Cylindroma (syn: Spiegler's tumor, turban tumor) is a benign neoplasm of the skin, the primary focus of which comes from the cells of the sweat glands and hair follicles. Refers to rare types of neoplasms.
- Causes
- Symptoms
- Features of skin cylindroma
- Diagnostics
- Treatment methods
- Prognosis and further prevention
Tumor nodes are most often painless and localized on the scalp, but can spread to the face and ears. Both single and multiple nodes can occur. Typically, the size of one node is 1-2 centimeters in diameter, but it can be larger.
Causes
There are two types of cylinder - sporadic (randomly occurring) form of the tumor and hereditary.
The sporadic form most often occurs at the site of inflammatory foci of hair follicles, sweat glands or injured areas of the skin. With prolonged inflammation, adjacent cells can be modified and form nodes like a cylinder. However, the disease can occur without noticeable previous signs.
The hereditary form of the disease (Spiegler syndrome) can manifest itself in the form of two similar tumor processes of the skin: cylindroma or trichoepithelioma. In the vast majority of cases, one person will develop only one of these two types of tumor. However, the next or previous generation may have a different appearance. For example, the father has trichoepithelioma, and the son has cylindroma and vice versa.
Provoking factors for the occurrence and growth of a tumor are trauma, exposure to chemical agents, and previous operations of the head and face.
Introduction
Cancer begins when healthy cells change and begin to grow uncontrollably, forming a mass called a tumor. A tumor can be cancerous or benign. A cancerous tumor is malignant, meaning it can grow and spread to other parts of the body. A benign tumor may grow but not spread to other tissues.
Head and neck cancer
Head and neck cancer is a term used to describe a number of different cancers that develop in or in the throat, larynx, nose, sinuses and mouth.
Most head and neck cancers are squamous cell carcinomas. This type of cancer begins in epithelial cells, which make up a thin layer of surface tissue. Just below the epithelium, in some areas of the head and neck, there is a layer of moist tissue called mucosa. If cancer is found only in the squamous cell layer, it is called carcinoma in situ. If the cancer has grown beyond this cell layer and into deeper tissue, it is called invasive squamous cell carcinoma.
When head and neck cancer begins in the salivary glands, the tumor is usually classified as adenocarcinoma, adenoid cystic carcinoma, or mucoepidermoid carcinoma.
Types of head and neck cancer
There are 5 main types of head and neck cancer, each named according to the part of the body where it is found.
- Laryngeal cancer and hypopharyngeal cancer. The larynx is an integral part of the vocal apparatus. This tubular organ in the neck is used for breathing, speaking and swallowing. It is located at the top of the windpipe, or trachea. The hypopharynx (esophagus) is the lower part of the throat, surrounded by the larynx.
- Cancer of the nasal cavity and paranasal sinuses . The nasal cavity is the space behind the nose where air enters the throat. The paranasal sinuses are the air-filled areas surrounding the nasal cavity.
- Nasopharyngeal cancer. The nasopharynx is the air cavity at the top of the throat behind the nose.
- Cancer of the oral cavity and oropharynx . The oral cavity includes the mouth and tongue. The oropharynx includes the middle of the throat, from the tonsils to the tip of the voice box.
- Salivary gland cancer . The salivary gland produces saliva. Saliva is a fluid that is secreted in the mouth to maintain moisture and contains enzymes that break down food.
Other types of cancer can also be localized in the head and neck area, but their diagnosis and treatment are very different.
Symptoms
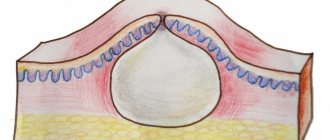
Cylinders are more often found in women in the form of isolated single nodes. A rarer form is multiple cylindromatosis (Brook-Spiegler syndrome). Initially, cylindromas appear as uniform reddish subcutaneous nodules with a smooth surface.
Soreness is not a characteristic symptom and can occur in the event of mechanical impact on the adjacent nerve trunk. Palpation does not cause significant discomfort, the tumor is homogeneous and mobile. The color of the tumor usually matches the color of the skin or has a slight reddish tint.
If a tumor occurs in the area of hair growth, the hair follicle moves away from the center of the tumor towards the edge of the tumor.
Where can I buy Israeli medicines?
- In an Israeli pharmacy - after consulting a doctor.
If you undergo examination at the oncology center, the doctor will prescribe you the necessary medications, which can be purchased in Israel. - At your place of residence - using a telemedicine program.
As part of this program, you will also receive a consultation from an Israeli doctor - but remotely. You can order the medications prescribed by him and have them delivered to your home.
Features of skin cylindroma
The tumor grows slowly and continuously. The diameter of a cylindroma can reach 7-8 centimeters after 10-15 years of stable growth. Ulceration of the tumor indicates its transformation into a malignant process. Cylindroma has no tendency to metastasize. The general condition of the patients remains unchanged, the neoplasm causes exclusively aesthetic discomfort.
Is it painful to remove warts?
Removing warts using cryodestruction is painful.
Painful sensations are observed both during the period of removal and after it, when an inflammatory reaction is formed.
If electrocoagulation or laser is used, there is no pain.
Because anesthesia is used.
When a wart is located on the scalp, topical anesthesia is usually used.
A cream containing prilocaine and lidocaine is applied to the skin.
After a few minutes, skin sensitivity disappears.
The doctor can remove the wart, and the patient does not feel anything during the procedure.
After its completion, when the anesthesia wears off, there is no pain either.
Diagnostics
To establish an accurate diagnosis of cylindroma, a tumor biopsy is necessary, since clinically (visually) the tumor is very easily confused with other types of pathology. Moreover, a biopsy with excision of a tumor site is the diagnostic method of choice, since puncture of a tumor with a needle can give false results.
On biopsy, cylindroma is described as a benign tumor with eccrine and apocrine differentiation. Usually making a diagnosis is not difficult.
In case of ulceration of the neoplasm or the presence of an inflammatory focus directly on the cylindroma or on adjacent areas of the skin, it is necessary to conduct a bacteriological examination. Such diagnostics allows you to identify the infectious pathogen and select the necessary antibacterial treatment if necessary.
Other diagnostic methods, such as ultrasound or dermatoscopy, may be prescribed by a doctor to determine the extent of tumor growth, but they are optional. The results obtained are of an auxiliary nature and are not used to confirm the diagnosis of cylindroma.
How does melanoma manifest?
Melanoma differs from basal cell and squamous cell skin cancer primarily in that, unlike previously described types of cancer that do not penetrate into the deeper layers of tissue, this tumor has the potential to grow and spread. The deeper it penetrates the skin, the higher the risk of its further spread throughout the body. Metastatic melanoma is an extremely dangerous disease. However, melanoma can be completely cured if it is detected at an early stage, before it has time to grow deeper into the skin and form metastases in the internal organs.
Melanoma not only penetrates deeper into the skin, but individual cells spread around the primary tumor. Therefore, when resection of melanoma, the surgeon necessarily removes a fragment of normal tissue. For example, if the tumor is comparable in size to a pencil cut, you need to additionally remove about a centimeter of healthy skin around the entire circumference of the melanoma - and possibly more if the cancer has penetrated into the deeper layers of the tissue.
When melanoma grows deep into the skin, there is a risk of it spreading to other organs. Typically, in cases of metastases, secondary lesions form in the lymphatic system, namely in the lymph nodes. Lymph nodes in the armpits, groin or neck begin to enlarge and can reach considerable sizes. From there, cancer cells can spread to internal organs. Therefore, in cases of deep germination of melanoma, the doctor not only removes the tumor itself, but also checks the lymph nodes. They should not show any signs of cancer spreading.
Check the price with a specialist
Treatment methods
The treatment method for cylindroma is selected by the doctor based on the results of the biopsy, as well as depending on the location and presence of ulcerations of the tumor. In general, cylindroma is well treated and disappears without a trace.
Surgery
A single cylindroma responds well to treatment by excision of the tumor node, even with a simple surgical scalpel. Surgery is performed under local anesthesia. However, in the case of atypical tumor localization or location near nerve and vascular trunks, doctors at the Euroonco clinic give preference to other types of treatment.
Laser treatment
Laser treatment allows you to remove a cylindroma with minimal trauma to surrounding tissue and, accordingly, with a minimal residual scar, sometimes completely invisible. This method of treating cylindromas involves the ability of a laser to burn out areas of the tumor.
Laser treatment is an alternative to classical surgery and can be used for small tumors. To remove large tumors, several sessions of such treatment may be necessary, or it is better to give preference to other methods.
Chemotherapy
In the presence of multiple nodes (Spiegler's syndrome), surgical or radiation treatment cannot be performed due to the large area of the lesion and possible complications in the postoperative period. In this case, preference is given to drug therapy aimed at suppressing tumor growth. Most often, combination treatment is used. The drugs can be used both systemically and locally in the area of development of the cylinder. Chemotherapy does not completely get rid of the disease, but only reduces the activity of the process.
Stages
Staging is a determination of where the cancer is located, whether and where it has spread, and its effect on other parts of the body.
Doctors use diagnostic tests to determine the stage of cancer; they may need information based on tissue samples obtained at surgery, so staging may continue until all tests are completed. Information about the stage helps the doctor determine which treatment is optimal and predict the possibility of recovery.
TNM tumor classification system
One way to determine the stage of cancer is the TNM system. Doctors use the results of diagnostic tests and scans to answer questions such as:
- Tumor (T): its size and location?
- Lymph nodes (N): extent of spread of the process to the lymph nodes?
- Metastasis (M): Has the cancer spread to other parts of the body?
The results are combined to determine each patient's cancer stage. Stage provides a common way to describe cancer so doctors can work together to plan the best treatment.
Who does BKR choose?
Basal cell skin cancer (BCS) most often affects men over 70 years of age - approximately 2 times more often than women of the same age group. However, there is no consensus on the predominance of BCC in people of different sexes - most authors believe that BCC occurs with approximately the same frequency in people of both sexes; in the samples of some authors, the predominance of BCC is indicated in either men or women. In case of BCC, a single lesion was found in different years in 94–99%, multiple lesions (from 2 to 7) – on average in 2.5% of patients in different areas of the skin [ 6
].
In the development of BCC, great importance is attached to genetic factors, the presence of xeroderma pigmentosum, immune disorders, adverse external influences - intense insolation, contact with carcinogenic substances, arsenic compounds, previous radiation therapy, increased photosensitivity, work with sources of ionizing radiation, contact with petroleum products, resins, local mechanical trauma [ 8
].
The main importance is given to excessive insolation. The greatest danger is posed by ultraviolet radiation, especially UV rays type A. A special risk group consists of people with fair skin and low melanin content (type I and II skin) [ 9
].