking material for demodex testing is a painless procedure that can cause only slight discomfort to the patient.
The material taken for analysis is placed in a special solution (glycerin or alkaline) on a glass slide and examined under a microscope. The study consists of counting subcutaneous mite individuals.
Also, to determine the general condition of the patient and identify concomitant diseases (anemia, allergic reactions, inflammatory processes or bacterial infections), a general blood test is prescribed, which is recommended for all patients without exception.
Test for the presence of demodex
Demodectic mange is a disease that can cause serious discomfort, both physical and aesthetic. Often, attempts to treat acne, recurring blepharitis or eyelash loss do not work if the real cause lies in mite activity. In such cases, specialized treatment is required, selected by an experienced doctor.
Demodicosis can be detected by microscopic examination for the presence of demodex mites. This type of diagnosis is available at Diagnostic and Treatment Center No. 1, where you can take the necessary tests. Laboratory studies, their prompt implementation and guarantee of high accuracy are undertaken by INVITRO. Before collecting the material, the patient will be given recommendations regarding preparation. Test results are usually ready the next day.
Sign up for tests: +7 (4742) 37-02-52, +7 (4742) 37-03-52, +7 (4742) 37-04-52, you can also sign up online
When a positive result is given
When testing for demodicosis in a private laboratory, the patient receives the test result within an hour. State clinics provide results within 24 hours.
A positive diagnosis is made when a tick, its eggs or larvae are identified. If an empty shell of a parasitic mite is found on the skin, the demodex test is re-administered. If several individuals are detected within one cell, the result is considered conditionally negative and treatment is not prescribed, since this number of mites is not capable of harming human health (changes in appearance or hair).
When a parasite is detected, it is necessary to determine the type of tick (long or short), since this fact affects the duration of treatment and medication prescription. The shortest type is the most difficult to treat.
Indications for examination
Analysis for demodex must be carried out if there is:
The doctor's or patient's assumption of infection.- Clinical manifestations in the form of:
- affected ciliary margin;
- redness and inflammation;
- gluing eyelashes;
- severe scabies at the affected area;
- heaviness in the eyes;
- eyelash loss, which usually falls out without a root;
- the appearance of plaque or white scales on the eyelashes.
The danger is not the tick itself, but the products of its vital activity; it does not live long (up to 18 days in the larval stage and 5 days as an adult). When the tick dies, it begins to disintegrate, releasing toxins that subsequently lead to the appearance of unpleasant symptoms.
How much does the demodex detection procedure cost?
Depending on the place where the sample is taken for demodex scraping, the cost of the procedure varies. Moreover, the price of the study depends on the region of residence, the type of medical institution and the speed of obtaining the result.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: 23807 Date of publication: 09.28.2018
Dermatologists - search service and appointment with dermatologists in Moscow
References
- Fromstein, S., Harthan, J., Patel, J. et al. Demodex blepharitis: clinical perspectives. Clin Optom (Auckl), 2022. - Vol. 10. - P. 57-63.
- Jacob, S., VanDaele, M., Brown, J. Treatment of Demodex-associated inflammatory skin conditions: A systematic review. Dermatol Ther., 2022. - Vol. 32(6).
- Bitton, E., Aumond, S. Demodex and eye disease: a review. Clin Exp Optom., 2022.
- Elistratova, L.L., Potaturkina-Nesterova, N.I., Nesterov, A.S. Current state of the problem of demodicosis. Fundamental Research, 2011. - No. 9-1. — P. 67-69.
Diagnostics
To determine the disease, the patient requires a visual examination. The doctor then interviews the patient and orders a laboratory test. The materials that are taken for research (scrapings) are examined using microscopy - but the diagnosis of demodicosis does not end there. It happens that the result is negative - after which it is prescribed again. This is due to the fact that ticks are especially active in the evening and at night, and the analysis itself is usually taken in the morning, which can reduce the accuracy of the results. In addition, they may be affected by certain cosmetics - the skin should not be treated before the test.
The material is collected not only by scraping. To study the eye shape, several eyelashes are taken from the patient, and there is also a study using a special adhesive tape, which is stuck on at night and checked in the morning.
The examination of the material under a microscope itself takes only a few minutes, so the patient receives the result almost immediately.