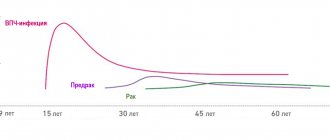
Today, HPV infection is one of the most common and important STIs (predominantly sexually transmitted infections), which affects most of the sexually active population of the planet. The peak incidence of HPV infection occurs at the age of 18-25 years and decreases after 30 years, when the incidence of dysplasia and cervical cancer increases significantly, the peak of which occurs at 45 years.
The International Center for Health Protection carries out diagnosis of infection with the human papillomavirus, as well as procedures for the prevention of infection with sexually transmitted infections after casual sexual intercourse. All services of the gynecological department and prices for them can be found in the relevant sections of the site.
At least 50% of sexually active adults are infected with one or more types of HPV, and in most cases, genital HPV infection in them is unrecognized, subclinical or asymptomatic. Genital HPV infection is highly contagious and is acquired during the first few sexual contacts; Infection with a single sexual contact occurs in approximately 60% of cases.
Risk factors for human papillomavirus infection
Recent studies have established that HPV is a necessary but not sufficient factor in cervical neoplasia. Risk cofactors for the development of the disease may be:
- disorders of cellular and humoral immunity
- unfavorable socio-economic status;
- sexual behavior;
- concomitant sexually transmitted diseases (herpes, chlamydia, trichomoniasis, gonorrhea, syphilis, etc.);
- hypo- and vitamin deficiencies;
- young age;
- smoking;
- pregnancy;
- vaginal dysbiosis.
The virus is also sometimes transmitted from mother to child, both in utero and during childbirth. In addition, pregnancy is a provoking factor for the manifestation and growth of neoplasms, as well as their transition to cancer. This occurs due to a decrease in immune defense and changes in hormonal levels.
Quite often we have to deal with a situation where a patient is diagnosed with human papillomavirus (HPV) of high oncogenic risk. As a rule, doctors immediately inform you that there is a risk of developing cervical cancer. Often quite aggressive treatment is immediately prescribed, a biopsy is performed, however, in general, what is actually happening and what the further prognosis is is not clearly explained. So, if you have been diagnosed with a high oncogenic risk human papillomavirus (HPV) by PCR, this does not mean that you need to panic. There is nothing serious about this find; it is just a reason to undergo an appropriate examination.
Cervical screening, aimed at identifying oncologically dangerous human papillomavirus infection and associated lesions of the cervix, continues to be a necessary component of healthcare and every woman should remember the need to “undergo” it.
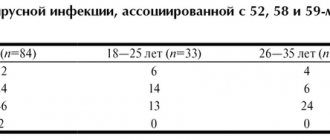
Identification of the causative agent of papillomavirus infection (Human Papillomavirus), during which the DNA of viruses in a sample of biomaterial is examined using the real-time polymerase chain reaction (RT-PCR) method. In this case, the presence of highly carcinogenic types of the virus (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58 and/or 59) is determined and their typing is performed.
Synonyms Russian
Human papilloma viruses of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 types), papilloma viruses of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 types), HPV of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 types).
English synonyms
Papillomavirus hominis, 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 types, DNA.
Research method
Real-time polymerase chain reaction.
What biomaterial can be used for research?
Rectal scraping, urogenital scraping.
General information about the study
Human papillomaviruses (HPV) are widespread, infect the epithelium of the skin and mucous membranes and have oncogenic potential. HPV is transmitted through close contact with infected epithelium, so the main routes of infection are sexual and household contact. It is possible to transmit HPV from an infected mother to her fetus. A person can be infected with several types of HPV.
Factors that provoke the development of HPV infection include: early onset of sexual activity, a large number of sexual partners, reduced immunity, the use of oral contraceptives, vitamin deficiencies, sexually transmitted infections, smoking and living in large cities.
The incubation period can last from 2 months to 2-10 years. A latent course of the disease is characteristic, in which there are no clinical manifestations, and colposcopic, cytological and histological examination reveals the norm. In 30% of cases, the virus can be cleared within 6-12 months. Diagnosis of latent HPV infection is carried out only by PCR.
During acute infection, benign formations occur, such as papillomas, warts, and condylomas. In children, papilloma viruses can lead to laryngeal papillomatosis. Damage to trophoblast cells by papilloma viruses is fraught with spontaneous abortion.
The combination of papillomavirus DNA with the cell gene leads to dysplasia/neoplasia (most often in the transition zone of the cervix). High oncogenic risk papillomaviruses include HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68. Infection with them leads to relatively benign bowenoid papulosis or squamous intraepithelial neoplasia of the cervix .
To identify HPV of high oncogenic risk, real-time polymerase chain reaction is mainly used, which makes it possible to find HPV DNA in the biomaterial under study and identify its individual types. The principle of the method is based on the amplification (multiple increase in the copy number) of a DNA section specific for a given pathogen.
What is the research used for?
- To detect papillomavirus infection of high oncogenic risk.
- To confirm/exclude persistence of a certain type of HPV.
- To assess the degree of carcinogenic risk in women with cervical epithelial dysplasia.
When is the study scheduled?
- For primary screening of cervical cancer (along with cytological examination) in women over 30 years of age.
- After surgical treatment of cervical intraepithelial neoplasia (CIN II) to identify/exclude the persistence of a certain type of HPV of high oncogenic risk (dynamic assessment).
- If the results of a cytological examination of gynecological smears are questionable.
What do the results mean?
Reference values: negative.
Reasons for a positive result
- Infection with papilloma virus.
Reasons for a negative result
- Absence of papillomavirus infection.
- Low levels of HPV in the blood.
Detection of HPV DNA in the test material indicates the presence of papillomavirus infection. If HPV DNA is not detected in the biomaterial under study, then the presence of papillomavirus infection is unlikely.
What should be done to prevent the development of cervical cancer?
1. Once a year, be sure to undergo an examination by a gynecologist with a mandatory examination of the cervix - colposcopy.
2. A simple examination of the cervix is not enough - certain tests must be done. That is, to answer two questions: do you have the human papillomavirus, and are there changes in the cells of the cervix that could potentially lead to the development of cervical cancer.
Most often, in ordinary clinics and laboratories they take a simple cytological smear and a PCR smear to determine the virus (that is, an analysis that simply answers the question whether this virus exists or not). These assays have several limitations that can significantly affect their accuracy.
Human papillomavirus infection (HPV) - symptoms and treatment
In 90% of cases, a healthy human immune system copes with human papillomavirus infection on its own within a period of six months to two years from the moment of infection, after which a complete recovery occurs with the disappearance of the virus from the body. In this case, intense lifelong immunity is not formed, that is, a person can become infected again.
In other cases, in the presence of predisposing factors, the disease takes on a chronic form, prone to a long latent course with periodic relapses and the possible development of severe complications.
From the moment the virus enters the body to the development of precancerous conditions and, especially, the appearance of cancer, quite a long time can pass, sometimes tens of years. Therefore, regular preventive examinations, timely detection and treatment of precancerous conditions are a very real and effective way to avoid the worst case scenario.[13] To this end, the World Health Organization recommends that all women over 30 years of age undergo not only a “routine” cytological examination during initial screening, but also a test for the presence of HPV.[10]
Regular visits to the gynecologist (if there are no complaints - once a year) with a Pap test allows you to timely detect the initial signs of dysplasia and take all necessary measures to prevent the progression of the process and its transition to cancer.
The use of barrier contraception methods, although not completely protects against infection, somewhat reduces its likelihood.
The main method of primary prevention of human papillomavirus infection is vaccination . [11] Modern vaccines are developed to protect against the most dangerous, highly oncogenic strains of HPV, responsible for 70-80% of cases of cervical cancer. A standard course of three vaccinations provides quite reliable protection.
It is advisable to vaccinate children (girls, and boys to curb the spread of infection) from 9-10 to 17 years old, as well as young women (18-25 years old) before engaging in sexual activity, since the vaccine prevents infection, but is not a means of treatment. developed infection. If the patient is already sexually active, then before vaccination she needs to undergo testing for the presence of human papillomavirus infection. However, even if one of the strains included in the vaccine is identified, vaccination can still be carried out, since this is not a contraindication.
HPV of high oncogenic risk, DIGENE - test
HPV of high oncogenic risk, DIGENE-test
- a clinical study that is prescribed for diagnosing cervical cancer and precancerous conditions in women. The infection is usually transmitted sexually; in some cases, the child may be infected with the virus from the mother during childbirth.
HPV infection causes laryngeal papillomatosis, genital warts, genital tumors, and cervical cancer.
Cervical cancer
- a malignant neoplasm in which the main cause of the disease has been established. Research shows that human papillomavirus DNA is found in almost all cases of precancerous conditions, as well as in cervical cancer. Infection with the papilloma virus also precedes squamous (scaly) intraepithelial dysplasia of the cervix.
Digene HPV test is a molecular technology from Digene, based on the detection of specific DNA fragments of the human papillomavirus using the “hybrid capture” method.
The test also allows you to differentiate between 2 groups of virus genotypes - high and low cancer risk. This test detects the presence of HPV DNA from a group of high-risk genotypes (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68).
This test is often used in research due to its reliability and ease of implementation. The sensitivity of the test in combination with the PAP test in detecting precancerous changes of the cervix and cervical cancer is much higher than cytology alone. This combination of tests is the standard for diagnosing cancer in women over 30 years of age. A positive result of the Digene HPV test in women under 30 years of age is a direct indication for repeat testing after 9 months, since in young women HPV infection can be transient.
With a positive Digene HPV test in women over 30, special prevention or treatment is necessary, since the patient has a high risk of cervical cancer. Modern treatment methods make it possible, in case of early detection, to sharply reduce the incidence of cervical cancer, and especially its incurable cases. After treatment, repeat testing is usually prescribed.
Indications:
- in combination with a cytological examination (PAP test) for the diagnosis of precancerous and cancerous changes in the cervix;
- screening examinations of women over 30 years of age (if the result is negative, the analysis is repeated at intervals of 3 years);
- monitoring the effectiveness of the therapy.
Preparation
No special preparation for the study is required to conduct the analysis.
Interpretation of results
Method of presenting the result: the result of determining the HPV DNA types of the high oncogenic risk group (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68) is presented in semi-quantitative form.
Units of measurement: conventional units.
Reference values:
If the result is below the threshold, the response “NOT DETECTED” is given. If the result is above the threshold, the answer is given in relative units. Relative units characterize the ratio of the obtained result to the threshold value.
1 relative unit corresponds to the threshold clinically significant HPV concentration (RLU 100,000 genocopies/ml).
For cases of newly diagnosed HPV - all positive results from 1 rel. units and higher, indicate the presence of HPV in clinically significant concentrations and the corresponding risks if it persists.
For cases of dynamic observation, during successful therapy there is a decrease in results in rel. units
Positively:
the presence of papillomavirus of the corresponding group of genotypes in epithelial samples. Consultation with a specialist is required to decide on further examination or treatment.
Negative:
No papillomavirus DNA associated with the risk of cervical cancer has been identified.