When red bumps appear on the tongue, at the tip or closer to the throat, you need to find out what this phenomenon is. Such rashes often bother not only adults, but also children. And since they arise for a wide variety of reasons
, you need to figure out whether pimples pose a danger and choose the optimal treatment method.
What is glossitis?
Glossitis (from the Greek glossa (tongue) + suffix –itis) is an inflammation of the tongue. The reasons for its occurrence are different. Glossitis can develop as a result of a viral or bacterial infection, or as a result of another disease in the body. In addition, there are some other factors that provoke the development of the disease. These include mechanical, chemical and thermal damage to the oral cavity; nicotine; food that is too spicy or too hot; alcohol; caramel; some components present in toothpastes.
Glossitis has the following forms:
- folded
- diamond-shaped median
- desquamative
- hairy black
- Gunter's
- interstitial
According to the duration of the inflammatory process, acute and chronic glossitis are distinguished. The acute form of glossitis manifests itself as inflammation of the tongue, a change in its structure or color. Symptoms of the chronic form are more varied, but in most cases the disease is diagnosed by the presence or absence of papillomas - fungal growths on the tissues of the tongue. There are cases when the cause of the disease can be identified only after comprehensive medical research. True, this happens quite rarely and, as a rule, is associated with the presence of congenital, hereditary diseases.
Preventive measures
Simple preventative measures will prevent the onset of the disease. Basic rules of behavior and hygiene:
- Fruits and vegetables should always be washed before consumption.
- Food should not be excessively hot, cold, spicy or rough.
- The chewing process should be slow, which will prevent tongue biting.
- Personal hygiene should be observed: dental and oral care.
- It is necessary to have individual cutlery and a toothbrush.
- The brush should be renewed monthly. Change immediately after an illness.
- Regular visits to the dentist are recommended. It is necessary to treat diseases of the teeth and oral cavity in a timely manner, remove tartar and plaque, because these are the main sources of infection in the mouth.
- It is necessary to maintain adequate physical activity, which will increase immunity and the condition of the entire body.
Any pimple, growth or tubercle on the mucous membrane, both in an adult and in a child, requires close attention. You should not treat the bumps yourself; only a doctor can do this.
You should not pierce or try to squeeze out pimples on the mucous membrane; such actions can lead to negative consequences: the growth of foci of inflammation, the appearance of open wounds as a result of injuries.
The best thing a person can do if they have bumps on their tongue is to see a dentist or therapist. Such a decision will speed up recovery and prevent possible complications.
Main symptoms of glossitis
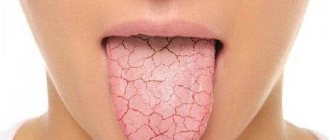
Glossitis, the symptoms of which are very diverse and largely depend on the cause of the disease and the stage of development of the process, but the following signs are almost always present:
- coating on tongue uneven with spots
- ulcers in the oral cavity of varying depth and extent
- color changes (general or in the form of local spots)
- swelling of the tongue, the presence of “imprints” of teeth on its lateral surfaces and other sores
- limited tongue mobility
- bad breath problem
- salivation disorder
Often these changes are accompanied by a decrease in taste sensitivity, a burning sensation and pain at the slightest movements of the tongue while eating and when talking. Sometimes, as the inflammatory process progresses, there is a deterioration in general health: an increase in temperature, enlargement of the submandibular and cervical lymph nodes.
Types of disease
Depending on the prevalence of the process and the predominance of a certain nature of changes, the following are distinguished:
Catarrhal glossitis
It is manifested by swelling, redness of the tongue, and the appearance of plaque on its surface, but the process does not extend to its deeper layers. Most often, catarrhal glossitis occurs with superficial injuries and burns of the tongue (chemical, thermal), oral candidiasis (disturbance of the balance of normal microflora), various forms of stomatitis, infectious diseases (viral and bacterial nature), as well as with a number of diseases (anemia, hypovitaminosis , metabolic disorders, diseases of the digestive system, etc.).
Ulcerative glossitis
It is usually manifested by the formation of single or multiple small ulcers on the tongue (the so-called aphthae, hence another name for it - aphthous glossitis). Ulcerations are often accompanied by bleeding, severe swelling, severe pain and deterioration in general condition. This type of glossitis can develop from catarrhal glossitis, and also be a manifestation of diseases of the oral cavity, gum diseases, and diseases of internal organs.
Purulent-phlegmous glossitis
It is a severe form of inflammation, spreading not only to the deeper layers of the tongue, but also to other tissues of the oral cavity; the nearby lymph nodes are also involved in the process. In this case, the patient’s condition is serious, with severe intoxication and elevated temperature, so such patients are usually treated promptly. Antibiotics for this glossitis are a mandatory component of treatment.
Special types of glossitis and their treatment
In addition to the above types of glossitis, dentists distinguish special types of glossitis, characterized by the development of limited specific changes in the tongue. These include:
Desquamative glossitis
It appears in the form of a “geographical” tongue, which has a “variegated” pinkish-red appearance, somewhat reminiscent of the outlines of the continents on a geographical map. In some cases, with the development of the inflammatory process, thinned areas cleared of plaque may change their position and shape within a short period of time (2 - 4 days). In such cases, desquamative glossitis is also called wandering glossitis. This can usually be observed with exudative diathesis, diseases of the digestive system, helminthic infestations, metabolic disorders, blood diseases, pregnant women, etc. Desquamative glossitis involves standard treatment, which leads to a gradual cleansing of the surface of the tongue and the disappearance of associated complaints in the patient.
Median rhomboid glossitis
It is characterized by the presence of a local thickening of the epithelium, usually located in the middle of the back of the tongue. In this case, the thickened area of the epithelium has a diamond-shaped or oval shape and can change its color from red to bluish. Rhomboid glossitis most often occurs in chronic diseases of the digestive system and is prone to chronicity and recurrence. Depending on the form of glossitis (flat, tuberculate, papillomatous), appropriate treatment is carried out: laser therapy, surgery, etc.
Atrophic glossitis
It often develops with insufficient intake of vitamins A and E. It usually appears as a single bright red, smooth spot that occupies the entire surface of the tongue. The focus of atrophy can persist for quite a long time without progressing. Sometimes the tongue decreases in size. Histological examination reveals dilation of blood and lymphatic vessels, swelling and inflammation in the papillary layer. Often, atrophic glossitis is a symptom of tongue damage due to gonorrhea.
Gunter's glossitis
Appears with a deficiency of vitamin B12 and folic acid. It most often occurs with blood diseases (usually anemia associated with impaired hematopoietic processes). In this form of the disease, the surface of the tongue is bright crimson in color and, due to atrophy of the papillae, has a “varnished” appearance. Gunter's glossitis involves treatment of the underlying disease by a therapist or hematologist.
Mycotic, candidal, or yeast glossitis
As a rule, it is a consequence of intensive antibacterial therapy, as a result of which the normal microflora in the patient’s body was suppressed. The disease manifests itself as swelling of the tongue, an accumulation of white plaque on it, with pronounced longitudinal and transverse grooves. Very often, mycotic glossitis occurs in young children and the elderly, as well as in people with weakened immune systems. Candidal glossitis requires treatment with antifungal drugs.
As an additional means for the treatment and prevention of glossitis, many experts have recently begun to recommend the use of an ultrasonic brush for oral hygiene.
Pimples appeared on the tongue: treatment at home
Having determined the nature of the rash, the doctor can prescribe a comprehensive treatment of the disease (drug and herbal treatment) or non-drug treatment at home. Pimples on the root, tip, and near the frenulum of the tongue can be removed using folk remedies.
Herbal medicine
Herbal decoctions and infusions effectively remove pimples both on the tip and at the base of the tongue. The most effective rinses are chamomile, St. John's wort, and calendula. Herbal decoctions are especially effective when the rashes are inflamed.
Method for preparing the decoction: pour a teaspoon of herbs into a glass of boiling water, leave for about 15 minutes, and cool. You need to rinse your mouth 2-4 times a day.
Infusions and decoctions can be taken orally, this will help alleviate the symptoms of the disease, relieve inflammation, and help stabilize metabolic processes.
Compresses and lotions
If the formations are inflamed, pain and inflammation can be relieved by applying a cotton swab moistened with a herbal decoction of chamomile and calendula to the affected surface.
You can numb the surface of the tongue using therapeutic and prophylactic toothpaste, which is applied for 2 minutes. The paste relieves pain, has a calming, anti-edematous and anti-inflammatory effect.
Rinsing with antiseptic solutions
They help treat inflammation of the mucous membrane, eliminate tubercles on the tongue both at the very beginning and closer to the throat. In the fight against the disease, the use of Chlorophyllipt and Chlorhexidine is common. The preparations can be used as rinses and are effective for irrigating the oral cavity. Procedures are carried out several times a day.
Manifestations of tongue glossitis in children
In children, glossitis usually occurs at an early age - from 1 to 5 years. The causes of this pathological process have not yet been fully studied and can be very diverse: from infection to poor heredity. Externally, glossitis in children is manifested by the appearance of spots on the tongue, which slightly swells and itches. Itching and a burning sensation are the most unpleasant signs of glossitis, since a small child begins to scratch the tongue, thereby contributing to the appearance of microcracks with their subsequent infection. However, the disease does not pose a threat to the child’s life. The famous pediatrician Komarovsky does not recommend panicking about this and self-medicating by giving the baby serious medications. As a rule, multivitamins and a gentle regimen will have a positive effect within a week.
Causes of herpangina
Herpangina can be caused by about 70 serotypes of enteroviruses. Most often these are Coxsackie B, Coxsackie A17 viruses and enterovirus 711.
Since the only carrier of enteroviruses is humans, you can become infected through contact with a sick person or with a virus carrier who has no symptoms of the disease1. According to the literature, the number of virus carriers can be up to 46% of people2.
The virus is released into the external environment with feces and droplets of saliva. It is also contained in bubbles that appear in the patient’s throat. Enterovirus infections most often affect children, although the disease also occurs in adults5.
The patient or virus carrier excretes viruses from the upper respiratory tract within 3 weeks after infection, and with feces - up to 8 weeks. In the first two weeks, herpetic sore throat is most contagious1.
You can become infected in the following ways:
- through dirty hands, objects and food if they are exposed to the virus;
- drinking contaminated water from a reservoir;
- upon contact with a patient or virus carrier.
The herpangina virus is also transmitted transplacentally - from mother to fetus3.
Up to contents
Features of glossitis during pregnancy
The causes of glossitis of the tongue in pregnant women are due to the fact that the immune defense weakens to allow the fetus to develop, which means that the body during this period becomes practically defenseless in the face of various bacteria and viruses. The second risk factor is a lack of vitamins and minerals obtained from food.
According to statistics, most often pregnant women experience a picture of desquamative and Gunter's glossitis. Symptoms that should alert you during pregnancy include:
- Profuse drooling. During the period of bearing a child, a woman already secretes a larger amount of saliva than usual, but a sharp increase may indicate the onset of glossitis.
- "Lacquered Tongue" A specific symptom that indicates the development of B12 deficiency anemia.
- Color change. White spots on the surface of the tongue alternate with spots of rich red color.
- Refusal of food. Acute glossitis in pregnant women is characterized by severe pain in the tongue during chewing and speaking, which, among other things, affects appetite.
As for the treatment of glossitis in pregnant women, the safety of the fetus comes first. Therefore, all therapy is exclusively local in nature (sprays, rinses), eliminating the penetration of the drug through the placenta. It is recommended to adjust your diet in such a way as to remove any foods that irritate your tongue.
Attention!
In order to avoid complications that can negatively affect the health of the fetus, treatment of glossitis during pregnancy must be carried out under the supervision of an obstetrician-gynecologist monitoring the woman.
Diagnosis and treatment
To diagnose glossitis in adults, the following basic methods are successfully used today.
- Examination
An experienced dentist in 95% of cases is able to diagnose glossitis based only on visual data. - RPR test
A special test that detects antibodies to the cardiolipin antigen. - Scraping
It is taken from the surface of the tongue to exclude syphilis, whose symptoms are similar to glossitis. - PCR
The most modern and accurate diagnostic method for identifying a wide range of infectious pathogens.
Treatment of glossitis depends on the form of the disease and analysis of concomitant diseases, but in any case it should be comprehensive:
- enhanced oral hygiene;
- general strengthening therapy aimed at increasing immunity;
- local treatment with antiseptics;
- strict diet;
- targeted medications (for example, for candidal glossitis - antifungal agents).
You can find out more about how to treat glossitis of the tongue in the article.
Sources
- Corsino CB, Ali R, Linklater DR. Herpangina. 2022 Jun 23. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan–. PMID: 29939569. https://www.ncbi.nlm.nih.gov/books/NBK507792/
- Ter-Baghdasaryan L.V., Ratnikova L.I., Stenko E.A. Clinical and epidemiological aspects of enterovirus infection // Infectious diseases: news, opinions, training. 2022. T. 9, No. 1. P. 88-93. doi: 10.33029/2305-3496-2020-9-1-88-93 https://infect-dis-journal.ru/ru/jarticles_infection/672.html?SSr=2601343bdb01ffffffff27c__07e4040b011a36-9772
- Alacheva Z. A., Rybalka O. B., Kulichenko T. V. Should everyone escape from Coxsackie?! Or fear has big eyes. Issues of modern pediatrics. 2017; 16 (4): 286–290. doi: 10.15690/vsp.v16i4.1774) https://vsp.spr-journal.ru/jour/article/viewFile/1787/713
- Herpangina Brenda L. Tesini. University of Rochester School of Medicine and Dentistry // MSD Handbook - 2019 https://www.msdmanuals.com/ru/professional/infectious-diseases/enteroviruses/herpangina
- Kozlovskaya O.V., Katanakhova L.L., Kamka N.N., Evseeva A.N. Epidemiological, clinical and diagnostic features of enterovirus infection in children and adults. Bulletin of Surgu State University. Medicine. 2018;(2):56-60. https://surgumed.elpub.ru/jour/article/view/140/141
- Kuo KC, Yeh YC, Huang YH, Chen IL, Lee CH. Understanding physician antibiotic prescribing behavior for children with enterovirus infection. PLoS One. 2022 Sep 7;13(9):e0202316. doi: 10.1371/journal.pone.0202316. PMID: 30192893; PMCID: PMC6128467. https://pubmed.ncbi.nlm.nih.gov/30192893/
- Instructions for use of the drug HEXORAL® SOLUTION:
- Instructions for use of the drug HEXORAL® AEROSOL:
- Instructions for use of the drug HEXORAL® TABS:
- Instructions for use of the drug HEXORAL® TABS EXTRA:
Up to contents
Is it worth treating glossitis with folk remedies?
If you have a question: how to cure glossitis, don’t waste time looking for folk remedies! If you notice characteristic symptoms that do not go away for more than a day, you need to seek help from a specialist. Treatment of glossitis should be carried out only by a dentist, who will determine the cause of the changes in the oral cavity, carry out all the necessary therapeutic and diagnostic procedures, prescribe a set of therapeutic measures that the patient can perform at home, and also monitor the entire treatment process, making changes to it as needed. necessary adjustments. Moscow dental clinics are presented in the “Search” section on our website.
Glossitis, like other periodontal diseases, is fraught with many complications, so treatment with folk remedies can only serve as an aid in complex therapy.
In order not to come face to face with glossitis, it is enough to brush your teeth regularly, including brushing your tongue, and do not skip preventive examinations at the dentist. In addition, doctors recommend avoiding excessive consumption of spicy foods and spices, limiting the intake of alcoholic beverages and smoking. Remember, disease is easier to prevent than to treat.