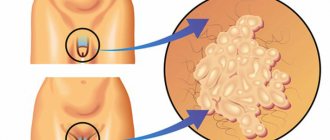
Papillomatosis is a common viral disease that is sexually transmitted in 80% of cases. These are rashes of benign formations on the surface of the skin and mucous membranes.
Growths that appear on the penis must be
treat in a timely manner. The danger is when they spread to the urinary canal, causing difficulty urinating. Enlarged and overgrown papillomas can interfere with normal sexual life.
| Human papillomavirus is a risk factor for the development of cancer. When the immune system is weakened, the pathogen is activated and neoplasms can degenerate into malignant ones. It is not the infection with the virus itself that is dangerous, but the reduction in the body’s protective functions. |
The essence of the problem
Genital warts are essentially genital warts and look like these “harmless” growths or may resemble overgrown cauliflower. This often leads to a neglectful attitude towards the problem. Papillomas do not cause any problems, they do not hurt, do not cause itching or other negative aspects. But warts on the genitals can be caused by human papillomavirus, which often provokes cancer of the penis and cervix. Condylomas pose a threat to both women and men, because this disease is sexually transmitted.
Human papillomavirus
The human papillomavirus (HPV) is very insidious and has more than a hundred varieties, many of which are unfavorable for humans. Cervical dysplasia, warts on the soles, genital warts are just a small part of the problems that can result from the spread of the human papilloma virus on the human skin and mucous membranes. The presence of a latent period during HPV infection makes it difficult to diagnose problems. Genital warts are a viral disease and are therefore transmitted through contact with a sick person. As a rule, this occurs during intimate relationships (genital, anal and oral sex), but domestic infection is also possible. There are statistical data about the acquisition of such a disease during childbirth by newborns. The male part of the population can “acquire” genital warts when the following HPV strains enter the body: 33, 18, 16, 11, 6.
Spread of infection
Do not be mistaken and think that HPV “rewards” only disadvantaged people and those belonging to a risk group - prostitutes, homosexuals, drug addicts, etc. Papillomavirus can spread in all segments of the population. The inexorability of statistics suggests that half of all people who are sexually active may have one or another type of HPV. Human papillomavirus scales are separated during sexual contact and invade new areas on the skin and mucous surfaces. Warts on the genitals should be a signal that you need to consult a doctor and protect yourself from the possibility of cancer.
Classification and examples of local GCS
| Group | Power of action | Examples |
| 1 | very strong | clobetasol 0.05% |
| 2 | strong | betamethasone ointment 0.05% |
| 3 | strong | triamcinolone ointment 0.1% |
| 4 | average | hydrocortisone 0.2% |
| 5 | average | triamcinolone cream 0.1% |
| 6 | small | betamethasone lotion 0.02% |
| GCS - glucocorticosteroids | ||
Localization location
Condylomas-warts in men can choose the following places:
- urethra;
- glans penis;
- body of the penis;
- bridle;
- scrotum;
- perianal area.
In some cases, warts can settle in the mouth, and this poses a threat to the transmission of the disease not only through sexual contact, but also through household contact. Genital warts usually affect the skin or mucous tissues. The source of risk for infection are areas of the skin with various microtraumas, which are not uncommon during sexual relations. Depending on sexual contact, the location of viruses may also change. Warts appear on the genitals during heterosexual relationships, near the anus during anal sex, in the partner’s mouth or on the partner’s penis during oral sex. Warts can spread either singly or in whole groups. The color of genital warts can vary from pale pink to dark brown. Often these skin neoplasms have a thin stalk and a wide base-head.
Surgeries for stage II penile tumors
For tumors of stage II and higher, as well as in the presence of metastases in the inguinal lymph nodes, an operation is required to remove regional lymph nodes - lymphadenectomy (lymphodissection).
During this operation, the inguinal and, in some cases, pelvic lymph nodes are removed. After removal of lymph nodes, complications such as prolonged lymphorrhea, lymphatic swelling of the scrotum and lower extremities (lymphedema), necrosis of skin flaps, and wound infection are often observed. The likelihood of complications depends on the extent of lymph node dissection.
Causes
Genital warts in men on the penis can appear due to the following reasons:
- Lack of protection during sexual intercourse.
- The presence of microcracks in the skin and mucous membranes in the genital area.
- Weakening of the immune system.
Men who are sexually active are the first to fall victim to HPV attacks. Warts on the penis are more likely to appear on the penis of members of the male population who are gay or who welcome promiscuous sexual relations without the use of protective equipment. You should not include only men who are into sexual excesses into the risk group. Respectable family men are also susceptible to infection. If HPV has entered a man’s body, this does not mean immediate infection. For the papillomavirus to begin its attack on a person, he “needs help.” An unfavorable factor in this case may be a weakened immune system. Vulnerability to the entry and spread of infection in the body increases if a man:
- became very cold or overheated;
- leads an unhealthy lifestyle (doesn’t get enough sleep, eats poorly, etc.);
- abuses smoking or alcohol;
- suffered from any serious illness;
- is in a constant state of stress.
Radiation therapy
Radiation therapy can be used as an independent treatment for penile cancer in the early stages.
Radiation therapy is possible only for tumors no larger than 4 cm. In this case, radiation therapy is an alternative to surgery, and in 80% of cases it allows to save the penis.
Circumcision is performed before radiation therapy, as radiation causes swelling and may cause the foreskin to shrink.
External beam radiotherapy
External beam radiation therapy is a method when the source of radioactive radiation is located at a distance from the surface of the human body.
The radiation session lasts several minutes; the process of setting up and preparing for radiation therapy takes a longer time.
Treatment is usually carried out 5 times a week for 6 weeks on an outpatient basis. The irradiation process itself is painless; symptoms may occur after irradiation (including in the long term), and are associated with complications of treatment.
Brachytherapy
Brachytherapy is a type of radiation therapy in which a radioactive source is placed inside the tumor. This treatment requires hospitalization in a hospital. IN
The penis is inserted into the penis in an operating room; hollow needles are inserted through which radioactive grains are injected, which are left for several days, after which they are removed.
The main disadvantage of radiation therapy is that, along with tumor cells, nearby healthy tissues are also damaged during the irradiation process. Therefore, after irradiation, changes in the irradiation area may be observed (swelling, redness, numbness of the skin), burning when urinating.
More serious complications such as penile necrosis, cicatricial narrowing or urethral fistulas are rare. In most cases, the appearance and function of the penis is restored within a few months.
If the tumor has spread to the lymph nodes, radiation therapy may be given after surgery to prevent recurrence of the disease. In addition, radiation therapy may be used in advanced cases to slow tumor growth or treat symptoms caused by the tumor.
Symptoms
The incubation period from the time HPV enters a man’s body until obvious manifestations of the disease can range from several weeks to eight months. Warts “scattered over different parts of the body (on the penis, scrotum, around the anus, on the tongue, etc.) can have different colors and sizes. Some condylomas pass from the solitary stage to the group stage, gradually spreading and merging into one monolith, which looks very much like a cauliflower inflorescence. Condylomas on the penis can cause discomfort to the patient; this is especially painful during sexual intercourse, because there is constant mechanical irritation. Frequent and painful urination is a symptom of condylomas in the urethral area. Typically, condylomas do not stop only on the genitals. And in advanced cases, they smoothly move to the groin and anus. The so-called “cockscombs” in the anus area can bleed and interfere with the natural and painless act of bowel movement.
How common is penile cancer?
Penile cancer is relatively rare. The incidence in different countries ranges from 0.1 to 8 cases per 100 thousand men. This variation in incidence is associated with social, cultural, and religious customs in different countries.
The lowest incidence is observed in countries where circumcision of newborns or children before puberty is common. In the Republic of Belarus, on average, 50 new cases of penile cancer are detected per year, and the incidence in 2010 was 0.4 per 100,000 men.
Treatment
You can get rid of condylomas on the penis in a radical way. Papillomas are removed using surgery or laser exposure. Excision of affected areas can be done using other methods:
- cryodestruction (using liquid nitrogen);
- thermocoagulation (cauterization of tumors with a special solution);
- applications with a solution of chemicals (condiline, solcoderm).
All these techniques contribute to the disappearance of condylomas and the subsequent healing of their localization sites. After this process, patients are prescribed supportive therapy - creams, ointments, gel medications. Acceleration of healing is not the only thing that occurs with the action of such medications. Another purpose of such drugs is the prevention of new formations. Each treatment and rehabilitation course is prescribed by the attending physician, taking into account the general condition of the patient, the location of the condylomas and the course of the disease.
Chemotherapy
Chemotherapy is the use of drugs that kill cancer cells. There are two types of chemotherapy used for penile cancer:
- Local chemotherapy . In this type of treatment, a chemotherapy drug (5-fluorouracil) is applied to the damaged area of the skin of the penis in the form of an ointment. This method of applying the drug does not allow it to affect tumor cells located deep in the skin. Therefore, this type of treatment can only be used for superficial forms of cancer (carcinoma in situ, stage 0).
- Systemic chemotherapy . In this type of treatment, chemotherapy is administered intravenously or taken orally in tablet form. Systemic chemotherapy for the treatment of penile cancer can be used after inguinal lymphadenectomy. In case of massive damage to the inguinal lymph nodes, chemotherapy can be used before surgery in order to reduce the volume of the tumor and subsequently undergo surgery to remove the lymph nodes.
Stages of the disease
Staging of penile cancer is carried out according to the international TNM classification, where T is a description of the primary tumor, N is the condition of regional lymph nodes, M is distant metastases.
| Stage | T | N | M |
| 0 | is – carcinoma in situ; a – non-invasive verrucous (warty) carcinoma without destructive infiltrative growth | 0 – no palpable or visually enlarged inguinal lymph nodes | 0 – absence of distant metastases |
| I | 1 – invasion into subepithelial connective tissue | 0 – no palpable or visually enlarged inguinal lymph nodes | 0 – absence of distant metastases |
| II | 1-2 – invasion into subepithelial connective tissue; ingrowth into the corpus spongiosum with or without invasion of the urethra | 1 – a mobile palpable enlarged inguinal lymph node is determined on one side | 0 – absence of distant metastases |
| 2 – ingrowth into the corpus spongiosum with or without invasion of the urethra | 0-1 – there are no palpable or visually enlarged inguinal lymph nodes; palpable mobile palpable enlarged inguinal lymph node on one side | 0 – absence of distant metastases | |
| III | 1-3 – invasion into subepithelial connective tissue; ingrowth into the corpus spongiosum with or without invasion of the urethra; ingrowth into the corpus cavernosum with or without invasion of the urethra | 2 – mobile palpable inguinal lymph nodes on both sides or multiple | 0 – absence of distant metastases |
| 3 – ingrowth into the corpus cavernosum with or without invasion of the urethra | 0-2 – there are no palpable or visually enlarged inguinal lymph nodes; a mobile palpable enlarged inguinal lymph node is palpated on one side; mobile palpable inguinal lymph nodes on both sides or multiple | 0 – absence of distant metastases | |
| IV | 4 – tumor spread to other surrounding structures | 0 – no palpable or visually enlarged inguinal lymph nodes | 0 – absence of distant metastases |
| 1-3 – invasion into subepithelial connective tissue; ingrowth into the corpus spongiosum with or without invasion of the urethra; ingrowth into the corpus cavernosum with or without invasion of the urethra | 3 – fixed conglomerate of inguinal lymph nodes or enlarged pelvic lymph nodes on one side or both sides | 0 – absence of distant metastases | |
| 1 – there are distant metastases |
For squamous cell carcinoma, the histopathological grade of differentiation (G) is also indicated:
- Gx – insufficient data to assess histological differentiation;
- G1 – well-differentiated tumor;
- G2 – moderately differentiated tumor;
- G3 – poorly differentiated or undifferentiated tumor.
Signs of Penis Cancer
The earliest symptom of penile cancer is a change in the condition of the skin on the head or shaft of the penis, which at first may appear as a small, inconspicuous lump. The area of changed skin may be flat or raised above its surface, have unchanged color or be pigmented. Gradually, as the lesion increases, the compaction loses its mobility, blisters and ulcerations may appear. Seals and ulcers can be painless or cause some discomfort (itching, burning, pain).
You should immediately consult a doctor at this stage. Attempts at self-treatment using traditional methods or on the advice of friends can lead to irreparable consequences.
As the neoplasm grows and develops, it infiltrates the underlying tissues and penetrates the corpus cavernosum and/or spongiosum. The primary tumor may bleed and have serous discharge. Infection of the disintegrating lesion leads to the appearance of an unpleasant odor, and there is a risk of developing urethral fistulas, soft tissue phlegmon, and sepsis. In advanced cases, self-amputation of the penis is not excluded.
Subsequently, regional lymph nodes are involved in the process, which enlarge, fuse together, forming conglomerates. The development of infectious lymphadenitis and purulent fistulas cannot be ruled out. As a result of impaired lymphatic drainage, elephantiasis may develop - severe swelling of one or both legs.
Further growth of the tumor and the appearance of metastases cause disruption of the general condition. Patients note weakness, fatigue, loss of appetite, and weight loss. Metastases in distant organs cause symptoms consistent with damage to these organs.
Diagnostics
The most accurate method for diagnosing penile cancer is a biopsy. The doctor removes the entire pathological tissue ( excisional biopsy ) or a fragment of it ( incisional biopsy ) and sends it to the laboratory for examination under a microscope. If cancer cells are found in the sample, the diagnosis leaves little doubt.
If enlarged lymph nodes are found, a biopsy may also be performed. The material for research is obtained using a needle or by surgically removing lymph nodes.
After penile cancer is diagnosed, the doctor may prescribe an ultrasound, computed tomography, MRI - these studies help assess how much the tumor has invaded neighboring tissues and spread to the lymph nodes.