The drug Lantox is a botulinum toxin type A drug, the action of which is to block the transmission of nerve impulses from the central nervous system to the muscle. As a result of the action of botulinum toxin, the overstrained muscle relaxes and the pain syndrome caused by muscle spasm stops. Lantox acts locally, without having a systemic effect on the entire body, so its use is safe. In dentistry, Lantox is used for pain caused by increased muscle tone, to treat bruxism, to normalize the functioning of the temporomandibular joints, etc., just like the drug Botox.
Advantages and disadvantages
Advantages of the drug:
- Price. Among known analogues it has the lowest cost - 30-40% cheaper.
- The effect is noticeable by the end of the first day.
- High duration - 8-10 months.
- Availability of a convenient dosage of 50 units.
- The risk of adverse reactions is reduced due to minimal diffusion into nearby tissues.
Disadvantages of the drug : cases have been recorded when the body begins to produce antibodies to the active substance, which will subsequently neutralize the effect of rejuvenation.
This drug is used by specialists:
- Avetisova Ksenia Nikolaevna
- Akulov Mikhail Albertovich
- Alifanova Irina Sergeevna
- Ambartsumyan Victoria Sergeevna
- Antipenko Elena Albertovna
- Artamonova Olga Grigorievna
- ASTAKHOVA ELENA VYACHESLAVOVNA
- Balbert Alexander Anatolievich
- Baranova Ksenia Vladimirovna
- Belan Lyudmila Petrovna
- Bolgova Daria Sergeevna
- Botsina Alexandra Yurievna
- Bocharov Vladimir Anatolievich
- Bubenchikova Natalia Alexandrovna
- Bychkova Natalya Yurievna
- Vaganova Olga Vladimirovna
- Vinogradov Konstantin Valerievich
- Glozman Oksana Mikhailovna
- Gontar Alena Alekseevna
- Gribanov Ivan Ivanovich
- Gulyashch Raisa Anatolyevna
- Dadasheva Marina Nikolaevna
- Ekusheva Evgenia Viktorovna
- Emelyanova Olga Alexandrovna
- Efremov Nikolay Sergeevich
- Zhukova Maria Viktorovna
- Zalyalova Zuleikha Abdullazyanovna
- Ibatullin Robert Alberovich
- Isagulyan Emil Davidovich
- Kapuler Olga Marselevna
- Karakulova Yulia Vladimirovna
- Karlova Olga Anatolyevna
- Kibisheva Amina Askerbievna
- Kislyakova Ekaterina Alexandrovna
- Konovalova Zagidat Narimanovna
- Korenko Lyudmila Alekseevna
- Krasavina Diana Alexandrovna
- Kulkova Tatyana Alexandrovna
- Kuramshina Elena Rifkhatovna
- Kutsemelov Igor Borisovich
- Kushnareva Victoria Vladimirovna
- Larkina Maria Alexandrovna
- Latysheva Nina Vladimirovna
- Lysenko Dmitry Dzhonovich
- Maslov Yaroslav Igorevich
- Mashkina Anastasia Sergeevna
- Melkumova Karina Aleksandrovna
- Melnikova Ekaterina Alexandrovna
- Meshcheryakova Irina Anatolyevna
- Minasyan Rimma Alexandrovna
- Mingazova Leniza Rifkatovna
- Mirsaev Tagir Rafailovich
- Moroshek Ekaterina Alexandrovna
- Mokhova Olga Igorevna
- Mugutdinova Bahu Tazhutdinovna
- Nabieva Asiyat Magomedovna
- Naprienko Margarita Valentinovna
- Narolskaya Svetlana Borisovna
- Novikov Andrey Gennadievich
- Novikov Dmitry Veniaminovich
- Amulet Lada Ivanovna
- Okuneva Olga Vyacheslavovna
- Oleynikova Yulia Vladimirovna
- Orlova Olga Ratmirovna
- Panchenko Dina Serafimovna
- Polyanskaya Svetlana Mikhailovna
- Pokhabov Dmitry Vladimirovich
- Putsyna Natalya Nikolaevna
- Rozov Roman Alexandrovich
- Romashova Daria Andreevna
- Sagildina Yulia Olegovna
- Sadchikova Elena Alexandrovna
- Sakanyan Margarita Babkenova
- Saxonova Elena Vladimirovna
- Salyukov Roman Vyacheslavovich
- Sanchez Elena Albertovna
- Slivko Mikhail Pavlovich
- Soboleva Anna Nikolaevna
- Soykher Marina Ivanovna
- Surovykh Svetlana Viktorovna
- Tanygina Tamara Anatolyevna
- Taran Marina Gennadievna
- Timerbaeva Sofia Leonidovna
- Tishaninova Victoria Viktorovna
- Tolmacheva Violetta Alexandrovna
- Tomsky Alexey Alekseevich
- Toropova Anna Albertovna
- Turchanova Rimma Leonidovna
- Falkovsky Ilya Viktorovich
- Fedyushina Elena Yurievna
- Feigina Anna Alexandrovna
- Filimonova Elena Viktorovna
- Filippova Larisa Ivanovna
- Khasanova Dina Rustemovna
- Khatkova Svetlana Evgenievna
- Khrustaleva Galina Mikhailovna
- Chechenov Alim Muaedovich
- Chirkova Olesya Alekseevna
- Shamrina Anna Mikhailovna
- Shemena Tatyana Nikolaevna
- Shchelokova Elena Borisovna
- Yakovleva Polina Nikolaevna
- Yaremenko Andrey Ilyich
Which is better: comparison table with Botox and its analogues
| Index | Lantox | Botox | Dysport | Xeomin | Neuronox | Relatox |
| Manufacturer country | China | USA | France | Germany | Korea | Russia |
| Best before date | 3 years | 2 years | 2 years | 3 years | 3 years | 2 years |
| Dosage, units (action units) | 50 units 100 units | 100 units | 100 units | 100 units | 50 units 100 units 200 units | 50 units 100 units |
| BB (excipients) | Gelatin, dextran, sucrose. | Albumin, sodium chloride. | Albumin, lactose. | Albumin, sucrose. | Albumin, sodium chloride. | Gelatin, maltose. |
| Mm. (molecular weight), kDa | 900 kDa | 900 kDa | 500 kDa | 150 kDa | 900 kDa | 150 kDa |
To read more about what is better - Botox, Dysport or Xeomin, read here, and here we told you what is better - Botox or hyaluronic acid.
Indications and contraindications
Indications. In cosmetology, the drug is used in the following cases :
- wrinkles in the forehead area;
- fold in the bridge of the nose;
- radial wrinkles around the mouth;
- facial asymmetry;
- wrinkles in the décolleté and neck area;
- as well as increased sweating of the palms, feet and armpits.
In addition to this, Lantox also has a number of other indications due to its relaxing effect on muscles:
- Treatment of muscle spasms.
- Strabismus.
- Hyperhidrosis (increased sweating).
- Pain syndromes (chronic headache).
Contraindications:
- Increased sensitivity of the body to the components of the drug (even to excipients).
- Pregnancy.
- Breastfeeding period.
- Hereditary disease - hemophilia.
- Inflammation at the correction site.
Price
The price for Lantox on average fluctuates around 250-300 rubles per unit. And the number of units required and the volume of product used is determined by the doctor individually with each patient.
But you can approximately estimate the consumption of the drug for each area of the face:
- Forehead area - horizontal wrinkles: 5-30 units.
- Vertical wrinkles between the eyebrows: 15-30 units.
- Crow's feet - area around the eyes: 10-20 units.
- Nose wings: 2-10 units.
- Oral area: 4-16 units.
- Neck and décolleté: from 60 units.
- Armpits: 6-200.
How are injections performed?
All drugs containing botulinum toxin are administered according to the same regimen . The procedure must be performed by a cosmetologist who has undergone appropriate training.
- At the beginning, the doctor must examine the patient, collect a medical history, and find out whether the client is currently taking any medications.
- Next, the specialist assesses the condition of the skin, conducts facial tests and selects the necessary correction scheme.
- The cosmetologist must inform the client about the drug, its composition, contraindications, restrictions and the presence of adverse events.
- Then informed consent is given for signature. And after signing it, they begin the procedure.
If the client wishes, the cosmetologist can administer anesthesia. The procedure takes from 10 to 30 minutes.
Independent use
Is it possible to inject at home?
Independent use is strictly prohibited . And you cannot purchase it yourself, since it is sold only to specialized medical institutions.
Instructions for use
In most cases, Lantox is administered intramuscularly, but it can also be administered subcutaneously.
It is never used in its pure form - it is diluted by adding saline solution, hyaluronic acid or vitamins.
For hyperhidosis of the palms, feet or axillary area, Lantox is administered subcutaneously . And in order to smooth out wrinkles:
- Two subcutaneous or intramuscular injections are made in the forehead area at a distance of 2 centimeters from each other.
- One subcutaneous injection into the orbicularis oculi muscle.
- Two symmetrical injections are made into the nasal area.
- Intramuscularly into the chin area at two symmetrical points.
- Neck and décolleté area - injection into the area of the thyroid cartilage.
Cost of the procedure
Thus, on average, when correcting facial wrinkles, the cost of the drug per procedure will be from eight to fourteen thousand rubles. When eliminating excessive sweating of the armpits from twenty thousand rubles, and when correcting the décolleté and neck from ten to fifteen thousand rubles.
But we must not forget that the average costs are given for the Central region of Russia, for a clinic at the level of a licensed and certified cosmetology or aesthetic center. If the proposed contract specifies a significantly reduced price for the drug, it is worth thinking about the originality of the proposed product, the quality of services and the professionalism of the cosmetologist.
Rehabilitation process
The period after Lantox administration is important. And the duration of the effect and its manifestation, as well as the presence or absence of side effects, will depend on it.
Here are some recommendations to follow after “beauty injections”:
- In the first 3-4 hours after injections, it is forbidden to take a horizontal position.
- Do not rub the neurotoxin injection site.
- Do not abuse alcohol.
- It is recommended not to visit saunas, steam rooms, etc. for several weeks, as they, similar to the effects of alcohol-containing drinks, increase blood flow, which increases the area of distribution of the drug.
- It is prohibited to take antibiotics during the first 2 weeks.
About the results
When and what will be the effect?
The first result can be expected within a few days.
And the maximum effect of the procedure is observed in the first two weeks. As a result of the action of botulinum toxin on the muscles, they relax. Outwardly, this manifests itself in a decrease in the depth and size of wrinkles, which refers to deep, senile wrinkles. And if it is small, it can disappear completely. In addition to the fact that the result of this procedure is getting rid of wrinkles , there is also a pleasant additional bonus - the body, as it were, “forgets” about previously existing facial wrinkles. In other words, a person stops straining some facial muscles and the fact that the depth and size of wrinkles are worsening will not bother him.
How long does it last?
The effect of the procedure lasts on average half a year.
But it can reach a longer period - 10 months. This will be determined by the individual characteristics of the human body.
Is correction required?
Sometimes correction is required:
- To correct vertical wrinkles above the lip, it can be injected subcutaneously and intramuscularly into one point (in the middle of the upper lip) or into two. The choice depends on the desired result (for example, raising the corners of the mouth).
- To correct the chin - at two symmetrical points.
- When correcting the oval of the face, it is injected subcutaneously into 2 points located along the edge of the lower jaw, at a distance of 2 cm.
Side effects
Side effects are very rare and poorly studied. But nevertheless they exist:
- slight bruising at the injection site;
- development of an inflammatory process at the site of drug administration;
- painful sensations in a certain area of the face;
- swelling;
- headache;
- allergic reactions;
- facial asymmetry resulting from the unequal location and number of capillaries on the face;
- the effect of the so-called “mask” of the face, which occurs due to an overdose;
- drooping upper eyelid and sagging lower eyelid;
- involuntary blinking.
Surgical treatment of tumors of the posterior and middle cranial fossa—acoustic neuromas, petroclival meningiomas, brainstem tumors, and traumatic injury to the pyramid of the temporal bone is associated with the risk of developing dysfunction of the trigeminal and facial nerves [4].
Combined lesion n. trigeminus, n. facialis
and
n.
petrosus major in the latter leads to changes in the sensitivity of the cornea, impaired lacrimation and lagophthalmos. This is the cause of the development of trophic keratopathy, erosion, and corneal ulcers. As a rule, damage to the cornea occurs in the optical zone, so visual functions suffer and visual acuity decreases. In addition, lagophthalmos leads to aesthetic discomfort for the patient [3]. At the same time, the severity of trophic disorders is directly dependent on the volume of the tumor being removed, and therefore can be predicted in the preoperative period [4].
To prevent and treat trophic keratopathy, drug therapy is usually used, including keratoprotectors of varying degrees of viscosity. However, it is not always possible to stop the development of trophic keratopathy only with the help of keratoprotective therapy. With the development of a particularly severe form of corneal-conjunctival xerosis, emergency and temporary “help” for the cornea is needed. M. Naik et al. [10] in 2008 proposed the use of botulinum toxin A (BTA) injections into the projection of the levator palpebrae superioris muscle in order to obtain induced ptosis.
Various doses of BTA are given in the literature. Thus, J. Prell et al. [12] suggest administering 25 U of BTA to obtain temporary drug-induced ptosis, and M. Ellis, M. Daniell - 5 U of BTA [7].
BTA was used to obtain temporary drug-induced ptosis for the correction of lagophthalmos and trophic keratopathy in neurosurgical patients. A number of authors [8, 9] used Botox in their works. Our choice fell on Lantox.
There are successive stages of BTA action. At the first stage, the BTA molecule binds to the presynaptic membrane, then the associated toxin is internalized into the cytosol through endocytosis, which at the third stage leads to a blockade of the release of acetylcholine from the presynaptic endings of cholinergic neurons. The end effect of this process is persistent chemodenervation. 10-30 days after the injection, the process of development of additional axonal processes begins, which, growing, form new active neuromuscular synapses, which ultimately leads to the restoration of muscle contractions.
The purpose of this study is to evaluate the effectiveness of temporary drug-induced ptosis obtained by injecting the drug Lantox into the projection of the levator palpebrae superioris muscle in neurosurgical patients with lagophthalmos and trophic keratopathy.
Research objectives:
1. Determine the indications for receiving temporary drug-induced ptosis in neurosurgical patients with lagophthalmos and trophic keratopathy.
2. Determine the method of administration and duration of action of BTA when obtaining temporary drug-induced ptosis.
3. Assess the dynamics of the severity of lagophthalmos and trophic changes in the cornea after BTA injection.
Material and methods
The study was conducted from October 2008 to June 2011 at the Research Institute of Neurosurgery named after. N.N. Burdenko. To obtain induced ptosis, lantox was used, which is a local muscle relaxant and is a sterile, lyophilized form of purified BTA isolated from the culture medium of the bacteria Clostridium botulinum
.
Treatment was carried out on 66 patients (44 women and 22 men) aged from 11 to 67 years (average 52 years).
55 patients had space-occupying lesions of the cerebellopontine angle. 40 had acoustic neuroma (of which 3 patients had neurofibromatosis type 2), 12 patients had petroclival meningioma (of which 4 had meningioma of the posterior surface of the temporal bone), 2 had petroclival cholesteatoma, 1 had a combination of neuroma and meningiomas of the cerebellopontine angle. The group with other diseases included 11 patients: 1 - with hyperstatic cranio-orbital meningioma, 2 - with dural arteriovenous fistula, 1 - with meningioma of the middle cranial fossa, 2 - with trigeminal neurinoma, 3 - with a tumor of the fourth ventricle, 1 - with a ruptured aneurysm right middle cerebral artery, 1 - with traumatic brain injury, fracture of the temporal bone.
Of the group of patients, 50 were admitted initially, 16 were admitted repeatedly. One patient had undergone 4 surgical interventions at the time of Lantox administration. Tumors were removed in 62 patients: total tumor removal in 32, subtotal tumor removal in 30. 15 patients received radiation treatment (radiotherapy or radiosurgery) after surgery due to continued tumor growth. Four patients with diagnoses of dural arteriovenous fistula (2 patients), aneurysm of the bifurcation of the middle cerebral artery (1), condition after severe concomitant trauma (1) underwent cerebral angiography or surgery on cerebral vessels, or ventriculoperitoneal shunting.
In addition to a standard neuro-ophthalmological examination, including determination of visual functions - visual acuity, visual fields, function of the V pair of cranial nerves, pupillary reaction to light, degree of eyelid closure, oculomotor functions and convergence, examination of the fundus using direct and reverse ophthalmoscopy - biomicroscopy of the anterior segment of the eye with staining of the cornea with a fluorescein solution, determination of the stability of the precorneal tear film, a measurement method for which was proposed by M. Norn [11] in 1969.
The injection was carried out through the superior orbitopalpebral groove in the amount of 10-25 units at 1 or 2 points. In our study, 46 injections were made at 1 point and 34 injections at 2 points.
With injections of 15 U of BTA, the optimal ratio of complete ptosis/incomplete ptosis/no reaction to injection was obtained (Table 1).
Contraindications to the administration of Lantox were allergic diseases and a history of hypersensitivity to the drug. Lantox injections were not performed in the acute stage of infectious and non-infectious diseases.
Due to the development of incomplete drug-induced ptosis, 2 patients were given repeated doses of Lantox 5–14 days after the first injection. Due to the end of the effect of BTA and the worsening of neurotrophic keratopathy, subsequent injections were made after 2.5 months or more. During these periods, it is possible to re-administer BTA without the formation of antibodies to the latter.
One Lantox injection was given to 55 patients, three to 3 patients, two to 7 patients. One patient received one BTA injection into the binocular projection of the levator palpebrae superioris muscle. A total of 80 injections were performed.
results
The indication for the use of Lantox in the majority of patients (53) was the presence of lagophthalmos and the development of corneal-conjunctival xerosis of varying severity in the absence of positive dynamics from keratoprotective therapy. With the initial degree of lagophthalmos, the lower sector of the cornea suffered; the more pronounced the lagophthalmos was, the larger the area of the cornea was damaged, affecting the optical zone and leading to a decrease in visual functions.
We regarded drug-induced ptosis as an “ambulance” for the acute development of trophic keratopathy, erosion or corneal ulcer. This was a means of preventing the development of more severe and profound changes in the cornea.
In 18 patients, dysfunction of n. was observed before surgery. facialis
in the form of weakened squinting - a symptom of eyelashes - in 17 patients (on the House-Brackmann scale - 2-3) and lagophthalmos in 1 patient (on the House-Brackmann scale - 6).
After surgery, dysfunction of n. facialis was present in 62 patients: 2 had weakened squinting, 60 had lagophthalmos of varying severity (Table 2).
Dysfunction of n. trigeminus
before surgery, it was detected in 53 patients: in 38 the corneal reflex was reduced, in 15 it was absent.
Before surgery, 50 patients had no signs of trophic keratopathy (Table 3).
After surgery, dysfunction of
n.
trigeminus was observed in 57 patients, and with a decrease in the corneal reflex, severe corneal-conjunctival xerosis was more often detected, and in the absence of a corneal reflex, in most cases, particularly severe corneal-conjunctival xerosis occurred, manifested by xerotic erosion or corneal ulcer.
In 4 observations, Lantox was administered to patients due to severe xerosis of the cornea with dysfunction of only n. trigeminus
, without changing function
n.
facialis .
In 9 cases, patients with severe lagophthalmos that developed after surgery received BTA injections without signs of trophic keratopathy in order to protect the cornea in the early postoperative period.
The tear film breakup time in all patients was less than 5 s, which indicated severe dry eye syndrome [6].
The onset of action of BTA was observed on days 1–7 (median: day 3) after injection.
Complete drug-induced ptosis developed within 1–17 days (median 3 days) and persisted for 6–150 days (median 20 days).
This was followed by a period of residual semiptosis until the complete completion of the action of BTA. The end of the action of botulinum toxin was observed on days 27–182 (median day 46) after injection (Fig. 1).
Figure 1. Distribution of the effects of BTA on the musculus levator palpebrae superioris depending on time parameters.
In 1 patient, complete ptosis lasted 150 days. We can explain such a long-term effect of BTA by individual sensitivity to the drug.
19 patients (21 injections) developed hemiptosis. The median duration of semiptosis was 30 days (Fig. 2).
Figure 2. Chemodenervation options.
In 2 patients there was no reaction to a double dose of the drug and in 1 patient - to a single dose. We attributed the first two cases to primary resistance to BTA [1], the third patient was not given a second injection for technical reasons.
There were no complications in any case. Side effects: in 2 cases - hemorrhage at the injection site, which regressed within a few days, in 6 - vertical strabismus associated with diffusion of BTA into the superior rectus muscle, which regressed with the end of the action of BTA.
Thus, the overwhelming majority of patients achieved the desired effect in the form of ptosis or severe semiptosis. This led to regression of trophic changes in the cornea with complete drug-induced ptosis and a significant decrease in keratopathy with incomplete ptosis in all patients.
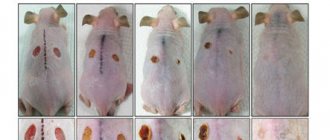
In 59 of 66 patients, we observed good results - gradual adaptation of the eye with lagophthalmos, absence of keratopathy or minimal defects of the corneal epithelium (Fig. 3-5).
Figure 3. Lagophthalmos before BTA injection.
Figure 4. Drug-induced ptosis after BTA injection.
Figure 5. 1 year after surgery and medical ptosis. All patients received and continue to receive keratoprotective therapy. In 7 patients, after the end of the action of BTA, trophic keratopathy developed again, and therefore partial bloody blepharorrhaphy was performed.
Discussion
The process of tear production is a reaction to a stimulus that, arising in the anterior segment of the eye, along the sensory fibers n. ophthalmicus
passes to the sensory nuclei of the trigeminal nerve, located in the dorsolateral corner of the pontine tegmentum.
Most of these fibers form the spinal tract, to which sensory fibers from the intermediate nerve are attached. The nuclei of the facial nerve are located in the floor of the fourth ventricle of the brain. In the facial canal, n. departs from the intermediate nerve .
petrosus major , formed by preganglionic parasympathetic fibers, which are processes of cells of the superior salivary nucleus. This nerve, connecting with the fibers of the sympathetic nerve from the internal carotid plexus, is responsible for the autonomic innervation of the lacrimal gland. Thus, the reflex arc is closed and tear secretion is produced, which is disrupted when the volumetric process affects the V and VII cranial nerves or damage to the latter during surgery [4, 5].
So, with a combination of damage to the V and VII cranial nerves, our patients developed the following symptom complex: against the background of lagophthalmos of varying severity, corneal sensitivity and tear production were impaired. As a result, trophic changes in the cornea developed - corneal-conjunctival xerosis, trophic erosion, corneal ulcer. Thus, with the initial degree of lagophthalmos, trophic changes were observed in the lower sector of the cornea, and with an increase in the degree of lagophthalmos, a large area of the cornea was damaged and the optical zone was captured.
In most patients, trophic changes in the cornea developed despite the adequate use of keratoprotectors. Some patients, in the complete absence of the corneal reflex, did not experience discomfort, which led to a loss of motivation to use keratoprotective therapy in the prescribed mode and volume; as a result, trophic keratopathy worsened and trophic erosion or corneal ulcer developed (in 16 patients). Receiving medicinal ptosis was an adequate urgent help in the development of acute conditions of the cornea caused by trophic disorders in it when only keratoprotective therapy was insufficient. Moreover, trophic changes in the cornea were the main indication for this injection, although the presence of severe lagophthalmos with minimal xerotic corneal changes also required induced ptosis.
The use of lantox to obtain induced ptosis is a safe method for correcting trophic changes in the cornea. The side effect of diplopia due to the development of vertical strabismus associated with the diffusion of BTA into the superior rectus muscle does not cause significant discomfort in patients due to temporary monocular vision with the development of complete drug-induced ptosis or severe semiptosis. Diplopia regresses with the end of BTA action.
The timing of the development and continuation of induced ptosis that we obtained coincides with the results presented by European authors.
For long-term changes in the cornea that affect the stroma, such as a corneal cataract, Lantox is not effective.
conclusions
1. BTA is indicated for obtaining temporary drug-induced ptosis in neurosurgical patients with lagophthalmos in the early and late postoperative periods in the presence of trophic keratopathy, trophic erosion or corneal ulcer when keratoprotective therapy is ineffective.
2. The effect of BTA was obtained in the vast majority of patients. The optimal dose of BTA to obtain induced ptosis is 15 units, regardless of whether it is administered into 1 or 2 points. Side effects were minimal and resolved quickly.
3. During complete drug-induced ptosis, trophic keratopathy completely regressed; during drug-induced semi-ptosis, the manifestations of trophic keratopathy decreased significantly.
A comment
A long way has come since the introduction of botulinum toxin type A (BTX-A) into clinical practice in 1980. Given the widespread use of BTX-A in medicine, its expansion in the aesthetic field is especially impressive. The development of ptosis of the upper eyelid after the so-called “youth” injection in the periorbital region is far from an exclusive complication. In case of exposure corneal pathology, it seems logical to use VTX-A as a “temporary tarsorrhaphy” or “non-surgical tarsorrhaphy” (M. Ellis, M. Daniell, 2001; M. Fernandes et al., 2008; U. Wollina, H. Konrad, 2005; J. Woodward, 2010). Unfortunately, only a few studies are devoted to this topic, which often include only a few patients, for example, 3 cases of successful use of protective ptosis in the treatment of recurrent corneal erosions (I. Mackie, 2004).
In the article by T.B. Tabashnikova et al. The results of the use of drug-induced ptosis on a sufficient number of patients (66) with neurosurgical pathology and ophthalmosymptoms represented by exposure and trophic keratopathy are analyzed. In all patients, BTX-A injections were performed for corneal decompensation using the maximum regimen of corneoprotective drugs. The results of treatment of patients with a combination of exposure and trophic keratopathy obtained by the authors are of great practical and scientific interest.
It is not entirely clear why a higher dosage of the drug (20-25 units) did not lead to an increase in the incidence of complete ptosis. It also seems interesting in the future to monitor the effect of BTX-A injection on the severity of the Bell reflex and tear production, the impairment of which can lead to worsening of the cornea.
In this group of patients, it is advisable to use humidifying chambers, external weights, and placement of lacrimal occluders. However, for various reasons, these time correction techniques are rarely used in the Russian Federation. In this connection, in our country, even with acute paralytic lagophthalmos, tarsorrhaphy is often performed. But given the temporary nature of the pathology, after dissection of the artificial ankyloblepharon, changes in the edges of the eyelids often remain. Some changes in the eyelids may occur after the introduction of hyaluronic acid gel into the upper eyelid (Ya.O. Grusha, E.I. Agafonova, Yu.F. Ivanchenko, 2010—2012).
Thus, for the first time, on a sufficient number of patients, it was shown that the use of chemodenervation of the levator of the upper eyelid made it possible to obtain positive dynamics in the condition of the cornea in 59 patients, the optimal dosage of BTX-A was substantiated, and the effectiveness of repeated injections of the drug was presented.
Ya.O. Pear
(Moscow)
Can the product be used in combination?
Before performing the procedure, you should always ask what medications you are currently taking.
And this is not easy. After all, their interaction with Lantox, and in particular with botulinum toxin, leads to serious consequences. Banned drugs include aminoglycoside antibiotics (for example, gentamicin). They are dangerous because they increase muscle paralysis.
Also, the following are not allowed for joint reception:
- Medicines that have the same effect - muscle relaxant - because the effect is similar to the previous examples, intensify.
- Antidepressants (also affect muscle condition).
- Aspirin-based medications, when used together, can cause bruising, swelling, and bleeding.
- Antipsychotics - due to the risk of damage to the nervous system (it is recommended to stop taking them a month before).
Alcohol compatibility
All alcoholic drinks contain ethanol.
It is quickly absorbed and enters the bloodstream. Acting on the walls of blood vessels, it reduces their tone, thereby promoting their expansion. As a result, blood flow and metabolic processes increase. And the interaction of botulinum toxin with alcohol will lead to the fact that it will quickly diffuse when it enters the body.
Consequences of compatibility with alcohol:
- small hematomas will appear at the injection site, and hemorrhage is also possible;
- swelling;
- weakening of injected muscle groups;
- the occurrence of symptoms of general intoxication and much more.
Carrying out manipulation - step-by-step instructions
The manipulation of the administration of any botulinum toxin must be carried out in a specialized medical center, in which all specialists performing this operation must be certified and have the appropriate permits to work with this drug:
- Before the procedure, you must make sure that Lantox was stored at the required temperature: -5/-20 degrees.
- The packaging must be intact, without traces of tampering.
- The cosmetologist must collect all the basic information about the patient’s health status, whether there are any allergic reactions to protein or gelatin of animal origin. The doctor must also make sure that there are no neuralgic diseases, allergic risks, etc.
- The doctor should then evaluate the condition of the skin at the injection site. It is unacceptable to inject botulinum toxins into areas with irritated skin, inflammatory formations, urticaria, etc.
- Next, facial contractions are assessed and a correction plan is developed based on the client’s wishes and the doctor’s recommendations.
- The skin is treated with an antiseptic, and the planned injection points are applied.
- The doctor must provide maximum information about the product, inform the client about contraindications and side effects, and obtain written consent from the Client for the manipulation.
- Next, local anesthesia is performed with an anesthetic gel.
- The product is diluted only in the presence of the patient.
- Injections are administered according to the developed plan for correction of the face or neck.
Storage rules
The drug is stored out of the reach of children, at a temperature of -5 to +20 degrees.
You can find out about other Botox analogues in the following articles:
- Korean botulinum toxins.
- Refinex.
- Botox Allergan.