Mole or medical term Nevus.
This is a collective name for limited, benign formations of the skin or mucous membranes.
The development of which is based on melanocytes - specialized skin cells that produce melanin.
Fair-skinned people have an average of 20 to 30 nevi.
Some are congenital or develop after birth in young children.
With age, the number of moles may increase, which is not considered a pathology.
Acquired moles are associated with the accumulation of pigment-forming cells.
Such as melanocytes in the upper layers of the skin.
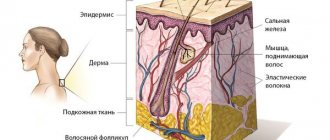
If we consider in detail, the nevus is located either in the epidermis, in the dermis (corium), or at the border between these layers of skin.
Such spots can vary in color, being light, dark brown and even black.
Some moles are flat, others are raised.
Intense and constant exposure of the skin to ultraviolet light, as well as hormonal causes, cause or accelerate the development of birthmarks.
In principle, the development of moles is a complex process.
Biological factors and the environment play an important role.
Nevus is usually benign.
Therefore, the reasons for surgical removal are mainly cosmetic.
Only if the spot is perceived as alarming, for example, its color or shape has changed dramatically, is a detailed examination prescribed to determine subsequent treatment.
Black moles attract special attention.
They may appear against the background of hormonal changes during pregnancy and lactation.
Most patients consider the appearance of a dark nevus as an increased risk of developing skin cancer.
However, not every black mole on the skin is melanoma; however, they require consultation with a doctor.
First, the specialist will evaluate the clinical change in the formation by viewing it with the naked eye.
The next step in diagnosis will be dermatoscopy.
Dermatoscopy is a diagnostic procedure.
Used to differentiate skin lesions.
Allows you to determine whether a black mole is of epidermal, vascular or melanocytic origin.
Dangerous clinical signs of a mole
Are black moles dangerous, what complications can they provoke?
If you discover a black mole, you should not panic immediately, but it is always better to consult a doctor.
Not all such nevi are malignant; the risk of transformation into an atypical formation does not exceed 5%.
It is imperative to visit a dermatologist if a black mole appears and the following clinical changes are observed:
- The previously discovered black nevus has increased in size (even a slight increase requires an in-person consultation with a specialist).
- The surface of the mole has changed its structure (looseness and bumpiness have appeared).
- Changes in the mole are accompanied by peeling, itching, and bleeding.
- A change in the color parameter of the nevus is observed: the mole abruptly began to change color, the red one became black, and a transition from a brown tint to a bluish tint was observed.
Normally, moles should not change.
Therefore, any dynamics should prompt a person to contact a specialist and undergo the necessary research.
It is strictly forbidden to try to remove a nevus on your own or use drugs intended for the elimination of papillomas and warts.
Trauma to a mole is a provoking factor in the development of malignancy—melanoma.
Melanoma is a type of skin cancer.
This is a very dangerous tumor with unpredictable behavior.
The disease can be quite easily prevented in the early stages, but treatment of later forms of melanoma is not very effective.
In a global comparison, malignant melanoma ranks third among all cancers.
Types of dangerous black moles
A black, convex and flat mole does not always indicate an ongoing malignant process.
The following will describe moles that are melanoma-dangerous.
In the presence of favorable factors, they can degenerate into malignant, cancerous tumors.
Black moles that are considered potentially dangerous:
- Dysplastic nevus (dysplastic nevus)
Dysplastic nevus (nevoid tumor) is a pigment-type formation.
Has the ability to transform into atypical.
The presence of such stains may indicate a direct danger, which is determined using the so-called ABCD rules.
These rules mean:
- asymmetry of education (A)
- irregular or worn border (B)
- presence of more than two colors (C)
- spot diameter more than 5 mm (D)
Nevoid tumor does not tend to be inherited.
It develops equally in both men and women, and is diagnosed in 6% of the world's population.
Such a mole has a flat surface, less often it can rise above the level of the skin epidermis.
There is no typical location for this type of nevus.
A preliminary diagnosis can be made based on dermatoscopy.
Confirmation of the type of formation is possible only through histology after surgical removal of the mole.
The main treatment is excision of the tumor, followed by monitoring the patient every 3-12 months.
Photographic documentation of skin malignancy with overview photographs and microscopic images is especially important.
In this way, even the smallest changes can be detected and dangerous moles can be removed on time.
Particular attention should be paid if a black mole appears on the labia majora.
Although this phenomenon is rare, such a nevus can be malignant.
- Nevus Yadassona-Tits (blue/blue nevus)
Benign, rarely acquired, dermal, melanocytic tumor.
Consists of mature, pigmented, dendritic, spindle cells and/or epithelioid melanocytes.
Acquired blue nevi can also appear in adulthood.
Because of their color, they are often mistaken for malignant melanoma.
Possible widespread distribution.
But they are more often observed on the arms, legs and head, in the hair growth area (in more than 60% of cases).
Visually, the blue nevus has a regular shape and its surface is smooth.
Such formations are usually single, up to 1 cm in diameter (in rare cases, 2-3 cm in size have been found).
Although blue nevus has this name, it can be either dark blue or black.
The provoking factor for malignancy is injury to the mole or attempts to independently excise the tumor.
If the mole is small in size and is not subject to injury or growth, removal is carried out only at the request of the patient.
Since nevus Yadassona-Tits does not often develop into melanoma, dermatologists choose a wait-and-see approach.
If a black mole grows, it is advisable to prescribe removal of the tumor.
After excision of the nevus, its histological examination is mandatory.
- Nevus Ota (phakomatosis Ota-Sato)
The characteristic localization of the formation is the face; it often develops in patients of Asian appearance.
As a rule, a nevus is located in the cheek area and can affect the mucous membrane of the eye.
Such a black mole on the face has another name - oculocutaneous melanosis.
The formation is classified as melanomatous, but rarely progresses to an atypical tumor.
When diagnosing nevus of Ota, regular monitoring by a dermatologist is recommended.
It is believed that phakomatoses are progressive in nature and have a hereditary predisposition.
Surgical intervention to excise phakomatosis is rarely prescribed when signs of malignancy are detected.
To eliminate the formation in order to eliminate a cosmetic defect, a laser procedure is recommended.
There is currently no definitive research that shows the underlying cause of Nevus of Ota.
Some researchers believe that the phenomenon may be caused by a genetic mutation.
Others argue that hormonal factors or radiation can cause the development of phakomatosis.
Although more research is needed to confirm both options.
People with oculocutaneous melanosis, which has spread to the mucous membrane of the eye, are more likely to develop glaucoma.
This is because melanocytes, which cause hyperpigmentation, block the flow of fluid in the eye, thereby increasing intraocular pressure.
- Border pigmented nevus (border pigmented nevus)
A border nevus is a pigmented spot no larger than 1 cm.
The color scheme can vary from gray to brown and black.
Most often this mole is brown-black.
Borderline nevus can develop on any part of the skin.
As a preventive measure, it is recommended to remove the formation using laser equipment.
Nevus is benign.
It rarely develops into cancer, but experts recommend an annual examination by a dermatologist.
- Giant pigmented nevus (congenital/giant pigmented nevus)
A congenital pigmented nevus is considered gigantic if its size reaches more than 20 cm in diameter.
Giant congenital nevi can occur in people of any racial background and in any area of the body.
They are the result of localized genetic changes in the fetus that lead to excessive growth of melanocytes, which are responsible for skin color.
Congenital nevus may not be accompanied by any other signs.
And it can occur together with itching or increased dryness of the skin.
The color may be fairly uniform or consist of several shades, including shades of brown, black, red or blue.
The predominant number of patients have a black and red mole.
In approximately 5-10% of cases, giant congenital nevus is associated with neurocutaneous melanocytosis (excess pigment cells in the brain or spinal cord).
Characterized by neurological symptoms.
Such a nevus has an increased risk of transition from a benign formation to a malignant melanoma.
If possible, treatment includes surgery to remove the nevus.
In other cases, other therapy, such as laser dermabrasion, may be performed.
In most cases, when there are no neurological problems, the prognosis is good.
But it is necessary that the formation be regularly examined by a doctor.
There are also other types of nevi, for example, you can find a dark brown mole with black spots. Such a neoplasm is highly likely to be benign.
Often defined as a pigmented nevus of the papillomatous type.
During pregnancy, there are cases when a black mole appears on the nipple.
Usually after childbirth, during the period of normalization of hormonal levels, the formation disappears.
But in a mandatory case, you will need to consult a doctor if the black mole hurts and changes.
Factors contributing to changes in nevus color
There are many reasons that influence the darkening or lightening of a mole. The leading factor is genetics. Neoplasms are often congenital. If relatives have malignant ones, then there is a high risk that the child will also develop melanoma.
Another reason why a mole becomes light is due to exposure to ultraviolet radiation. People with many moles on their body should not stay in the open sun for a long time or visit a solarium.
Regardless of the reason for the appearance of a nevus, any changes in it indicate the development of a certain process in the skin, and how dangerous it is should be determined by a doctor.
Changes in the color of a mole also occur for other reasons:
- Exposure to chemicals. If the nevus is constantly exposed to toxic agents, this leads to its modification and irritation.
- Damage. Banal scratches, scratches, wounds or insect bites lead to the degeneration of birthmarks. This causes inflammation of the skin and leads to the production of substances that increase cell growth.
- Hormonal imbalances. A nevus may acquire a heterogeneous consistency, change size and shade due to hormonal imbalance. Most often, dysfunction occurs in pregnant women, adolescents and people with diseases of the endocrine system.
Methods for diagnosing black moles
Melanocytic tumors are one of the main problems in diagnostic dermatopathology.
Because they include benign nevi, malignant melanomas and borderline cases.
Apart from the proportion of congenital lesions, most benign nevi occur in early or adulthood.
May eventually undergo regressive changes.
Particular care should be taken if moles and nevi become black.
Dermatoscopy of moles
The main diagnostic measure is dermatoscopy.
Dermatoscopy is a visual examination of the skin performed by dermatologists.
Diagnostics is of great importance for the prevention and early diagnosis of skin cancer.
The study uses a device known as a dermatoscope.
This is a small instrument that can magnify the area of skin being examined.
The device also has a light source.
There are many types of dermatoscopes.
In simpler models, the diagnostician looks directly into the magnifying glass.
If the device model is more modern, the dermatoscope can be connected to a computer.
This will allow you to enlarge the image the required number of times.
The image can be downloaded and saved on your computer for later use or for sending to other healthcare professionals.
Dermatoscopy is a non-invasive imaging technique.
Allows you to see submicroscopic structures invisible to the naked eye.
Diagnostics is used to study pigmented and amelanotic skin lesions.
Dermatoscopy is also called epiluminescence microscopy, incident light microscopy, and skin surface microscopy.
It is the most commonly used imaging method in dermatological practice.
Why does a mole have uneven coloring?
If you look closely at the moles on your body with a magnifying glass and a bright lamp, you can see interesting things. Not a single mole is 100% evenly colored. Some have darker areas in the center, others on the periphery, and others generally have lighter fragments.
You might unwittingly think that you have lived with melanoma all your life and only now noticed it...
Again, this is most likely not the case. Please look at this photo - there is a mole on it with 10x magnification:
Like any part of the human body, a mole does not have perfectly straight lines, identical proportions, or 100% symmetry. In the photo you can see how the pigment melanin, which is produced by the cells of the mole, forms a pigment network. It can be uniform by definition.
In a living organism that is constantly changing, such a situation is impossible in principle. Therefore, the pigment in some moles may be produced unequally, and our eye will see an uneven color.
Preparation for dermatoscopy of moles, disadvantages and advantages of the method
The analysis does not require special preparation from the patient, the study is absolutely painless.
The only relative disadvantage is that dermatoscopy subjectively evaluates the appearance of blackheads.
The result largely depends on the experience of the medical expert.
However, a modern dermatoscope with the ability to connect to a computer allows you to share the results with other doctors.
This increases the likelihood of correct diagnosis and accurate diagnosis.
Special computer programs are being developed that should facilitate the differentiation of benign and dangerous lesions of the epidermis.
Dermatoscopy is a simple, non-invasive and widely available diagnostic method.
Does not expose the patient to harmful radiation and provides valuable information for the evaluation of skin lesions of unknown origin.
However, the most informative method for diagnosing moles/nevi remains histopathology (histology).
Histopathological examination represents the gold standard for diagnosis in dermatology.
Dermatoscopy is an additional tool that allows you to assess the condition of the epidermis.
It should be taken into account that the effectiveness and information content of this method also depends on the specialist - the diagnostic accuracy of dermatoscopy correlates with the doctor’s experience.
Preventing and reducing the risk of melanomas
The postulates in the prevention of skin melanoma are: screening, limiting damaging factors, removing altered pigment formations.
Screening includes non-invasive diagnostic methods - dermatoscopy or epiluminescence microscopy annually, and for risk groups at least 2 times a year. Eluminescent microscopy is a non-invasive method for studying skin formations in a special immersion environment that can save a digital image, enter it into a database and track changes by comparing it with existing and subsequent images.
Primary prevention is to avoid the damaging effects of ultraviolet radiation, chemicals and other external factors. Secondary prevention is the removal of all moles suspicious for malignancy.
Tips that can prevent the development of melanoma are quite simple and effective. Will help reduce the risk of mole degeneration:
- wearing dark, thick clothing;
- eating vitamin D;
- removal of altered or injured moles.
The widespread use of screening and preventive measures will have a beneficial effect on the timely diagnosis and treatment of this dangerous disease.
How are black moles treated?
There are two treatment options - watchful waiting/observation of the patient by a dermatologist and removal/excision of the black mole.
In the first case, wait-and-see tactics are necessary when the chance of developing an atypical process is extremely low.
And the patient does not experience any discomfort from the mole, either emotional or physical.
Surgical removal is recommended when a black mole has a chance of degenerating into a malignant formation.
Or for aesthetic reasons, for example, when localized on the face, genitals, cheek.
The following removal methods can be used to remove a nevus:
- Surgical intervention. The tumor is completely removed. If during dermatological diagnosis it was revealed that the mole is accompanied by a malignant process, surgical intervention should consist of removing a certain edge of healthy tissue to prevent local recurrence.
- Cryosurgery. A procedure that uses a special instrument called a cryoprobe. The device is used to freeze and destroy abnormal tissue. The cryoprobe has a thin end that is cooled by substances such as liquid nitrogen and liquid nitrous oxide. Cryosurgery can be used to treat certain types of cancer and certain conditions that may progress to malignancy. This manipulation is also called cryoablation or cryotherapy. The technique can be used if there are black moles on the penis or in the perineal area.
- Radio wave excision. The procedure is based on the use of a special drug, most often “Surgitron”, which produces high-frequency radio waves. During the manipulation, the pathologically altered tissue is destroyed, while the surrounding epidermis is not injured. When removing moles, radio wave excision is often recommended. During the procedure, the vessel is blocked, so the risk of bleeding is almost zero. A black mole after this type of removal is not accompanied by the development of scar tissue, healing of the excision site occurs quickly.
- Laser removal. Excision of moles with a laser is considered the most effective method. The laser beam is able to penetrate deep into the epidermis, clearly along a given trajectory. This facilitates effective removal of the nevus without blood loss. The procedure is most often recommended for Ota phakomatosis. The procedure has proven itself in removing black moles on the lip and facial area.
Summary or briefly about the main thing:
A very small number of unevenly colored moles turn out to be melanoma. The likelihood of a malignant mole tends to zero if there are no other signs of melanoma. If doubts persist, be sure to see an oncologist and have a dermatoscopy done. If you are in doubt whether to go or not to go, it is better to go. Communication with a living doctor who is responsible for his every word, as a rule, dispels all fears.
If you still have questions, the following will help you:
- In-person appointment with an oncologist
(St. Petersburg) - Mole removal
with histology (St. Petersburg) - My online consultation (from anywhere in the world)