Basal cell carcinoma (basal cell carcinoma) is the most common type of skin cancer. It grows from epidermal cells called keratinocytes, which are located near the basal layer of the dermis. The tumor grows extremely slowly and practically does not metastasize, which is why it is called semi-malignant. However, basal cell carcinoma is characterized by infiltrative growth, so it can penetrate into the underlying tissue. With severe destruction and persistent relapses, basal cell skin cancer metastasizes and can lead to the death of the patient.
- Causes of malignant skin tumors
- Types of basal cell skin cancer
- Skin Cancer Symptoms
- Methods for diagnosing basal cell tumors of the skin
- Treatment options for basal cell skin cancer
- Possibility of recurrence of basal cell carcinoma
- Prognosis and prevention of basal cell carcinoma
- Related operations and techniques
Typically, basal cell carcinoma occurs in people with fair skin on areas of the body exposed to sunlight (face and hands).
In the head and face area, basalioma is usually localized in natural folds:
- Wings of the nose.
- Nasolabial folds.
- Lips and corners of the mouth.
- Corners of the eyes.
Causes of malignant skin tumors
The development of basal cell carcinoma can be triggered by the following factors:
- Exposure to ultraviolet radiation - tanning under the influence of solar radiation or a solarium.
- Exposure to ionizing radiation - a history of radiation therapy courses, work with open sources of radiation, etc.
- Immunodeficiencies, both primary and secondary.
- Chronic traumatic injury to the skin, such as chafing from uncomfortable clothing.
- Exposure to carcinogenic factors of a chemical nature - work in hazardous production conditions, contact with household chemicals.
In addition, there is a genetic predisposition - basal cell nevus syndrome or Gorlin syndrome. It is characterized by the formation of multiple foci of basal cell carcinoma in young people in combination with endocrine pathology, mental disorders and skeletal lesions.
At the moment, there are two most common forms: superficial and nodular
Superficial (newly identified) BCC:
- most often develops on the skin of the trunk and limbs;
- less common: head and neck;
- in younger patients, with a predominance of women.
Important!
The main development factor is genetic - this is a hereditary mutation that is transmitted to descendants or arises in connection with environmental or other adverse effects of the external environment. Nodular form (first identified) of BCC:
- most often develops on the scalp
- in elderly and senile patients
Types of basal cell skin cancer
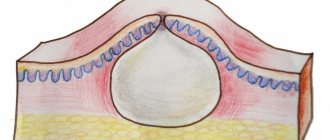
- Nodular-ulcerative form of skin cancer. The onset of the disease is characterized by the appearance of dense areas on the skin that have clear boundaries (nodules). New growths may have a gray, pinkish or yellowish color. Gradually, the skin over them becomes thin and acquires a pearlescent hue. The nodules merge with each other and form a plaque with a depression inside. Over time, an ulcer covered with a crust forms in the center of this plaque. It spreads to the sides and deep into the plaque, as a result the latter becomes like a crater. The bottom of the ulcer is uneven, covered with scabs and crusts, the edges are very dense, almost like cartilage tissue. The process lasts several months. If basalioma is not removed, it will grow into the underlying tissue, affecting the subcutaneous tissue, muscles and even bones.
- Large nodular basalioma develops from a single node. It gradually increases in size and becomes rounded. Its diameter can exceed 3 cm. The surface of the node is usually smooth, but can be covered with scales. The color of the tumor may not differ from healthy skin, but may acquire a pinkish tint. An ulcer forms in the center of the node, from which ichor oozes.
- The perforating form of skin cancer is characterized by initially infiltrative growth. The tumor grows inside the tissue, has no clear boundaries, and over time an ulcer appears on its surface.
- The warty form of cancer looks like papillomas with keratinizations tightly adjacent to them.
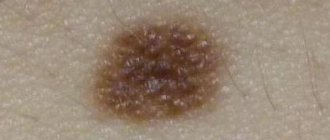
- The superficial form of basal cell carcinoma begins with the formation of a pale pink spot. At first it does not exceed 5 mm, then it begins to peel off and acquire clear contours. After some time, its edges thicken and nodules form on them, which then merge into a roller. The center of the formation sinks and becomes dark pink or brown. The tumor gradually increases in size and can sometimes grow into the underlying tissue.
- The scleroderma-like form of basal cell skin cancer begins with the formation of an inconspicuous yellowish-whitish plaque. Periodically, erosions form along its edges, covered with a thin crust. These crusts are easily separated, revealing a reddish inflammation underneath. Gradually, cysts form in the tumor, in which crystals of calcium salts can be found.
- The fibrous form of skin basalioma begins with the formation of a dense nodule, which gradually grows, flattens and turns into a plaque. Blood vessels are visible through the layer of epidermis.
- Cylinderoma, or turban skin tumor, is most often localized on the scalp. It consists of hemispherical nodes of a violet-red color; spider veins can be visible in them. The size of one node in diameter can reach 10 cm. Usually there are several such nodes.
During a general examination of the patient, an oncodermatologist
EVERYONE is watching! Skin on the torso, face, neck, limbs, mucous membranes, scalp.
- Dermatoscope.
- SIAscopically.
- Cytologically.
- Histologically!!
Biopsy of a skin tumor
A mandatory diagnostic step for skin tumors is morphological verification of the process; for this, a biopsy
. The oncologist takes cells or tissues from the site of the tumor and submits them for examination to pathologists, who form their conclusion.
The morphological report contains information about the tumor:
- localization of the process (where the tumor is located);
- diameter (what size is the tumor);
- growth type;
- characteristics of the resection margin (the tumor was completely removed or not).
The oncologist makes a final diagnosis and forms a treatment plan only after receiving the results of the biopsy.
Skin Cancer Symptoms
Symptoms of basal cell carcinoma are extremely variable and depend on the form of the disease. The tumor manifests itself with the following manifestations:
- Shiny pink nodules with visible blood vessels.
- Papules or nodules covered with ulcers.
- Plaques. Dense, scar-like.
- Psoriasis-like plaques.
Stages of basal cell skin tumor:
- Stage 1 - the tumor is no more than 2 cm in greatest dimension.
- Stage 2 - the size of the tumor exceeds 2 cm, but there is no germination (invasion) into the underlying tissue.
- Stage 3 - Skin cancer has grown into underlying structures, such as muscles or bones. Or a less invasive tumor, but with regional metastases.
- Stage 4 - the tumor gives distant metastases.
Methods for diagnosing basal cell tumors of the skin
Diagnosis of basal cell carcinoma involves a thorough examination of the skin. The Photofinder digital dermoscopic system allows you to perform a more detailed examination. Its effectiveness is tens of times greater than that of standard dermatoscopy, since it records all nevi and skin tumors larger than 0.9 mm and allows you to monitor the dynamics of their changes.
To confirm the diagnosis, a laboratory histological examination of a piece of tumor tissue is performed. This piece is obtained in one of the following ways:
- Incisional biopsy. Using a scalpel, a small marginal fragment of the neoplasm is excised within visually unchanged skin. This method is indicated for large tumor sizes.
- Excisional biopsy. The entire tumor is excised within healthy tissue. The resulting wound is sutured with cosmetic sutures. Such a study is possible for tumor sizes up to 1 cm on the body and limbs and less than 0.5 cm on the face.
A biopsy is not always possible, especially if the skin cancer is located on the face. In this case, a cytological examination of scrapings or impression smears from the tumor is indicated. If the surface of the tumor is not changed, a puncture is performed with aspiration of the tumor tissue.
Additional diagnostic methods are used to examine lymph nodes for the presence of metastases. For this purpose, ultrasound, CT or MRI is used. If there is a suspicion of damage to the lymph nodes, they are punctured and the resulting material is subjected to microscopic examination.
Diagnostics
Diagnosis of malignant skin tumors is in most cases simple. The examination of the patient should begin with a history and medical examination, with special attention paid to a complete examination of the skin and regional lymph nodes.
The main diagnostic measures to confirm skin cancer include:
- Dermatoscopy is a visual assessment of the tumor, zoomed in using special magnifying glasses;
- Thermography - measuring the temperature of a tumor;
- A smear is an imprint. A method in which a glass slide is applied to a crusted ulcer with gentle pressure. Several pieces of glass and different areas of the suspected tumor are used. The collected prints are then examined using microscopy;
- Scraping Using a special wooden spatula, scrape off a certain amount of content from the bottom of the ulcerated surface and transfer the material to a glass slide for subsequent study;
- Biopsy. In the puncture form, using a needle and syringe, cellular material is taken from the depth of the formation. In the excision option, which is possible when the size of the formation is tiny, it is excised within tissues not affected by the process, followed by examination of the removed area. With the incisional option, a large tumor is removed in a wedge shape, capturing healthy tissue structures;
- Imaging methods necessary to clarify and verify the spread of the oncological process. These include: ultrasound screening, computed tomography examination.
Treatment options for basal cell skin cancer
The choice of treatment options for basal cell carcinoma is determined by the location of the tumor and the stage of the disease. Preference is given to surgical removal methods. If their use is impossible, radiation therapy is performed. Additional treatment methods can also be used, for example, cryodestruction, local chemotherapy, etc.
Surgery
Surgical treatment is more preferable because it allows you to control the radicality of the operation by examining the cutting edges for the presence of malignant cells.
- The classic method is excision of the tumor with a scalpel within healthy tissue. The wound is closed with cosmetic stitches, and the tumor is sent to the laboratory. If there are no tumor cells at the cutting edges, it is considered that the tumor has been radically removed and no other treatment methods are required. Surgical excision cannot be performed when basal cell carcinoma is localized in the folds of the face, since a pronounced defect will remain.
- The second option for the operation is curettage followed by electrocoagulation. First, the basal cell carcinoma is removed using a curette (a surgical instrument with a tip in the form of a ring with a sharp edge). Then the wound is cauterized with an electrocoagulator. If there is a high risk of relapse, the procedure is repeated to destroy any malignant cells remaining in the wound. A whitish scar remains at the site of removal.
Radiation therapy for cancer
Radiation therapy gives fairly good results in the treatment of basal cell carcinoma. Its effectiveness reaches 90%. Treatment is carried out in courses over several weeks. Sometimes the protocol involves daily radiation therapy sessions.
Indications:
- Senile age of the patient.
- High risks of surgical intervention.
- Impossibility of surgery due to the “inconvenient” location of the tumor - nose, ears, eyelids.
- The patient's serious condition.
- As part of combined treatment for high risks of relapse after surgical excision.
Chemotherapy
Treatment of superficial forms of cancer is possible with the help of local chemotherapy drugs. For this, an ointment based on 5-fluorouracil or other cytostatics is used. If regional metastases are present, they are surgically removed. As a rule, the operation involves excision of subcutaneous fat in a volume corresponding to the nature of the lesion.
Other methods
In addition, alternative methods of treating basal cell carcinoma are used, which provide good clinical and aesthetic results. Photodynamic therapy is most effective in this regard. It is performed as follows: a special drug is applied to the surface of the basal cell carcinoma - a photosensitizer, which accumulates in malignant cells in increased quantities. After this, the tumor is exposed to laser radiation of a given wavelength. This leads to the activation of the photosensitizer and the launch of a cascade of chemical reactions that destroy tumor cells. Immediately after irradiation, swelling develops at the site of exposure, and within 24 hours the tissue begins to become necrotic.
After a few days, a dense scab forms at the site of the tumor, fused to the underlying tissues. As it heals, the scab falls off and an epithelialized wound remains in its place. In general, the cosmetic result is satisfactory. Photodynamic therapy in our clinic is used to treat superficial forms of basal cell cancer located in the face and hands.
Other alternative treatments are less effective, but may be used under certain conditions:
- Cryodestruction is the destruction of a tumor using low temperatures. The cooling agent is applied to the skin by application or applied using an aerosol. This method is rarely used because it gives worse treatment results. However, its use may be justified in patients suffering from bleeding disorders (propensity to bleed).
- Laser surgery has not received official approval for the treatment of cutaneous basal cell carcinoma, so it is used in cases where other methods have exhausted their possibilities. The essence of the treatment is layer-by-layer evaporation of the tumor using heating under the influence of laser radiation.
Combination treatment of basal cell carcinoma
Combined treatment is carried out for large invasive tumors that cannot be removed to the required extent, as well as in the presence of metastases. Surgical excision of the tumor is used, followed by irradiation of its location (for locally advanced cancers), or surgery followed by systemic chemotherapy.
Systemic drug treatment for disseminated forms of basal cell carcinoma
Invasive and metastatic forms of basal cell carcinoma require systemic therapy. Targeted drugs are indicated that block the molecular processes that ensure the functioning of the tumor.
In 85% of basal cell carcinoma cases, there are mutations in genes encoding proteins of the Hedgehog signaling cascade, which is of great importance during embryonic development. In particular, it affects the specialization of cells in the process of organ formation. In adults, its work is very limited.
Normally, the signaling pathway is triggered by the action of the Sonic Hedgehog SHH protein, which is named after the video game character Sonic the Hedgehog (in a study on fruit flies, turning off SHH resulted in the embryos becoming like spiky balls). But with basalioma, the process began without it, with the help of another protein called SMO.
The drug Vismodegib suppresses the action of SMO, thereby blocking the entire uncontrolled Hedgehog cascade. This therapy is indicated for locally advanced and metastatic forms of basal cell carcinoma, as well as in cases where other forms of treatment (surgery or radiation therapy) are impossible or impractical.
INTRODUCTION
Papillomatosis and warty lesions affecting the skin were described in Ancient Greece. Research into papillomavirus (PV) began at the beginning of the twentieth century. In 1933, VP was isolated as a possible etiological agent of warts in rabbits. Since then, this class of viruses has been considered as a natural viral infectious agent responsible for the development of warts in various groups of mammals, including humans.
In 1935, Rous described warts in rabbits as having the potential for malignant transformation. Straus et al. reported the first visualization of HPV particles in human warts using electron microscopy in 1949. In 1950, the carcinogenic potential of human papillomavirus (HPV) was discovered in patients with epidermodysplasia verruciformis. The structure of the viral genome was only discovered in 1963 by Crawford and Crawford. However, in subsequent years, research into HPV has slowed due to the lack of tissue culture systems and the apparently benign nature of human warts.
In the 1970s, interest in these viruses gradually began to resume. At that time, researchers described the diversity of this class of viruses, and Zur Hausen proposed the hypothesis of the involvement of HPV in the etiology of cervical cancer.
The early 1980s saw rapid growth in HPV research; HPV types 16 and 18 were identified and their connection with cervical cancer was established. The first epidemiological study on HPV and cervical cancer was published in 1987. Since then, several epidemiological and molecular studies have confirmed that infection of the cervix with certain types of HPV is a precancerous condition of the cervix.
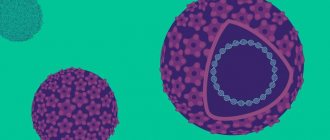
CHARACTERISTICS OF VIRUSES
HPVs are small DNA viruses (50-55 nm) belonging to the Papovaviridae family, a genus of papilloma. These are viruses with icosahedral symmetry and a true genome of about 8000 base pairs (8Kb) with double-stranded, circular DNA. Despite their small size, the molecular biology of these viruses is quite complex. Viral DNA is associated with histone-like proteins wrapped in 72 capsomeres, consisting of two structural proteins L1 and L2. These viruses can infect humans and a wide range of animal species (cats, rabbits and primates). Humans are the most widely studied host.
HPV is highly species specific and there are no reports of the species causing productive infection in another species. These are viruses that exhibit tropism for epithelial cells, causing infections of the skin and mucous membranes (genitals, mouth, larynx, esophagus), and their replication occurs in the nucleus of squamous epithelial cells.
Their viral genome consists of 3 functionally differentiated regions based on their location and functional properties: E (early) and L (late) and the third region is called LCR (long control region). The LCR region controls transcription of the viral genome, E initiates the functioning of early genes (E1-E8), expressing proteins responsible for viral genome replication (E1 and E2), DNA transcription (E2), maturation and release of viral particles (E4), cell transformation (E5, E6, E7), and immortalization (E6 and E7). The L region of the HPV genome consists of the L1 and L2 regions of the genomic sequences that determine the structural proteins of the HPV capsid. Its product, L1 protein, represents 80% of the viral capsid proteins, being the most abundant protein with high immunogenicity. Protein L2, together with L1, promotes the incorporation of viral DNA into the virion. Oncoproteins are proteins E6 and E7, which have an inhibitory effect on the functioning of the interleukin-18 gene, one of the dominant factors in the formation of immunoreactivity of CD8+ lymphocytes. The expression of major histocompatibility complex genes is reduced. E5, associated with IL-18, prevents the induction of γ-interferon. These proteins stimulate cell proliferation by interacting with and inhibiting the functions of the cellular proteins p53 and NRP, which are involved in the control of cell proliferation. Only high-risk HPV E6/E7 proteins can immortalize primary human keratinocytes, but not similar low-risk HPV proteins. The above-mentioned structural and functional features of HPV cause insufficient effectiveness of immune reactions to block the developing infection. The HPV life cycle is directly related to the cellular differentiation program of the host cell. The virus infects epithelial basal cells that have the potential to differentiate. Plant viral functions, DNA and capsid protein synthesis, and the assembly of new viruses occur exclusively in differentiated keratinocytes.
HPV appears to remain in host cells for a long period of life. Many different parts of HPV can be found in random areas of normal skin in humans and animals. This confirms that life cycle latency is a characteristic of these viruses.
Phylogenetics
HPVs are classified into several types by comparing the nucleotide sequence of their viral genome.
HPVs are grouped into different genera, which are in turn divided into different types, containing one or more genotypes. Each genotype is grouped into subtypes and variants based on sequence similarity in the L1 region.
To date, approximately 100 different types of HPV have been fully identified. In addition to all of these HPVs that have been fully sequenced, there are a large number of additional types for which genetic sequences have not yet been obtained using conventional methods.
Different types of virus within the same genus have approximately 60% - 70% similarity. A new type of HPV is considered a virus with changes in the genome of more than 10% in the L1, E6 and E7 genes compared to any known type of HPV. Differences of 2-10% represent new subtypes, and varieties with differences of up to 2% are variant types.
HPVs are grouped into the following genera: alpha, beta, gamma, mu and nu papillomas. Other genera include types isolated from mammals and birds. Phylogenetic grouping sometimes reflects biological and pathological traits, but there are often differences. For example, different types and species of the same genus can display completely different characteristics and still belong to the same genus.
Alpha papillomas (superseries)
These HPVs with tropism for the reproductive epithelium are part of this group. However, some species belonging to this genus cause common warts. This genus includes HPV types that pose a high risk of developing cervical cancer, such as HPV 16 and 18, respectively, classified as species 9 and 7 of this genus, as well as low-risk HPV types, such as HPV 6 and 11, both in species 10. At the same time, the same genus includes non-mucosal types of HPV, for example, HPV 7 - associated with skin warts in butchers and meat, poultry and fish processors, HPV 2, 27 and 57, 3 and 10 cause common warts on the skin.
Beta papillomas (superseries B - subgroup B1)
They are divided into five different types. HPV 5 and 8 are most often found in the skin of people with epidermodysplasia verruciformis. This genus also includes cutaneous HPVs found in the skin of the general population without skin lesions, demonstrating the ubiquity and high frequency of asymptomatic infection.
Gamma papillomas (superseries B - subgroup B2)
They cover five different species with seven different types that cause skin lesions:. HPV 4, 48, 50, 60, 88, 65 and 95.
Mu papillomas (superseries E)
These include HPV 1 and 63. HPV 1 is the most studied member of this group and causes common and plantar warts.
Nu papillomas (superseries E)
They have only one type:. HPV 41.
CLASSIFICATION
Historically, HPVs have been grouped based on their tissue tropism for certain types of epithelium and depending on the location where they were first isolated. Based on these characteristics, there are three main groups of HPV: cutaneous, mucosal, and epidermodysplasia-associated. Mucosal HPVs are classified into low and high severity according to their oncogenic potential.
All types of HPV have an affinity for stratified squamous epithelial cells, but there are differences in terms of affinity for different anatomical sites. For example, HPV-1 has a high replication rate in keratinized areas of the epithelium of the palmar and plantar localizations. HPV type 16 is a mucosal HPV with a preference for the genital area, and HPV 11 also affects mucous membranes with replication in the larynx and genital epithelium.
This classification is not entirely correct, because genital types of HPV can be found in the skin and the opposite is also possible.
HPV DETECTION METHODS
HPV does not grow on conventional nutrient media and serological diagnostic methods are not accurate enough. Diagnosis of HPV infection is made histopathologically, or by detection of viral DNA in infected cells.
Hybridization and polymerase chain reaction (PCR) methods used to detect HPV.
Among the hybridization methods used are the following:
1) Southern blot has high specificity and sensitivity. Allows you to estimate the amount of DNA in the lesion. It has some limitations due to the wide variety of HPV types and the inability to detect DNA with unknown viral sequences.
2) Dot blot and reverse blot are labor-intensive methods that present equal sensitivity and high specificity.
3) Labeled probes make it possible to determine the localization of viral DNA in cells and tissues. Although the sensitivity of this method is limited, it is the best way to assess the distribution of HPV in lesions, and it allows viral localization to be determined using other markers.
4) Non-radioactive hybrid capture: This method is safe, easy to perform and reproduce. It has high specificity for mucosal lesions.
Polymerase chain reaction (PCR) is the most sensitive method. It is indispensable in cases where the amount of DNA is small.
Skin warts
Warts are the most common and characteristic clinical manifestation of HPV infection. These are virus-induced pleomorphic tumors that can occur in various areas, in particular the skin of the extremities, mucous membranes, the skin of the genitals and larynx, and the mucous membranes of the oral cavity.
Epidemiology, transmission and pathogenesis
HPV is a virus distributed throughout the world. Viral warts are a very common viral infection with an incidence of 7-10% in the European population and 1% in the US population. These numbers increase 50 to 100 times in immunocompromised individuals, such as kidney transplant recipients, reaching more than 90% 15 years after transplant. Warts can occur at any age and the incidence increases during school age, with a peak in adolescence.
HPV is transmitted through direct or indirect contact from a person who has the lesion. Infection is facilitated by disruption of the epithelial barrier in the form of trauma, minor trauma, or maceration. The incubation period ranges from 3 weeks to 8 months. In most cases, spontaneous regression is observed.
Cellular immunity plays an important role. A high prevalence of warts and extensive and persistent manifestations are observed in immunocompromised patients, such as kidney transplant recipients, persons with HIV, and patients with epidermodysplasia.
The HPV life cycle is directly related to the cellular differentiation program of the host cell. Infection begins when HPV reaches a cell in the basal layer; For some time, there is no viral replication at this site, and the virus simply maintains its genome by amplifying a low copy number. The replication phase and protein synthesis occurs in suprabasal differentiating keratinocytes. The time of progression and type of lesion correlate with the number of detectable viral particles. Small warts contain a higher number of viruses compared to older warts. Plantar warts have a higher viral load than common warts. The center of the lesion is the main part of the virus concentration.
In benign lesions, viral genome replication is extrachromosomal. In malignant neoplasms, viral DNA is integrated into the chromosomes of host cells and viral replication is absent. There is inactivation of the expression of the E2 protein, which acts as a negative regulator of the expression of the E6 and E7 oncogenes.
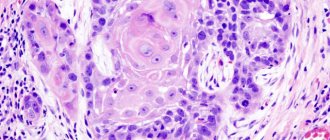
Histopathological characteristics of skin warts
The histopathological characteristics of viral warts are papillomatosis, hyperkeratosis with parakeratosis, hypergranulosis and acanthosis.
The most important characteristics that distinguish ordinary warts from other papillomas are: a) koilocytes (small vacuolated cells with a small round, highly basophilic nucleus and pale cytoplasm, located in the outer stratum corneum and granular layer); they represent a viral cytopathic effect, b) vertical rows of parakeratosis, and c) foci of keratohyaline granules. These three changes are characteristic of young or active common warts.
Some authors believe that certain histological features are specific to each HPV type and that histological examination may reveal different viral types. Other researchers disagree that different HPVs are characterized by different histological patterns that are characteristic of each type of virus. Most studies have not established any correlation between histology and HPV type.
1.1. Common warts
These are individual papules or nodules with a rough surface. Lesions can be one or several, of different sizes and, as a rule, proceed. Fusion of lesions can form large masses. They occur anywhere on the body, but are more common on the dorsum of the fingers. A common location in children is the knee.
Isolated warts may remain unchanged for months or years, or large numbers of new lesions may develop rapidly over a short period of time. The development of warts is unpredictable. Approximately 65% of warts disappear spontaneously within two years. Age and number of lesions do not affect the prognosis.
The types of HPV that cause common warts or warts vulgaris (VV) include: HPV 2, 27, 57 4, 1. HPV 7 is the most common type of wart in butchers and in fish and poultry handlers.
1.2. Plantar warts
Warts appearing on the soles. They may lie deep and this form is known as Myrmecia. They are usually painful and are caused by HPV 1. When they are more superficial, they form hyperkeratotic plaques called mosaic warts, which are less painful and are usually caused by HPV 2. HPV 4 is also found in plantar warts.
1.3. Flat warts
Flat warts are slightly raised, skin-colored or pigmented (brownish, slightly yellowish), with a flat, smooth or slightly rough surface. They are round or polygonal and their size ranges from 1 to 5 mm in diameter or more. The most common locations are the face and hands. Warts can be numerous and often have a linear arrangement corresponding to the site of skin injury (Koebner phenomenon). Spontaneous regression is common. The types of HPV most commonly found in flat warts are HPV 3 and HPV 10.
I.4. Filiform warts
They have a narrow stalk and grow perpendicular or inclined to the surface of the skin. Appear in the form of individual or multiple lesions, mainly on the face and neck. It is a morphological variation of the common wart with similar types of HPV, especially HPV 2.
I.5. Pigmented warts
Clinically, pigmented warts vary in color from gray to black-brown, and histopathologically, they present specific homogeneous cytoplasmic bodies - inclusions. The HPV types found in these lesions are HPV 4, 60, and 65.
Epidermodysplasia verruciformis (EB)
It is a rare, usually autosomal recessive, genetic disease where there is a honeycomb defect in the immune system and a high susceptibility to HPV-induced skin cancer. The link between HPV and cancer was first recognized in the 1950s among patients with EB. Patients with EB are highly predisposed to infection with a specific group of HPVs and to a high risk of developing cutaneous malignancies as a result of the oncogenic effects of HPV.
Skin lesions appear in early childhood and are polymorphic. They are no different from flat warts when present on the face and neck, and have the appearance of scaly hypo- or hyperpigmented erythematous spots, similar to lichen when localized on the trunk and limbs. Thicker, pink or purple plaques similar to seborrheic keratosis have also been described. Malignant transformations usually begin in the fourth and fifth decades of life and predominate in exposed areas, confirming the important role of ultraviolet radiation. Precancerous lesions such as actinic keratoses, malignant lesions such as Bowen's disease and invasive squamous cell carcinoma are observed. Basal cell carcinoma is rare in these patients.
The most common HPVs are 5, 8, 9, 12, 14, 15, 17, 19-25, 28, 29, 36, 38, 47, 49 and 50. HPV 5, then HPV 8 are the most common in malignant lesions, developed from BE. HPV 14, 17, 20 and 47 are less common in EB. With the development of technologies for HPV identification, these types of HPV began to be detected not only in patients diagnosed with EB, but also in normal skin and lesions, in immunodeficient and immunocompetent individuals, in patients with psoriasis and in patients with disorders of keratinocyte proliferation, such as autoimmune bullous diseases. diseases and burns.
Malignant skin lesions
3.1. Bowen's disease
Bowen disease (BD) is a squamous cell carcinoma that sometimes progresses to invasive cancer.
According to the literature, HPV, especially high-risk mucous types, are often found in extragenital BD, especially in periungual localization on the hands, less often on the feet. Detection of virus at these sites suggests autoinoculation from genital lesions.
The role of HPV is well known when BD is localized in the genital area, but is not fully understood in its extragenital forms.
With extragenital localization of BD, detection of HPV is not limited to the extremities (legs, arms, periungual areas). High-risk HPV is also found in extragenital lesions in the absence of genital lesions.
With extragenital localization, types such as HPV 2, low-risk mucosal HPV 6 and 11, HPV 54, 58, 61, 62, 73 are detected. HPV 58 is found in extragenital lesions located on the elbows, fingers and toes. For cervical cancer and vulvar carcinoma that developed at the site of BD, HPV 27, HPV 76, HPV-EV 20 and HPV-EV 23 are detected.
In 2005, Zheng et al. discovered in extragenital BD (EGBD) mucosal high-risk HPV types in 7% of 41 patients (HPV 16 and 33) and cutaneous HPV (HPV 27 and 76) in 5% of them. In lesions with high-risk HPV, the viral load was high and viral DNA in the cell nuclei of the stratum spinosum and part of the stratum basale in SCHD was easily detected using hybridization techniques. These results were not observed in EGD with cutaneous HPV types or in normal skin controls. Based on these results, the authors concluded that high-risk mucosal HPVs may play an important role in the pathogenesis of EGD.
3.2.Basal and squamous cell carcinomas
The precise role of HPV in the development of nonmelanoma skin cancers (NMSCs)—squamous cell carcinoma (SCC) and basal cell carcinoma (BCC)—has not yet been fully determined. There is growing evidence that HPV has significant potential in the process of cutaneous carcinogenesis.
The association between HPV and NMSC is observed in both immunocompetent and weakened patients. In the latter, positive detection of viral DNA in lesions is higher and the presence of various types of HPV in the same lesions is more frequent. More than 90% of kidney transplant recipients who had the transplant more than 15 years ago developed viral warts. 40% developed NMSC, a risk 50 to 100 times higher than in the general population. In this group of patients, in contrast to what is seen in the general population, the most common type of NMSC is RCC, with an approximate ratio of 3:1 to BCC, and the lesions tend to be numerous and more aggressive. Kidney recipients are more likely to develop RCC. Detection of HPV in these lesions is high, reaching 80-88%. A common feature is the discovery of new types of HPV-EV, as well as co-infection of the same type with involvement of more than one HPV type. In BCC, HPV detection is lower.
There are several studies of HPV and NMSC lesions in immunocompetent individuals. In these people, the prevalence of HPV is lower, 35% - 55% for RCC and 43.5% for BCC. In 2000, Harwood et al found the presence of HPV in 84.1% of RCC and 75% of BCC patients in immunocompromised kidney transplant patients, compared with 27.2% of RCC and 36.7% of BCC patients. immunocompetent patients. The predominant HPV type in both groups was HPV-EV. Cutaneous HPV types and infections of various HPV types were observed only in the immunocompromised group. There were no statistically significant differences between SCC and SCC regarding the HPV types present in the lesions.
In 2003, Iftner et al. conducted a case-control study to investigate the association between HPV and NMSC. HPV was detected in 59.7% of 72 RCC samples analyzed and in 27.8% of 18 BCC patients. HPV 4 and HPV 33 were the most common in NMSC. The authors noted that high-risk mucosal HPVs may represent a risk factor for NMSC in immunocompetent patients.
Forslund et al. in 2007 studied 349 immunocompetent patients with skin lesions: 82 with RCC, 126 with BCC, 49 with actinic keratosis and 92 with benign skin neoplasms. Paired normal skin biopsies from the same patient were also taken and PCR was performed to detect HPV DNA. Forty-two different types of HPV were identified and there was a strong association between HPV prevalence and sun exposure. HPV types 1 were more frequent in benign lesions, while HPV types 2 predominated in RCC. The authors conclude that HPV types of the beta-papilloma genus 2 are involved in the etiology of cutaneous SCC.
In 2008, Askari et al conducted a case-control study in Caucasian immunocompetent individuals to analyze the role of HPV in skin lesions in NMSC. 132 patients with RCC and 95 individuals without NMSC lesions were analyzed. Lesion material from patients with NMSC was collected from and near the lesions. In the control group, material was obtained from exposed parts of the body and from areas not exposed to sunlight. HPV prevalence was similar in both groups, suggesting that HPV is widespread in the general population. Compared with controls, HPV types of the beta-papilloma genus (HPV-EV) species 2 were more prevalent in NMSC, suggesting that certain HPV types may be involved in the progression of NMSC. However, additional factors are required for cancer to develop.
The detection and typing of HPV in NMSC is hampered by the genomic diversity of these viruses. Moreover, the methods used in the early 1990s were less able to accommodate this viral complexity. Despite significant advances in detection methods and the introduction of new primers, discrepancies in the prevalence and range of viral types found in these lesions continue to be observed across studies. Detection of mucosal HPV types in RCC is common, and HPV 16 is the most common. It can be assumed that the association of genital carcinoma and nail RCC, documented in a number of studies, is a consequence of autoinoculation from genital lesions. HPV 2, 31, 34, 35, 58, 61 and 73 were encountered less frequently than other types of HPV in cases of nail localization of BCC.
Benign mucosal lesions
4.1. Focal epithelial hyperplasia
Focal epithelial hyperplasia (FEH) or Heck's disease is a rare disease of the oral mucosa. It has a benign course and is associated with HPV 13 and 32. It is more common in children and women and has a clear racial predominance, being more common among American Indians, Eskimos and some African communities. It is clinically characterized by multiple small papules, pinkish in color, with the formation of plaques in the facial area. The lesions are asymptomatic and prone to spontaneous regression. The most common location is the lower lip. Less commonly, FEG spreads to the upper lip, tongue, oral mucosa, oropharynx and palate.
4.2. Condylomas acuminata
The most common manifestations of HPV in the genital area are anogenital warts or genital warts. These lesions are present as papules, nodules, or soft, thread-like, pinkish, pedunculated growths. They may have an exophytic growth and resemble cauliflower and are usually asymptomatic. HPV 6 and HPV 11 are most often found. High-risk HPV such as HPV 16 and 18 and other types of HPV can be found either isolated or (more often) in combination with HPV 6 and 11.
Buschke-Loewenstein tumor (giant condylomas or warty carcinoma of the anogenital region) is a clinically aggressive tumor, with an ulcerated, cauliflower-like surface, often with fistulas and abscesses. It has exophytic and endophytic growth, local invasion and a high tendency to relapse. Metastasis is very rare and histologically it is a benign tumor. This lesion is associated with HPV 6 and 11.
4.3. Bowenoid papulosis
The term bowenoid papulosis (BP) refers to a multifocal papular lesion on the genitals with histological features similar to BCC or BD. Its clinical manifestation is characterized by multiple brownish or erythematous papules located in the anogenital area, affecting mainly young people with an active sexual life. Clinically, it must be differentiated from seborrheic keratosis, melanocytic nevus and common warts. PD is strongly associated with HPV 16.
Despite histological atypia and association with high-risk HPV, the course of PD in men and young adults is usually benign, with spontaneous regression in many cases. In women, the association with cervical cancer suggests a less benign course, similar to women who have lesions and partners with PD. In the elderly and immunocompromised patients, its evolution also tends to be more aggressive. HPV 18, 31-35, 39-42, 48 and 51-54 are detected.
MALIGNANT LESIONS
4.1. Bowen's disease of the genitals
Cancer or BD of the genitals is associated with high-risk HPV, especially HPV 16. Clinically, it manifests as plaques, usually single, without a tendency to spontaneous regression and with the potential to develop into BCC. Characteristic lesions are erythematous, velvety, bright plaques with or without infiltration that may extend to the glans penis, foreskin, urethra, vulva, oral mucosa, tongue, and conjunctiva. Malignancy in BCC occurs in more than 30% of cases and higher. Research on the detection of HPV types in BD lesions is lacking. HPV 16 is the most common and HPV-EV 8 has also been detected.
4.2.Vulvar cancer
Invasive vulvar cancer usually precedes cervical cancer and often develops from long-standing genital warts. Detection of HPV in genital BCC occurs in 30%-70%. The detection of HPV in vulvar cancer is significantly lower than in cervical cancer. This may be due to the sensitivity of the methods used to detect the presence or new types of HPV not yet identified that may be present in the lesions.
HPV 16 is the most commonly observed type in genital carcinomas. HPV 18, 21, 31, 33, and 34 were also detected in these lesions.
4.3. Penile cancer
Clinically, lesions in the form of nodes, ulcerations or erosions may have a warty surface. Detection of HPV in penile cancer reaches 40-70% and the most common type is HPV 16.
4.4.Anal cancer
HPV is found in approximately 80–96% of anal cancer cases. The most common type is HPV 16. Other HPVs, such as HPV 18 and 33, are also found.
4.5.Cervical cancer
A high incidence of cervical lesions is associated with HPV, ranging from incipient cytological abnormalities and varying degrees of dysplasia to cervical cancer. A cause-and-effect relationship between HPV and cervical cancer is observed in approximately 90% - 100% of cases. Infection of the cervix with certain types of HPV is a precursor in the genesis of cervical neoplasia, although other associated factors may also contribute to the development of neoplasia.
HPV 16 and 18 are the two most important carcinogenic types and account for about 70% of cervical cancers. HPV 31, 33, 35, 39, 45, 51, 52 and 58 were also detected in cervical lesions.
Prognosis and prevention of basal cell carcinoma
The extremely slow growth of the tumor and the low probability of metastasis of basal cell carcinoma give a good prognosis in terms of complete recovery. Metastatic forms of basal cell carcinoma are extremely rare, so it is difficult to talk about accurate survival prognosis here. According to world literature, the average life expectancy of such patients is 4.5 years.
Prevention of cutaneous basal cell carcinoma involves regular protective measures against the aggressive effects of carcinogenic factors:
- Do not expose your skin to direct sunlight. At a minimum, use creams with sunscreen properties. Do not overuse tanning or visiting a solarium.
- When working with chemical irritants in hazardous production conditions, use personal protective equipment - clothing, gloves, masks.
- Do not neglect protective equipment when working with household chemicals.
In order to detect skin cancer in time and carry out treatment with minimal losses, it is recommended to undergo annual preventive examinations using dermatoscopy.
At Euroonko, this procedure is carried out using special German PhotoFinder technology. It involves drawing up a map of moles and neoplasms of the entire body, followed by tracking the dynamics of their changes. The resolution of the optical system allows visualization of skin tumors measuring only 0.9 mm.
When basal cell carcinoma is detected, we use treatment methods recommended by modern protocols. They give good clinical and cosmetic results. If you have any questions, please contact our specialists.
| Price : | |
| Oncologist consultation | 5,100 rub. |
| Dermatoscopy | 4,600 rub. |
| Histological examination | 5,200 rub. |
| PDT without contrast cost | RUB 39,600 |
Book a consultation 24 hours a day
+7+7+78
Reasons for the development of the disease
Currently, there is no clear answer to the question of what causes skin cancer. Like many other oncological diseases, skin tumors are considered a multi-etiological pathology. There are several predisposing factors, the presence of which increases the risk of developing a tumor focus. These include:
- Excessive exposure to ultraviolet rays on the skin. A similar situation occurs with prolonged and frequent exposure to sunlight, visiting a solarium, or working outside. Residents of the southern regions are at risk of developing skin cancer.
- Having light skin. Lack of melanin production increases the likelihood of skin tumors.
- Skin burn. A high degree of burn is accompanied by scarring of the skin. This process contributes to the emergence of latent carcinogenesis.
- Irradiation. Exposure to radioactive, ionizing rays has a detrimental effect on the skin. The risk of radiation dermatitis increases.
- Presence of skin contact with toxic substances. This group of carcinogens includes arsenic, aluminum, titanium, nickel and other heavy metals.
- Immunodeficiency. Conditions in which the body's protective functions decrease predispose to the formation of a tumor focus.
- Age. Most often, skin tumors affect people over 50 years of age.
- Concomitant systemic diseases. Doctors identify a group of pathologies in which the risk of developing skin cancer increases significantly. These include systemic lupus erythematosus, leukemia, and chronic skin diseases.
- Heredity. The presence of a skin tumor in previous generations of relatives is not a major risk factor. However, family history in combination with other predisposing conditions increases the possibility of developing skin cancer.
- Tattooing. In this case, there are two risk factors. This is a violation of the integrity of the skin and the introduction of paint with carcinogenic substances. Cheap tattoo ink may contain impurities of aluminum, titanium, and arsenic.
- A large number of nevi. Doctors urge you to monitor the condition of moles and contact a specialist if there is the slightest change. Traumatization of nevi increases the possibility of developing skin cancer.
- Excessive alcohol consumption, smoking. Chronic intoxication has a detrimental effect on the body as a whole. Against this background, the risk of tumor formation increases several times.
- Eating foods high in nitrates.