06/07/2018 I’ll start today’s article with what has already become a classic situation.
A person comes to see a doctor (dermatologist or oncologist) and shows him his moles.
And then something like this happens:
– You have dysplastic nevi here, here and here.
- What is this? Is it dangerous?!
– Dysplastic nevi are moles with an uneven edge and uneven color. Dysplastic nevi can develop into melanoma and must be removed.
- Oh!!! How scary!!! Let's delete it quickly!!!
The moles are safely removed and sent for histology.
A person comes home and starts reading on the Internet about dysplastic nevi. And then they add fuel to the fire:
- A dysplastic nevus is any nevus with an uneven edge and uneven coloration.
- All dysplastic nevi turn into melanoma in 146% of cases.
- To prevent death from melanoma, you need!!! URGENTLY!!! remove all dysplastic nevi.
All this “beauty” has been copied from one site to another for many years and fills the domestic segment of the Internet to the brim.
Let's understand all this from the point of view of evidence-based medicine.
How dangerous are dysplastic nevi?
There are specific, proven figures here that it would be better for those who spread hysteria on the “Internet” to become familiar with.
- The annual risk of a dysplastic nevus turning into melanoma is 1 in 10,000. According to the authors [4], this is very low.
- About 70% of melanomas develop not against the background of nevi, but against the background of unchanged skin [5].
- A study examining the genetic profile of atypical nevi has challenged the hypothesis that they are precursors to melanoma [6].
- In two studies, the authors followed patients with incompletely removed, histologically confirmed dysplastic nevi for a long time (up to 17 years) [8,9]. Based on this, the very thesis about the increased risk of developing melanoma from a dysplastic nevus can be seriously questioned.
- Gallery
- News
- Reviews
- Vacancies
- Licenses
- Insurance partners
- Controlling organizations
- Schedule for receiving citizens for personal requests
- What you need to know about coronavirus infection?
- Rules for patients
- Online consultation with a doctor
- Preparing for research
- to corporative clients
- Documentation
Dysplastic nevus is one of the types of flat pigmented skin formations, which are more often called moles.
Patients, and many doctors, mistakenly believe that all flat pigmented formations are benign and do not pay attention to them. However, it is known that dysplastic nevi can transform into melanoma. The transformation process occurs gradually as lentiginous melanocytic dysplasia (LMD) develops from grade 1 to grade 3.
This type of formation deserves the closest attention among all types, since there is a very high risk of their malignancy with transition to the most malignant tumor - melanoma. The term dysplastic itself means that it is a nevus that is not similar in external and internal characteristics to typical moles. Dysplastic nevus, which occurs in 5%-9% of the white population, has recently attracted the attention of researchers, as it may be a precursor to superficial spreading melanoma: it is found in almost all patients with hereditary melanoma and in 30–50% of patients with sporadic melanoma . A dysplastic nevus can occur on intact skin or be a component of a complex noncellular nevus.
Clinically, dysplastic nevus is similar to borderline nevus, but there are also differences. Thus, a dysplastic nevus is an irregularly shaped spot, while a borderline nevus has a regular shape - round or oval. The color of a dysplastic nevus is often heterogeneous, with areas of dark pigment, while a borderline nevus is characterized by a uniform color, the color of both nevi varies from light brown to dark brown. Often, a pinpoint formation resembling a target is noted in the center of a dysplastic nevus. When a dysplastic and mixed nevus is combined, there is a picture of a “fried egg” with a raised yolk in the center.
In our observations, dysplastic nevi were found in 5% - 10% of patients who consulted a surgeon or oncologist for various diseases. In some, the nevi were single - from 3 to 10 formations, in others - multiple - from 50 to 100 or more. Observing patients with multiple dysplastic nevi, we identified 2 types of these formations.
In the first type - there were fewer of these patients - dysplastic nevi appeared in childhood and adolescence, were often hereditary, but these patients did not report melanoma in relatives. Carriers of nevi were, as a rule, white-skinned, poorly tanned, with blond or red hair and light eyes. Dysplastic nevi of this type were large - 0.5 - 1.0 cm in diameter, located on open and closed areas of the body (buttocks, lower abdomen), and were often combined with papillomatous nevi. The color of nevi in the same patient could vary from pink to dark brown, sometimes a variegated color was observed: dark areas on a pink or light brown background. This pattern of nevi has been described as “dysplastic nevus syndrome.” After puberty, new nevi did not appear in this group of patients. This fact can be attributed to the fact that white-skinned people limited their exposure to the sun, as they quickly burned, and were also informed about the possible appearance of new “moles” as a result of exposure to ultraviolet radiation.
In the second type, dysplastic nevi were rare in adolescence; most nevi appeared in adulthood and were associated with frequent and prolonged exposure to the sun while vacationing in southern latitudes. Dysplastic nevi of this type were small - from 0.1 to 0.4 cm in diameter, regular rounded in shape, uniform in color, combined with multiple freckles in young patients and pigment spots of the “Dubreuil’s melanosis” type in older patients. In white-skinned patients with skin phototype 1 - 2, the nevi were light brown, in others they were brown or dark brown. The density of nevi was higher on sun-exposed areas of the body: the face, forearms, outer surface of the shoulders, upper half of the back and chest wall (like a “wide neckline”). All this indicates some similarity between dysplastic nevi of the second type and Dubreuil’s melanosis, which is a proliferation of melanocytes in the basal layer of the epidermis in individuals with skin phototype 1 - 2 under the influence of repeated sunburn.
According to our observations, the most important sign of progression of dysplastic nevus is:
- The appearance of pigment formation on unchanged skin and its further growth over several months or years in persons over 18 years of age , i.e. in adulthood.
- Changes in the last 3-5 years of a long-existing nevus may indicate the progression of a dysplastic nevus, which is combined with a borderline or mixed nevus.
- An important sign of a progressive dysplastic nevus is a very dark color (almost black), or uneven coloration of the formation with areas of dark brown or black.
- The irregular shape of the nevus may be little noticeable with a small size of the progressive dysplastic nevus , at the same time it can also be observed in a long-existing noncellular nevus - borderline or mixed.
Excision of dysplastic nevus
Excision of the nevus (excisional biopsy) should be performed under local anesthesia, 0.4–1.0 cm from the visible boundaries, with subcutaneous tissue. Histological examination of a removed nevus should be carried out by a pathologist with experience in the study of melanocytic formations. Progressive dysplastic nevi require excision for prevention purposes, as well as early diagnosis of cutaneous melanoma . When melanoma is detected, the question of the need for reoperation - excision of the postoperative scar - is decided depending on the thickness of the tumor, determined by histological examination. According to foreign authors, as well as WHO recommendations, an adequate deviation from the boundaries of the formation for in-situ melanoma is 0.2 - 0.5 cm, for invasive melanoma with a thickness of less than 1.5 mm - 1.0 cm.
During removals carried out in the department of surgery from June 2009 to April 2014, of all removed pigmented formations, the clinical diagnosis of “dysplastic nevus” was confirmed morphologically in 76% of cases, i.e. Histological examination of these formations revealed structures of lentiginous melanocytic dysplasia (LMD). In 2.4% of cases, melanoma was detected that developed against the background of LMD ; in other cases, other types of nevi were confirmed (intradermal, mixed nevus, nevus of the sebaceous glands). In our clinical cases, patients with diagnosed melanoma did not require reoperation.
Foreign authors recommend removing dysplastic nevi 0.6 cm or more; according to our research, smaller nevi - 0.4 - 0.5 cm in diameter - can also be removed. In our practice, melanoma in one case measured 0.5 x 0.4 cm, in another - 0.5 cm.
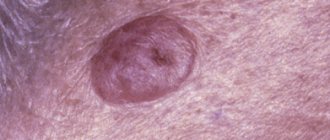
Photos 1 and 2 show dysplastic nevi with signs of progression.
Photo 1 shows a nevus of the gluteal region measuring 0.5 x 0.4 cm in a 29-year-old patient with skin phototype 1. The nevus, according to the patient, appeared 7 months ago in the form of a punctate formation, which gradually increased (a sign of progression) . No other pigmented nevi or freckles were found on the body. Histological examination: lentiginous pigmented nevus with severe (grade 3) melanocytic lentiginous dysplasia.
Photo 2 shows a nevus of the chest wall in a 27-year-old patient , 0.3 cm in diameter, round in shape, which darkened after staying in the south (a sign of progression) . Histological examination - mixed dysplastic pigmented nevus with severe (grade 3) melanocytic lentiginous dysplasia.
If the patient refuses surgery or in the absence of obvious signs of progression of the dysplastic nevus, the nevus should be re-examined by a doctor after 6 months. If there are changes in the nevus over the past period, surgery is recommended; if there are no changes, further observation after 6 months.
Patients with dysplastic nevi need:
- avoid prolonged exposure to direct sunlight,
- protect the skin with clothing,
- apply sunscreen.
The material was prepared based on the article: “Tactics for managing a patient with a dysplastic nevus” - O.A. Romanova, N.G. Artemyeva, E.A. Yagubova, I.M. Rudakova, V.N. Marycheva, A.A. Veshchevaylov . Clinical dermatology and venereology No. 2, 2015.
Services and prices
Histological examination of skin biopsy material
1,650 rub.
Appointment with a dermatovenerologist, therapeutic and diagnostic, primary, outpatient
2,000 rub.
Appointment with a dermatovenerologist, therapeutic and diagnostic, repeat, outpatient
1,800 rub.
Appointment with an oncologist, treatment and diagnostic, primary, outpatient
2,000 rub.
Appointment with an oncologist, therapeutic and diagnostic, repeated, outpatient
1,800 rub.
Appointment with a surgeon LD, PERV, AMB
2,000 rub.
Appointment with a surgeon, candidate of medical sciences, primary, outpatient
2,500 rub.
Removal of benign formations with a diameter of up to 5 mm using the molecular resonance surgical device VESALIUS LX 80 (with anesthesia and bandage)
2,500 rub.
Removal of a benign tumor with a diameter of more than 5 mm using a molecular resonance surgical device VESALIUS LX 80 (with anesthesia and bandage)
3,100 rub.
Isaeva Galina Ivanovna Oncologist Work experience: 19 years
Romanova Olga Aleksandrovna Oncologist (mammologist) Work experience: 62 years
Artemyeva Nadezhda Georgievna Head of department, surgeon, phlebologist Doctor of the highest category Work experience: 43 years
Bezlepko Marina Gennadievna Oncologist Work experience: 13 years
Make an appointment
What to do? Should I delete or not?
Fortunately, I was not able to find practical recommendations in which the mere presence of an atypical nevus on a person’s skin would be considered a direct indication for its removal.
On the other hand, the presence of single or multiple, atypical [7] and dysplastic [3] nevi on a person’s skin equally increases the risk of developing melanoma on the skin as a whole.
Thus, in my opinion, the most logical tactic seems to be not prophylactic removal of atypical nevi, but increasing the frequency of preventive self-examinations and examinations by an oncologist.
Is it time to sound the alarm?
Moles, or, in scientific terms, nevi, are present on the body of every person. It is believed that the bulk of them, up to 90%, appear by the age of 25. But they can also arise later - under the influence of various events. For example, a typical phenomenon is when they literally break out during pregnancy. Sometimes moles, on the contrary, disappear over time. They can be yellow, brown, black. This is all within normal limits and there is nothing to worry about.
But it happens that a mole begins to grow unevenly or changes color, its surface becomes “polished” or it begins to bleed - that is, changes occur in it. Another option is the appearance of a new mole of an unusual appearance. It is precisely such incomprehensible neoplasms that require close attention.
After the procedure
After removing a nevus, it is extremely important to protect the skin from ultraviolet radiation. You can’t sunbathe in a solarium; you should be in the sun as little as possible. It is recommended to refrain from thermal procedures. It is impossible to remove crusts at the site of the surgical wound; the skin should be provided with maximum rest. After removing a mole on the face, it is not advisable to use decorative cosmetics.
You can learn more about the diagnosis of skin tumors and methods of their treatment at a consultation with a dermatologist at the Galaktika clinic (Moscow).
Diagnostics
There are a number of signs of malignant degeneration of a mole:
- in the area of the mole there are signs of a violation of the skin pattern, peeling;
- the color of the mole changes from black to pale pink;
- uneven coloring of the mole;
- the formation of an inflammatory corolla around the mole;
- changing boundaries;
- increase in size, thickening of the mole;
- vertical or horizontal growth.
The appearance at the base of a mole of nodes with areas of decay, cracks, ulcers, bleeding, the presence of itching, burning, tingling should also be alarming.
The first signs of melanoma are an increase in the size of the mole. Discoloration, bleeding, ulceration and pain appear much later.
Diagnosis also consists of a thorough examination of the skin, including the armpits, scalp, interdigital folds, genitals, perianal area and oral mucosa, as well as palpation by the doctor of the lymph nodes and liver.
For unambiguous confirmation, an ultrasound examination (to determine the thickness and depth of invasion), ultrasound of the lymph nodes and abdominal organs, chest x-ray, biopsy and computed tomography (if metastases are suspected) are performed. A biopsy is indicated in some cases - when the thickness of the tumor is from 1 to 4 mm and if the entire range of diagnostic measures did not make it possible to verify the diagnosis.
Signs of metastasis in the final stages
Melanoma metastases usually occur in the following cases:
- if the patient is elderly;
- with complications of melanoma by chronic diseases;
- when melanoma cells grow into the walls of other organs;
- with a large size of primary melanoma.
Signs of liver metastases
When metastases are localized in the liver structures, black melanin accumulations form in them, representing the affected areas. In this case, functional or physical disorders occur in the liver, the consequences of which are felt by the entire body.
The main signs that melanoma has metastasized to the liver are:
- tuberosity of the organ;
- increase in liver size;
- sudden weight loss;
- presence of jaundice or ascites;
- pain in the right hypochondrium;
- nausea and vomiting;
- enlarged spleen;
- frequent nosebleeds.
Metastases in the lungs
The initial phase of pulmonary metastases does not have pronounced symptoms. In this case, there will be general signs of cancer problems in the body such as apathy, anemia, weakness, weight loss, decreased appetite, hyperthermia. Signs of metastases may initially include various colds - bronchitis, flu, pneumonia. Sometimes symptoms of lung metastases in melanoma occur only at the final stage of the disease, when nothing can be done to alleviate the patient’s condition. In this case, multiple nodular formations with involvement of the pleura and bronchi are diagnosed in the lungs.
If a large part of the lung is affected or the bronchi are compressed due to metastases, the patient experiences shortness of breath. The cough with metastases is predominantly nocturnal and dry, then gives way to ulcerations of mucopurulent sputum, odorless, but often with traces of blood. As metastases grow, the bronchi narrow and the sputum thickens, becoming purulent. Pulmonary hemorrhage may occur.
Pulmonary metastases, which affect the pleura, spine and ribs, cause pain. If metastases reach the lymph nodes of the left part of the mediastinum, hoarseness and aphonia appear, and with right-sided damage to the lymph nodes, the upper part of the body may swell due to compression of the superior vena cava.
Metastases in lymph nodes
Metastases in melanoma most often occur at stages 2-3 of the disease. The most common site for metastasis is the lymph nodes. Moreover, if a patient has a single metastasis to a lymph node, then, according to doctors’ forecasts, he will live another 5 years in 51% of cases. With 4 metastases in this area, only 17% of patients will overcome the five-year mark.
Signs of lymph node metastasis in melanoma are:
- sudden loss of body weight;
- causeless enlargement of lymph nodes;
- visual impairment;
- constant fatigue and chronic feeling of tiredness.
Metastases in bones
Metastasis to the bones is considered a very common phenomenon in melanoma in medicine, which gives severe pain to patients. The main manifestations of this process can be hypercalcemia, bone fragility, neurological changes, and compression of the bone marrow. Metastases to the bone come from the primary site, but other tumors can also be the cause, such as soft tissue sarcoma, ovarian tumors, etc. Melanoma most often affects the bones of the pelvis, hips, vertebrae, and ribs. Metastases follow from melanoma to the bones of the skull along the venous vertebral plexuses.
Nature has protected the skull bones with the ability to constantly renew themselves through osteoclasts and osteoblasts, but the entry of melanoma cells through the bloodstream into the bone marrow destroys these structures. The result of this is constant fractures of the skeleton in different parts, even under small loads.
Metastasis in the brain
Melanoma causes metastases to the human brain more often than other cancer pathologies. After this, there is no need to wait for a complete cure of the disease. The chances of survival for a patient with such metastases are significantly reduced. However, sometimes modern therapy with monoclonal antibodies helps to stop this process if there are individual characteristics of the human body.
Metastases to the brain area occur in 45% of all patients suffering from late-stage melanoma. This ultimately leads to the death of the patient. The symptoms of such metastasis will depend on the location of the lesion, necessarily including incoordination of the patient’s own body, emotional instability, headaches, fever and fever, memory loss, personality changes, lethargy, changes in pupil size, general weakness and difficulty in speech skills.
If the metastases have affected the frontal part of the brain, then the patient may experience sudden changes in rudeness, he begins to swear, and experience disturbances in visual functions and the musculoskeletal system. The symptoms of such metastases are very individual and sometimes they can completely change the patient’s personality.
When the patient's brain stem metastasizes, bursting or dull intracranial pain occurs in the head, which leads to dizziness and impairs visual functions. Also, such metastasis causes constant nausea and vomiting in the patient, convulsions, which in manifestations resemble epileptic seizures.
How are black moles treated?
There are two treatment options - watchful waiting/observation of the patient by a dermatologist and removal/excision of the black mole.
In the first case, wait-and-see tactics are necessary when the chance of developing an atypical process is extremely low.
And the patient does not experience any discomfort from the mole, either emotional or physical.
Surgical removal is recommended when a black mole has a chance of degenerating into a malignant formation.
Or for aesthetic reasons, for example, when localized on the face, genitals, cheek.
The following removal methods can be used to remove a nevus:
- Surgical intervention. The tumor is completely removed. If during dermatological diagnosis it was revealed that the mole is accompanied by a malignant process, surgical intervention should consist of removing a certain edge of healthy tissue to prevent local recurrence.
- Cryosurgery. A procedure that uses a special instrument called a cryoprobe. The device is used to freeze and destroy abnormal tissue. The cryoprobe has a thin end that is cooled by substances such as liquid nitrogen and liquid nitrous oxide. Cryosurgery can be used to treat certain types of cancer and certain conditions that may progress to malignancy. This manipulation is also called cryoablation or cryotherapy. The technique can be used if there are black moles on the penis or in the perineal area.
- Radio wave excision. The procedure is based on the use of a special drug, most often “Surgitron”, which produces high-frequency radio waves. During the manipulation, the pathologically altered tissue is destroyed, while the surrounding epidermis is not injured. When removing moles, radio wave excision is often recommended. During the procedure, the vessel is blocked, so the risk of bleeding is almost zero. A black mole after this type of removal is not accompanied by the development of scar tissue, healing of the excision site occurs quickly.
- Laser removal. Excision of moles with a laser is considered the most effective method. The laser beam is able to penetrate deep into the epidermis, clearly along a given trajectory. This facilitates effective removal of the nevus without blood loss. The procedure is most often recommended for Ota phakomatosis. The procedure has proven itself in removing black moles on the lip and facial area.
Preparation for dermatoscopy of moles, disadvantages and advantages of the method
The analysis does not require special preparation from the patient, the study is absolutely painless.
The only relative disadvantage is that dermatoscopy subjectively evaluates the appearance of blackheads.
The result largely depends on the experience of the medical expert.
However, a modern dermatoscope with the ability to connect to a computer allows you to share the results with other doctors.
This increases the likelihood of correct diagnosis and accurate diagnosis.
Special computer programs are being developed that should facilitate the differentiation of benign and dangerous lesions of the epidermis.
Dermatoscopy is a simple, non-invasive and widely available diagnostic method.
Does not expose the patient to harmful radiation and provides valuable information for the evaluation of skin lesions of unknown origin.
However, the most informative method for diagnosing moles/nevi remains histopathology (histology).
Histopathological examination represents the gold standard for diagnosis in dermatology.
Dermatoscopy is an additional tool that allows you to assess the condition of the epidermis.
It should be taken into account that the effectiveness and information content of this method also depends on the specialist - the diagnostic accuracy of dermatoscopy correlates with the doctor’s experience.