Facial skin diseases, main types
Human skin is capable of responding to any factors: both external (sun, wind, moisture) and internal (processes in the body).
The result of such reactions can be a variety of diseases that cause not only moral, but also physical discomfort. Therefore, at the first suspicion, and even more so symptoms of skin diseases, you should contact a specialist in order to avoid serious health problems and make your life comfortable. Being a kind of litmus test, our skin can react to anything: to changes in hormonal levels - acne, to long-term use of medications - rosacea, to sunbathing - rosacea, and so on.
Modern medicine identifies more than 600 skin problems, the vast majority of which are only the result of some factors, and only a small part of them are directly diseases of the epidermis.
The main diseases of the facial skin are:
- Anke - pimples and blackheads, the appearance of which is caused by disturbances in the functioning of the sebaceous glands;
- Rosacea is a small red or pink rash;
- Cuperosis - spider veins;
- Papillomas are neoplasms on the skin caused by a virus;
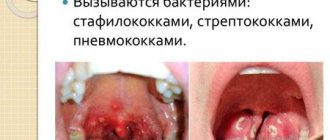
- Impetigo is an infectious purulent disease caused by streptococci and staphylococci (expressed in red tuberous rashes and spots);
- Keratosis - small spots covered with rough scales;
- Vitiligo - pink or milky-white spots with a round shape;
- Chloasma is increased skin pigmentation with clear boundaries;
- Seborrheic dermatitis is peeling of the skin in the nose and eyes, characterized by pain and itching.
Table of contents
- Expression and fine wrinkles
- Uneven skin color
- Wrinkles around the eyes
- Loose skin
- Rosacea
- Post-acne scars
- Changing the contours of the oval face
- Enlarged pores
- Accurate diagnosis of signs of aging and results of aesthetic procedures
- Principles of treatment
The first signs of aging and other aesthetic defects are changes in the structure, color and/or function of a skin area that cause concern to the patient.
In our company you can purchase the following equipment for correcting signs of aging and other aesthetic defects:
- Thermage (Solta Medical)
- Maximus (Pollogen by Lumenis)
- GeneO+ (Pollogen by Lumenis)
- UltraPulse (Lumenis)
- AcuPulse (Lumenis)
- Fraxel (Solta Medical)
- Antera 3D (Miravex)
Causes of facial skin diseases
Any skin diseases on the face do not occur on their own. They are, as a rule, provoked by third-party factors, with the search for which the treatment of any skin disease begins.
Improper skin care This is the most common cause of all kinds of problems and diseases of the facial skin. Thus, improper care can lead to severe contamination of the dermis and the proliferation of bacteria on it, which can ultimately lead to quite serious consequences.
Heredity It is very difficult to put in order the skin, the poor condition of which is caused by a person’s heredity. However, proper care for her, a healthy lifestyle and proper nutrition can significantly improve her condition.
Lifestyle Frequent stress, an unfavorable work environment, smoking, drinking alcohol, and poor-quality food - all this can affect the condition of the facial skin and even lead to skin diseases.
Diseases of internal organs As a rule, skin diseases on the face indicate improper functioning of the digestive system, kidneys or blood vessels. Also, weakened immunity, viruses and infections can provoke the appearance of acne, age spots and other skin problems.
Problems with the nervous system The main causes of various small rashes on the skin of the face are stress, which, unfortunately, awaits a modern person at every turn.
Wrinkles around the eyes
This is a clear sign of aging of the facial skin around the eyes of varying degrees of severity - from fine lines to large creases. Their main causes are chrono- and photoaging. A significant aggravating factor is smoking, which enhances the destructive effect of matrix metalloproteinases on extracellular matrix proteins (collagen, elastin) and contributes to the earlier appearance of wrinkles around the eyes.
One of the classifications of periorbital wrinkles is the following ( Fig. 4 ):
- Type I - wrinkles extend from the outer edge of the eye to the eyebrow and zygomatic process.
- Type II - wrinkles extend from the outer edge of the eye to the zygomatic process.
- Type III - single wrinkles are limited to the outer edge of the eye.
Find out more about wrinkles around the eyes and how to treat them here.
Rice. 4. Types of periorbital wrinkles (Tamura BM, Odo MY Classification of periorbital wrinkles and treatment with botulinum toxin type A. Surg Cosmet Dermatol 2011; 3(2): 129)
https://www.surgicalcosmetic.org.br - page 131, figure 2
Treatment of facial skin diseases
As mentioned above, the first step to successful treatment of any skin disease is to identify the factor that provoked it, since the entire course of treatment depends on this. It should be noted that self-medication for skin diseases on the face can be not only useless, but also dangerous.
If you are faced with skin problems on your face and want to get rid of them once and for all, then visit the ImageLab medical center, whose specialists will promptly make the correct diagnosis and prescribe an effective course of treatment.
The main thing is not to delay dealing with facial skin diseases, since even simple sagging or dry facial skin can ultimately turn out to be a serious disease requiring professional treatment.
Loose skin
Flabbiness of the skin occurs due to loss of elasticity and changes in the architectonics of connective tissue. These changes appear on any part of the body, but most clearly on the face.
The most important cause of sagging is age-related degradation of collagen and elastin. With aging, collagen fibers lose their ability to create an ordered network, begin to stick together with glucose molecules and form non-stretchable threads. The same thing happens with elastin fibers. Skin sagging is caused by photoaging, inflammasomes, chemotherapy in cancer patients, age-related syndrome due to hormonal changes in the body, micronutrient deficiency, smoking, etc.
Externally, loose skin is characterized by decreased tone, wrinkles, dryness, a tendency to sag, and a pale or yellowish tint ( Fig. 5 ). Find out more about sagging skin and how to correct it here.
Rice. 5. Skin laxity and other signs of aging compared to a youthful face (Health & Heldi)
Therapy results
Provided adequate treatment is prescribed, recovery is observed in 95-98% of cases. But even with the correct selection of treatment tactics, in a small number of cases a recurrence of basal cell carcinoma is possible.
After removal of the tumor, the patient should be monitored by an oncologist and undergo regular examinations in order to early diagnose a possible relapse. It is also necessary to remember that the development of basal cell carcinoma is promoted by excessive exposure to ultraviolet rays. For this purpose, patients are advised to limit their exposure to the sun.
Book a consultation 24 hours a day
+7+7+78
Changing the contours of the oval face
The gradual loss of an even facial contour is one of the first signs of skin aging and is usually observed in men and women after 45–55 years. The main reason for changes in facial contours is aging.
With age, the quality of the skin gradually deteriorates, the ligamentous apparatus of the muscular aponeurotic layer weakens, the volume decreases and redistribution of subcutaneous adipose tissue occurs in the middle and lower third of the face, and bone tissue is resorbed. Outwardly, this is manifested by a violation of the clear line of the oval of the face, loss of volume in the cheek-zygomatic region, the formation of deep nasolabial folds and “marionette lines”, drooping of the corners of the lips, and deepening of the chin fold. The face begins to look loose ( Fig. 8 ).
Find out more about changing the contours of the oval of the face and methods of non-surgical correction here.
Rice. 8. Changing facial contours over time (Pinterest
Post-acne scars
These are skin changes in areas where acne inflammatory elements are healing, associated with the formation of connective tissue. The vast majority of post-acne scars appear on the site of papules and pustules; much less often they occur in the area of comedones.
If the skin is damaged at the level of the papillary dermis, recovery can occur without gross defects - only depigmented areas with focal atrophy remain. With complete destruction of the basement membrane, a scar is formed ( Fig. 7 ) with the growth of coarse fibrous collagen, deformation of blood and lymphatic vessels. If collagen synthesis exceeds its destruction, the scar becomes hypertrophic - it bulges above the skin. If fibroblast activity becomes excessive, a large keloid develops due to tumor-like proliferation of immature connective tissue.
There are no post-acne scars:
- Hypertrophic.
- Keloids.
- Atrophic:
- chipped (icepick scars);
- rounded (rolling scars);
- rectangular (boxcar scars).
About half of acne scars disrupt the structure and/or function of the skin. They disfigure the patient’s face, negatively affect his emotional state and self-esteem, and can provoke psychological disorders and complexes about his appearance.
Find out more about acne scars and their treatment methods here.
Rice . 7 . Chip atrophic post-acne scars (Danish national service on dermato-venereology)
Causes of development of atopic dermatitis
Atopic dermatitis is being actively studied by dermatologists and allergists, but its causes have not yet been definitively established. It is a generally accepted fact that atopic dermatitis is based on a hereditarily determined excessive immune response to allergens, manifested by skin inflammation.
However, there is also a significant group of patients - about 20-30% - in whom hypersensitivity to any allergens has not been identified, but manifestations of atopic dermatitis are present [2].
Factors that provoke the development of the disease include:
- Genetic predisposition to the development of allergic reactions;
- Violation of the integrity of the skin barrier, facilitating the penetration of allergens and microorganisms into the deeper layers of the skin and the development of an allergic immune reaction;
- Excessive intake of allergens in early childhood from food (cow's milk protein, citrus fruits, chocolate, etc.);
- Impaired immunity after infectious diseases or against the background of a chronic illness.
Publications in the media
The morphological elements of the rash are the external expression of pathological processes that occur in the skin. Depending on the time of existence, the dynamics of the inflammatory process and under the influence of other reasons (scratching, secondary infection, etc.), the rash may change its original appearance during its evolution. Therefore, it is necessary to distinguish which rashes represent a typical picture of the disease, and which are the result of their further development. There are primary and secondary morphological elements • Primary morphological elements are rashes that appear on unchanged skin. Primary elements are divided into cavity and cavityless. Cavity-free elements include a spot, a blister, a nodule, a node, and a tubercle. Cavity elements have a cavity filled with serous, bloody or purulent contents. These include vesicle, bladder and abscess • Secondary morphological elements are rashes that appear on the skin as a result of the evolution of primary elements. These include hyperpigmentation, depigmentation, scaling, erosion, abrasion, ulceration, fissure, crust, scar, atrophy, lichenification and vegetation.
Primary morphological elements of the rash
A spot (macula) is characterized by a change in the color of the skin or mucous membrane in a limited area. The density of the spot does not differ from healthy areas and does not rise above the surrounding tissues. There are inflammatory and non-inflammatory spots. Inflammatory spots are caused by dilation of the blood vessels of the skin, disappear when pressing on them with a glass slide or finger and reappear when the pressure stops. They range in color from pale pink to bluish-red. Inflammatory spots measuring 2-25 mm - roseola; 2-3 cm or more - erythema. Roseola can be circumscribed or confluent; they are the most common symptom of infectious diseases. Non-inflammatory spots are characterized by the absence of inflammatory phenomena and do not disappear with pressure. With emotional excitement, neurotic reactions, large confluent and quickly disappearing non-inflammatory spots appear - erythema of shame, anger, etc. Among the spots caused by improper development of blood vessels in the skin, the most common are hemangiomas, which are a malformation of small veins and capillaries. Spots caused by persistent non-inflammatory dilatation of skin capillaries are called telangiectasias. When the permeability of the walls of blood vessels increases or they are damaged, hemorrhagic spots appear. According to size and shape, they are usually divided into: petechiae (petechiae) - pinpoint hemorrhages; purpura - hemorrhages with a diameter of 1–2 cm; ecchymoses - hemorrhages more than 2 cm in diameter; linear hemorrhages (vibices), bruises (sugillationes). The color of hemorrhagic spots changes sequentially over 2–3 weeks from red, then blue, green, yellow, light brown, dirty gray. When pressing on hemorrhagic spots, their color does not change. Hyperpigmented spots appear as a result of the deposition of melanins in the skin. There are congenital (most often nevi) and acquired (photodermatoses, freckles, etc.) hyperpigmented spots. When the content of melanin in the skin decreases or disappears, depigmented spots appear. There are congenital depigmented spots (albinism) and acquired ones. Non-inflammatory stains include stains from artificial injection of paints (tattoos, professional stigmas).
A blister (urtica) is an acutely inflammatory, cavityless element slightly raised above the skin, ranging in size from 2-3 mm to 10 cm or more, usually disappearing quickly and without a trace. It occurs as a result of limited acute inflammatory edema of the papillary layer of the skin with simultaneous dilation of the capillaries. The developed urticarial element has a pale porcelain-white color in the center and pinkish-red along the periphery, accompanied by itching and burning. Blisters are observed with urticaria, Dühring's dermatitis herpetiformis, etc.
Papule , or nodule (papula) is a cavity-free formation of dense or soft consistency protruding above the skin level. Papules are divided into inflammatory and non-inflammatory, according to their depth into epidermal, dermal or epidermal-dermal. The size of the papules varies. There are miliary (1-1.5 mm), lenticular (2-3 mm), nummular (2-3 cm) and larger papules - plaques. The shape and outline of the papules are different. They can be flat, hemispherical, cone-shaped, polygonal, etc. The surface of the papules can be smooth or covered with scales.
A tubercle (tuberculum) is a limited and dense formation protruding above the surface of the skin from pink-red to bluish-purple, ranging in size from 1-2 mm to 10 mm. They are formed as a result of the accumulation in the dermis of an inflammatory infiltrate such as an infectious granuloma. The tubercles can disintegrate, forming an ulcer, or resolve by replacing the infiltrate with connective tissue with the formation of a scar or cicatricial atrophy of the skin in their place.
A node (nodus) is a limited dense formation with a diameter of 1 to 5 cm or more, round or oval, located in the deep layers of the dermis or subcutaneous fatty tissue. The nodes may rise above the surrounding skin or be determined only by palpation. Nodes are divided into inflammatory and non-inflammatory. Inflammatory nodes are characteristic of infectious diseases (syphilis, tuberculosis, etc.), erythema nodosum; the color of the skin over them varies from pale pink to bluish-red; Nodes of this kind most often ulcerate and end with a scar, but can resolve without leaving a trace. Non-inflammatory nodes occur with various skin tumors or as a result of the deposition of metabolic products in it.
Bubble (vesicula) is a superficial (within the epidermis) and slightly protruding above the surrounding skin cavity formation with serous or serous-hemorrhagic contents, ranging in size from 3 to 5 mm. Blisters are observed in eczema, dermatitis, lichen simplex, etc.
A bubble (bulla) is a cavity element measuring from 0.5 to 5 cm or more with serous, bloody or purulent contents. The blisters can be located under the stratum corneum, intraepidermal or subepidermal. Blisters are found in pemphigus, Dühring's dermatitis herpetiformis, acute dermatitis, etc.
An abscess (pustula) is a cavity element with purulent contents. Varieties: pustule developing around the hair follicle - folliculitis; superficial pustule not associated with the hair follicle - phlyctena; non-follicular pustule developing in the dermis - ecthyma; pustules located around the sebaceous glands - acne.
Secondary morphological elements of the rash
Skin dyschromia (dischromia cutis) is a pigmentation disorder that occurs at the site of resolved morphological elements of the rash. Hyperpigmentation appears as a result of an increase in melanin content or hemosiderin deposition in the skin. A decrease in melanin deposits in the skin causes secondary hypo- or depigmentation. Secondary hypo- or hyperpigmentation disappears without a trace.
Scale (squama) is an accumulation of rejected cells of the stratum corneum that have lost contact with the underlying epidermis. The scales can be loose, easily scraped off (psoriasis, parapsoriasis), or tightly attached to the skin (lupus erythematosus), small-lamellar (measles, pityriasis versicolor), large-lamellar (scarlet fever, toxicoderma).
Erosion (erosio) is a skin defect within the epidermis. Erosion occurs due to the opening of a vesicle, blister, or disruption of the integrity of the epithelium on the surface of the papules.
Abrasion , excoriation (excoriatio) is a skin defect that appears as a result of mechanical damage.
An ulcer (ulcus) is a deep skin defect that involves the epidermis, dermis and often underlying tissues. It develops as a result of the disintegration of such primary elements as a tubercle, node, pustule. Ulcers can also occur as a result of tissue necrosis caused by trophic disorders due to vascular changes (atherosclerosis, chronic venous insufficiency). After the ulcer heals, a permanent scar always remains in its place.
Crack (rhagas, fissura) - linear defects (tears) arising due to loss of elasticity and infiltration of individual areas of the skin. There are superficial cracks (fissurae) that develop within the epidermis and heal without a trace. And deep cracks (rhagas), involving, in addition to the epidermis, also part of the dermis, and sometimes deeper-lying tissues and leaving behind scars. Most often, cracks form in places of natural folds and in areas subject to stretching (in the corners of the mouth, above the joints, etc.).
A crust (crusta) forms on the skin as a result of the drying of the weeping surface. There are serous, purulent and bloody crusts. Their color depends on the nature of the drying discharge and the particles of dust, medicinal substances, etc. mixed with it. Crusts can be thin, flat, thick, conical, layered, dense, loose, etc. Elements of a mixed nature—crust-scales—occur in cases where exudate impregnates the scales.
A scar (cicatrix) is a coarse fibrous connective tissue growth that replaces deep skin defects. Fresh scars are pink-red in color, while older ones are hyperpigmented or depigmented. Scars can be flush with the surrounding skin, raised above it (hypertrophic scars) or sunken (atrophic scars). Cicatricial changes - cicatricial atrophy - can be observed without a previous ulcerative lesion, as a result of the replacement of infectious granulomas (with tuberculosis, syphilis) or extensive infiltrates (lupus erythematosus) with connective tissue. Unlike ordinary scars, cicatricial atrophy develops in smaller quantities and more delicate connective tissue. At the same time, the affected skin becomes sharply thinner, easily gathering into folds like tissue paper.
Lichenification (lichenificatio) - thickening, hardening of the skin, accompanied by an increase in its normal pattern, hyperpigmentation, dryness, and roughness. Lichenification is observed in neurodermatitis, chronic eczema, etc.
Vegetation (vegetatio) is formed as a result of the growth of the spinous layer of the epidermis and the papillary layer of the dermis. It is a villous-like formation that develops on the surface of papules, inflammatory infiltrates, erosions, etc. Their surface can be covered with a stratum corneum or eroded.
ICD-10 • R21 Rash and other nonspecific skin eruptions
Symptoms and types of atopic dermatitis
The first manifestations of the disease in children are usually noted at the age of 6 months in 45%, up to 1 year in 60%, and up to 5 years in 85% of cases. [5]
Depending on age, the following forms of atopic dermatitis are distinguished:
- infant (from 1 month to 2 years);
- children's (from 2 to 12 years);
- teenage (over 12 years old).
A triggering factor for the development of AD in an infant can be a food allergy and it manifests itself in the form of rashes on the baby’s cheeks, thighs, legs and arms. In severe cases, large areas of the skin may be affected. The rashes are moist, weeping, and are accompanied by severe itching of the skin, which significantly disrupts the quality of life of both the baby and his mother. As a result of scratching, wounds appear on the baby’s skin, which are entry points for fungi, viruses and bacteria. Therefore, in the absence of proper care and timely treatment, children with atopic dermatitis have a high risk of secondary infection. This form of atopic dermatitis is often called exudative diathesis.
As children grow older, the disease may go away on its own. But in approximately 50% of children, atopic dermatitis persists [3]. At the same time, the manifestations of the disease also change - wet rashes disappear, and instead of them, itchy, dry areas of skin appear, sometimes with a rash in the form of nodules and microbubbles. The location of the rashes also changes - now they are in the area of the folds - knees, elbows, wrists; on the back of the neck. Doctors often differentiate these manifestations of the disease from neurodermatitis.
After 12 years, with the onset of adolescence, the clinical picture of the disease changes again. In adolescents and adults, it manifests itself as rashes on the backs of the hands, feet, and fingers, and is often accompanied by severe, unbearable itching. In severe forms, the disease can affect large areas of skin throughout the body.
What does atopic dermatitis look like on the face?
The key symptom of atopic skin is severe itching. Along with it, redness forms on the surface of the face, often accompanied by weeping and the formation of crusts, since damage to the facial skin is characteristic of the infant and child form of atopic dermatitis. Frequent “companions” of atopic dermatitis on a child’s face are other manifestations of atopy:
- bronchial asthma;
- allergic rhinitis;
- allergic lacrimation from the eyes.
Ignoring the problem and expecting the rash to go away on its own is a big mistake. It is much more correct and effective to contact a specialist to prescribe adequate therapy and personal selection of medications.
What is atopic dermatitis (AD)?
The term “atopic dermatitis” was proposed back in 1935, but was introduced into medical practice much later – in 1972.[1]
Officially, “atopic dermatitis” was adopted only in 1992 and introduced into the ICD-10 classification of diseases. This explains the existence of a large list of synonyms that are still used to designate the manifestations of this specific skin disease by doctors from different countries. Among the medical definitions of this disease one can find such as exudative diathesis, eczema, neurodermatitis, atopic eczema, childhood eczema, atopic dermatitis. So, atopic dermatitis is a chronic inflammatory skin disease that develops in individuals with a genetic predisposition to allergies and is characterized by rashes, severe itching and increased sensitivity to allergens.
The prevalence of atopic dermatitis among children reaches 15–30%, among adults – 2–10% [5]. Atopic dermatitis can be the debut of the so-called “allergic march”, when in the future such patients develop other atopic diseases, for example, food allergies, bronchial asthma, allergic rhinitis.
In recent decades, there has been a significant increase in the incidence of AD. The disease brings quite a lot of problems to patients and significantly worsens their quality of life.