What are atopic diseases and why do they occur?
Atopy is a tendency to develop diseases associated with the immune system’s reaction to allergens and external irritants to which it normally does not respond.
Let's try to simplify the mechanism of atopy development. After exposure to an irritant, the body produces special antibodies - type E immunoglobulins. These are proteins that cause cells to secrete special substances, in particular histamine, which trigger an inflammatory reaction and a number of other changes.
The inflammatory response is a universal protective reaction of the body. Usually it helps to cope with harmful microorganisms, but with atopy there are no microbes, which means that the inflammatory process starts in vain and can cause harm.
Atopy and allergy are not the same thing, although the terms are sometimes used interchangeably and can be used interchangeably. The difference is that in atopic diseases, an enhanced immune response is always associated with the production of immunoglobulins type E, while an allergy is any enhanced immune response to any antigen, regardless of its mechanism. That is, we can say that all atopic diseases will be allergic, but not all allergic reactions will be atopy.
As a result of the immune reaction, a person with atopy faces a variety of manifestations - he may have a skin rash, cough, runny nose, itching, red eyes, difficulty breathing and other manifestations of atopy, which depend on which organ is more “damaged” by the immune system reaction .
Atopic and allergic diseases are a whole group of diseases. These include bronchial asthma, allergic rhinitis, atopic dermatitis, chronic polypous rhinosinusitis. One person can have several atopic diseases at once, or over time, one replaces the other. Thus, approximately 75% of children with atopic dermatitis may develop allergic rhinitis, and more than 50% may develop asthma. In adulthood, polypous rhinosinusitis may appear. This is because atopic diseases have a common cause.
It is not yet known exactly why some people are prone to atopic diseases and others are not. It is believed that two factors play a role in the occurrence of such diseases:
- Genetics. There is a hereditary predisposition to atopic diseases. Moreover, this is precisely a predisposition, and not a pattern - that is, if the parents had atopic diseases, the child may not have them. And vice versa - parents can be healthy, but the child exhibits atopic diseases.
- Impact of the external environment. Some environmental factors can trigger the development of the disease and also worsen its course. Such factors are called triggers.
There is also now a hygiene hypothesis - its essence is that an almost sterile environment in childhood and fewer childhood infections may be the reason for the increase in cases of atopic diseases. That is, excessive hygiene or avoidance of contact with anything that can cause an allergic reaction increases the risk of atopic disease, since the immune system does not have the opportunity to become familiar with the required number of allergens. As a result, she may then react too strongly to something that she usually does not react to, from dust to certain types of food. This is just a theory for now, but it is being actively studied.
Atopy
The term "atopy"
, which comes from the Greek word meaning
"foreign"
, was first introduced in 1922 to define forms of hypersensitivity of the body to environmental factors.
Manifestations of atopy are various allergic diseases and their combinations. Their natural development during a person’s life is called “allergic”
or
“atopic march”
.
What does he look like?
The first signs of atopy
appear soon after the birth of a child in the form of food allergies and reach their peak by the middle of the first year of life.
At the same age, an increase in symptoms of atopic dermatitis
. Subsequently, the prevalence of atopic dermatitis decreases. But the symptoms of bronchial asthma gradually increase, and by the age of 6–7 years they come first.
However, by adolescence
Allergic rhinitis
begins to occupy a leading position .
The entire atopic triad from the point of view of Tibetan medicine refers to the “disturbance” of one of the three doshas: Mucus, Bile, Wind
. In childhood, the disease is most often caused by a violation of Mucus and Bile.
Is it possible to stop the atopic march using ancient medicine?
ATOPIC DERMATITIS (AD)
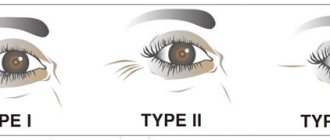
It is divided into three successive phases: infant, child and adult, and each has characteristic features.
In children, the extensor surfaces of the limbs, neck, elbow and popliteal fossae, and dorsum of the hand are usually affected; in adults, damage to the skin of the face and neck (red face syndrome), décolleté and skin of the hands, feet, and fingers is more common.
Weeping usually indicates a secondary infection. But in any phase, dry skin, itching, thickening of the skin, peeling, hyperemia and rashes typical for each age are typical.
According to several studies, approximately half of patients with AD subsequently develop bronchial asthma, especially in severe cases, and two thirds develop allergic rhinitis. Therefore, it is so important that treatment is aimed not only at preventing exacerbations of atopic dermatitis itself, but also at preventing the development of other forms of atopic disease.
Modern medicine is practically powerless against atopic dermatitis. The emphasis is on eliminating or reducing contact with the allergen, prescribing antihistamines, enzymes and vitamin preparations. Unjustifiably often, doctors use hormonal and immunosuppressive drugs to treat children.
However, the disappearance of skin symptoms in practice only means that the disease has gone inside. If we consider it from the perspective of Tibetan medicine, this disease is quite treatable - since the reasons for its development have been clarified.
All skin diseases are part of a general damage to the body based on disturbance of the constitutions Mucus (lymphatic and endocrine systems), Bile (digestion) and Wind (nervous system). The root cause of disruptions in the functioning of these systems is poor lifestyle and nutrition. At the same time, the skin is a mirror reflection of the state of the body and the functioning of internal organs.
In a child’s body, the “cold” constitution of Mucus (symbolizes growth, development) prevails over all other life principles. Very often, failure to comply with the basic rules of a healthy lifestyle and nutrition can easily throw Mucus out of balance in a fragile child’s body, and lead to a breakdown of other life principles in the body - Wind and Bile.
Any external manifestations, changes in skin color and texture, itching and others are perceived as a signal of these disorders that have gone quite far. Parents, following the recommendations of doctors, follow a “strict diet” for food allergies and atopic dermatitis. This is where the root of the trouble lies. For example, a child’s diet includes foods such as oatmeal and rice porridge, pork, zucchini, pumpkin, onions, dill, olive oil, sour cream, goat’s milk and cottage cheese, juices, and some fruits. What happens? Instead of having a therapeutic effect, such a “diet” only worsens the condition of a child prone to allergies.
All these products are “cold”. Especially pork, bananas, sour cream, goat milk and goat milk cottage cheese, water and juices. They slow down metabolic processes in the body, and in particular suppress the “fire” of the stomach - its “fiery warmth”, accumulate mucus in the body.
Additional factors in the development of atopic dermatitis are frequent hypothermia of the child (including as a result of parents' passion for hardening!), experienced stress or a nervous situation in the family.
In addition, modern medicines that are often used in pediatric practice, such as multivitamins, enzymes, and immunomodulators, are “Yin” remedies, and also cause an increase in mucus in the body and bile disorders (malfunctions in the digestive system), disrupting metabolic processes in the body.
BRONCHIAL ASTHMA
The next step in the development of the atopic march. Prolonged “perturbation” of Mucus, left in infancy without proper treatment, leads to its accumulation in the body, in particular in the bronchi and lungs.
Asthma is characterized by periodic attacks of suffocation or difficulty breathing due to bronchospasm, which are accompanied by a dry cough and wheezing in the bronchi. The mechanism of the disease is that excess mucus in the bronchi narrows their lumen and interferes with breathing (the “cold” scenario). If an inflammatory infectious process develops in the bronchi, their walls swell and thicken, which also causes a narrowing of the lumen between them (the “heat” scenario). The greater the narrowing of the lumen, the more difficult breathing is.
In both cases, bronchial spasm causes an acute attack of suffocation - the muscles surrounding the bronchial tubes contract sharply, narrow the bronchi, and air stops flowing through them. This is how an attack of suffocation occurs.
At the first stage, attacks can occur once or twice a year, at the second - once or twice a month or a week. And finally, when the disease enters the third stage, the attacks become constant and prolonged, causing severe fear in the child.
In the European part of Russia, ace is most often found, that is, mucus caused by disturbance of the constitution. The reasons for the accumulation of mucus in the bronchi are regular consumption of food chilled in the refrigerator, cold water and drinks. And also yin, that is, “cold” products: milk, kefir, yoghurt and curd cheese, potatoes, bakery and confectionery products, milk porridge, raw vegetables and fruits.
The disease is provoked by hypothermia of the body, especially in damp and humid climates, “hardening” procedures, untreated and suffered bronchitis, tonsillitis, flu, pneumonia and other respiratory diseases. Prolonged inflammation leads to a change in the quality and increase of mucus in the bronchi, and a general violation of the constitution of the mucus causes its accumulation, clogging and narrowing of the lumen of the bronchi.
ALLERGIC RHINITIS
It is the final stage in the development of the atopic march. Watery eyes, stuffy nose, sneezing, itching, asthma attacks, weakness - these are its signs. Atopic rhinitis is often combined with bronchial asthma, but it also exists independently in two forms: an acute form, often seasonal (hay fever, hay fever) and year-round allergic rhinitis.
These forms are combined with conjunctivitis (inflammation of the mucous membranes of the eye) - usually in the spring, occurring as an allergic reaction to pollen. The main symptoms of allergic rhinitis: spontaneous sneezing, itchy nose, stuffiness, lacrimation.
During allergic rhinitis, several stages are observed: from periodic nasal congestion to constant, when chronic swelling forms, and the possible appearance of polyps - growths of the nasal mucosa or paranasal sinuses, which gradually close the nasal passages. In severe cases, hay fever is accompanied by asthmatic attacks of suffocation, cough, skin rashes, and high fever.
Any allergy imposes very strict restrictions on the patient’s lifestyle. Not to mention the fact that difficulty breathing affects the tone of the blood vessels in the brain, the level of intracranial and ocular pressure, and constant itching can drive you crazy.
Allopaths usually prescribe vasoconstrictors and antihistamines, but these, only symptomatic treatments, improve the patient's condition temporarily.
TREATMENT
For allergic diseases, it primarily means proper nutrition. There should be yang food on the table, that is, “hot” food. To do this, boiled and stewed foods must be served piping hot, and must be seasoned with spices. Any are good - pepper, ginger, cardamom, coriander, onion, garlic and others, as well as table salt.
Food must have sour, salty and spicy tastes. Ginger drink is very useful, which includes three tastes (spicy, sour and sweet) and contains Yang energy.
Recommended meats include horse meat, lamb and beef (it contains medium and low heat elements) stewed and with seasonings; if you cannot do without milk, be sure to boil it; raw vegetables and fruits are contraindicated; they are best served stewed, baked or boiled; instead of sweets and cakes, berries, dried fruits and nuts are suitable.
It is better to drink compotes, fruit drinks, jelly. All food should be hot; drink - under no circumstances should it be cold.
A separate power supply principle is preferable.
We prescribe Tibetan herbal remedies that harmonize all three constitutions and have no side effects. In the complex treatment of atopic dermatitis, external methods of influence are widely used - treatment of the affected surface with a beam needle, cauterization with wormwood cigars, rubbing with a special liquid based on herbs "Clean Skin", which has an almost instantaneous therapeutic effect for severe itching and scratching, as well as ointments that contain Only herbal ingredients and oils are included.
Symptoms of atopic dermatitis disappear within a week - provided proper nutrition.
The Naran Clinic has accumulated extensive experience in the treatment of bronchial asthma and allergic rhinitis.
Tibetan medicine has unique herbal remedies for removing excess mucus from the body:
“Jubril”, “Dali-16”, “Pangen-12”, “Pangen-15”, “Darbu-5”, “Darb-19”, “Sembru”.
Such procedures as acupressure, moxibustion with wormwood cigars, stone therapy, and vacuum therapy provide excellent results.
The complex treatment method developed by us helps people of any age either completely get rid of asthma and obsessive runny nose, or control the symptoms of the disease - do not give the disease a chance to get the better of them.
Svetlana Choizhinimaeva, Candidate of Medical Sciences
How do common atopic diseases manifest and when should you see a doctor?
Bronchial asthma is a chronic lung disease that affects more than 300 million people worldwide. In Russia, the prevalence of the disease among adults is 6.9%, and among children and adolescents - about 10%. This is the most common chronic disease in children.
In asthma, the inflammatory immune response narrows the airways and can cause bronchospasm, making it difficult for air to get in and out of the lungs. As a result, cough, shortness of breath, suffocation, difficulty breathing, wheezing, and chest tightness appear.
Coughing with asthma can be constant, and it often interferes with sleep—it happens that it gets worse at night and in the morning. Shortness of breath occurs during exercise, but can also occur at rest. Breathing disorders can lead to a feeling of constant fatigue, problems with sleep, and poor health.
If such symptoms appear, you should consult a doctor: with adequate treatment, asthma attacks occur less frequently, and a person can live a full life.
Atopic dermatitis is a chronic systemic inflammatory skin disease. According to statistics, it affects approximately 15–20% of children and 1–3% of adults worldwide.
Dry patches appear on the skin with atopic dermatitis; severe itching and pain are possible in these areas. For some people, the rash appears in small areas of the body, while for others it can cover a large area.
The disease most often occurs with exacerbations and remissions: that is, the condition of the skin either improves or worsens. Atopic dermatitis occurs more often in people whose relatives suffer from the same disease, asthma or food allergies.
There are two hypotheses explaining the development of the disease:
- “from the inside out” - triggering an immune system response weakens the skin barrier and leads to symptoms;
- “outside in” - weakening of the skin barrier function (in particular, due to dysfunction of the filaggrin protein, which is part of the skin epithelium) allows allergens to penetrate inside and develop an immune response.
The insidiousness of the disease is that it is associated with an increased risk of multiple comorbidities, including food allergies, asthma, allergic rhinitis and even mental disorders. Thus, 60% of patients with atopic dermatitis may have a tendency to develop bronchial asthma, and 30–40% develop it.
The disease most often develops in children under 5 years of age—this happens in 85% of cases. Early diagnosis and treatment of atopic dermatitis are important to prevent complications and improve quality of life.
Chronic polypous rhinosinusitis . This disease is characterized by inflammation of the paranasal sinuses with the appearance of polyps - benign outgrowths of the mucous membrane. It occurs in approximately 1–4% of adults and most often develops after 40 years of age.
Symptoms of the disease include a runny nose, nasal congestion, facial sinus pressure or pain, and decreased sense of smell for more than 12 weeks. Often, the disease greatly reduces the quality of life and often leads to the need for sinus surgeries: on average, people with chronic polypous rhinosinusitis undergo up to 3 such surgeries. Up to 67% of people with this disease also have asthma.
A prolonged runny nose and accompanying symptoms are a reason to consult a doctor and undergo additional examination. Treatment in such cases usually differs from the treatment of a runny nose caused by colds and other diseases, so it can be difficult to cope with polypous rhinosinusitis on your own.
Symptoms of atopy
Let's imagine the structure of human skin in the form of a wall.
Atopic dermatitis has two main phases - exacerbation and remission. In the acute phase, inflammation, itching, weeping, and crusting are observed. Remission between two exacerbations is characterized by severe dryness and dehydration of the skin.
Symptoms that require consultation with a dermatologist:
- itchy rash: difficult to detect in infants, but a clue may be the appearance of a sleep disorder;
- rough thick skin;
- the spots suddenly begin to itch;
- crusts appear on them.
Another clue is the location of the foci of inflammation.
In children they occur in different places:
- in infants, as a rule, on the face, especially often on the cheeks and chin;
- in older children - on the knees, wrists, elbows and neck.
An exacerbation usually begins with the appearance of itchy red spots.
Once the diagnosis is made, it is necessary to carefully care for the wounds. Then the skin condition will quickly return to normal, and additional protection for the patient will not be needed. The most important thing in treating the disease is to restore the protective functions of the skin, since it plays the role of a natural barrier that prevents external irritants from penetrating inside. This is better than looking for dust mites or pollen, which is almost impossible and extremely tiring for parents!
Recent studies have shown that the more you try to protect your child from any irritating factor, the higher the risk of developing manifestations of atopic dermatitis. Therefore, the maximum that should be done is to select more gentle hygiene items, use emollients, and apply local treatment with corticosteroid drugs.
How do doctors make a diagnosis of atopic diseases?
Atopic diseases can manifest in different ways. Frequent symptoms are a runny nose, sneezing and nasal congestion if the upper respiratory tract is affected, difficulty breathing, coughing, suffocation and shortness of breath if the bronchi and lungs are affected, as well as rash, itching and redness if the skin and mucous membranes are affected.
The patient's medical history plays a key role in diagnosis. Collecting disease information can be more accurate and reliable than various laboratory tests or screenings. For example, with atopic dermatitis there are no specific tests or studies to confirm the diagnosis, although they may be prescribed to rule out other diseases.
Sometimes blood tests, such as immunoglobulin E, and other tests will be needed to look for polyps in the nasal cavity.
Basic questions your doctor may ask:
- How often do the symptoms of the disease occur, how long do they persist, and how the nature of the attacks changes over time.
- What causes attacks of the disease, if the triggers can be determined.
- Are the attacks associated with seasonal conditions, such as changes in weather, or any specific situations?
- Did any of your relatives have similar symptoms or other atopic diseases?
- What treatment the person used and how the disease responded to it.
Atopic diseases must be distinguished from infectious and inflammatory diseases and frequent colds. That’s why it’s so important to tell your doctor in detail about your symptoms, their development, and how they occur.
On the Atopia Live website there is a reminder for preparing for a doctor’s appointment. It will help you not to forget about important details - the more detailed and accurate you tell the doctor about the symptoms of the disease, the faster the diagnosis will be made.
How to prevent exacerbations of atopic diseases
Exacerbations are often triggered by environmental irritants. This could be food, cosmetics, household chemicals and anything else.
That is, according to one theory, contact with allergens and irritants from the external environment can prevent atopic diseases in a child. However, when atopic disease already exists, a different tactic is needed. The important thing here is to identify your allergens and triggers and avoid them - this will be part of the treatment.
For people living with atopic diseases, triggers and allergens are individual - some will react to dust, some to certain foods, and some to dry air.
It is important to remember that exacerbation of the disease may occur some time after exposure to the provoking factor. Because of this, it is not always easy to understand what specific trigger caused the condition to worsen.
The most common provoking factors:
- Irritants. Cleaning and detergents, cosmetic components, clothing materials, cigarette smoke, in general, any chemical compounds that can enter the body through the skin or respiratory tract. Which irritants provoke an exacerbation partly depends on the disease. For example, in case of asthma, this could be tobacco smoke, and in case of atopic dermatitis, it could be substances that come into direct contact with the skin, such as household chemicals.
- Allergens - food, pollen, animal dander, medications, mold and any others. They can cause an immune reaction both in atopic dermatitis and in other diseases.
- Dust and house dust mites. At home, a person is constantly in contact with this trigger, so it is difficult to identify. You can suspect a reaction to house dust mites if there is an “elimination effect” - an improvement in the condition of the skin when in a dust-free environment. You can reduce the number of mites and dust at home if you refuse down pillows and blankets, carpets, upholstered furniture, and also organize frequent cleaning of the premises.
- Stress. It affects the state of the immune system and can ultimately provoke an exacerbation of the disease. Sometimes psychotherapy is used to treat atopic diseases, and it can alleviate the person’s condition.
- Infections, especially viral ones. For example, exacerbations of bronchial asthma often occur after infectious respiratory diseases.
It is important for every person with atopic diseases to find their allergens and triggers and minimize their exposure.
To do this, you can keep a diary, noting the characteristics of the attacks of the disease and after what they occurred. With atopic dermatitis, it is also important to choose the right skin care - those non-drug products that will soften inflammation and eliminate dry skin, rather than irritate it. On the Atopy Live website you can read more about atopy triggers and download a skin care guide for atopic dermatitis.
Factors that aggravate atopy
First of all, do not confuse the factors that provoke attacks with the true cause of atopic dermatitis - damage to the skin.
An exacerbation can be triggered by many factors, and it cannot be prevented. Irritants are found in the environment and food, and even emotions can cause inflammation, although it is impossible to explain their critical role in the frequency and severity of attacks.
Teething and ear, nose and throat diseases can trigger an attack of atopic dermatitis in infants. In addition, everyone’s reaction to provoking factors is individual.
The most common provoking factors:
- dust, dust mites and pollen present in the air;
- soap, household cleaning products, washing powder;
- tobacco and environmental pollution;
- heat (+ sweat) and very dry air;
- clothes that irritate the skin: wool, synthetics...
- Pets;
- situations associated with emotional stress;
- teething;
- temperature difference;
- food allergens;
- swimming in the sea or pool.
Be that as it may, you should control inflammation when the first signs appear, rather than trying to get rid of the irritants.
Can atopic diseases be cured?
Atopic diseases cannot be cured, but you can live with them, completely controlling the disease. If you choose the right treatment, the symptoms can be relieved and the quality of life will improve. To do this, it is important to follow your doctor's recommendations, take medications if prescribed, and eliminate triggers that cause exacerbations.
If the disease began in childhood, its manifestations may go away or soften as they grow older. For example, with atopic dermatitis, up to 70% of children outgrow the disease, meaning it disappears over time.
If you have reasons to suspect an atopic disease or you feel that its symptoms have intensified, you should seek advice from specialized specialists.
The Atopia Live website contains a list of expert centers where you can get medical help for atopic diseases. To search, you need to enter the address and select the appropriate clinic.
Material supported by Sanofi. The information does not replace specialist advice.
MAT-RU-2200324-1.0-01/2022
Sources