Dermatovenerologist
Khasanova
Alina Rashidovna
9 years experience
Make an appointment
HPV, also known as human papillomavirus, is not a single virus, but a whole group of them. They are transmitted from person to person (usually sexually) and become the cause of papillomas - benign formations. Some of these viruses are oncogenic, that is, they increase the risk of developing malignant tumors, for example, cervical cancer. But HPV is dangerous not only for women, but also for men, as well as for children.
Development and localization
To begin with, it is important to note that there are more than 600 strains of this virus. That is, there is not one diagnosis, one version of the consequences and one version of the manifestations. There are many different situations involving infection.
If the immune system is strong, it can easily cope with the virus on its own and within a few years “displace” it from the body. But at the same time, re-infection or illness with a different strain is also possible.
Papillomas and other symptoms of HPV in the form of formations that develop as a result of infection can appear in different places:
- on the skin anywhere;
- in the anogenital area;
- in the oral cavity, bronchi and upper respiratory tract;
- in the rectum, etc.
Formations can grow and form entire groups, or they can gradually dry out and disappear - it all depends on the specific situation.
Symptoms
At the initial stage, a person, as a rule, does not know about his disease, but is contagious to others. HPV very often does not manifest itself at all, but certain types can cause the growth of flat or pointed warts - papillomas or condylomas - on the skin and mucous membranes. Their appearance may occur several weeks or even months after infection.
Condylomas: treat or remove?
“If condylomas bother you cosmetically, bleed or get touched by clothing, they need to be treated. In other cases, you can leave it alone.”
Nosov Vladimir Borisovich
expert
Head of the Department of Obstetrics, Gynecology and Gynecological Oncology, European Medical Center (EMC), Gynecological Oncologist, Obstetrician-Gynecologist
The number and nature of tumors caused by HPV varies. In some patients, everything is limited to the appearance of 1-2 small warts, while in others, the affected area and the number of individual elements turn out to be quite large. Condylomas can be either single or multiple, and have different shapes from dome-shaped or filamentous to mushroom-shaped and plaque-shaped with a smooth or bumpy surface (Fig. 3). Some genital warts grow extensively, giving them some resemblance to cauliflower. The color of condylomas is usually white or flesh-colored, less often pink, red or brown.
Figure 3. Some types of HPV lead to the formation of condylomas (pointed warts) on the skin and mucous membranes, often in the genital area. Source
Genital warts are benign formations, they are not dangerous, but in many people they form complexes, cause increased anxiety and reduce the quality of sexual life.
In women, condylomas can form on the cervical mucosa. The growth of condylomas in the anus and urethra (or urethra) can make it difficult to go to the toilet. Sometimes condylomas can hurt or itch, and when injured, they can bleed.
HPV strains
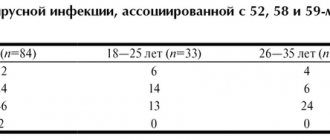
There are strains of the virus that have a high oncogenic potential. They are designated by numbers 16, 18, 39, 45, 56, 68, 73 and 82. There are also options with medium (26, 31, 33, 35, 51, 52, 53, 58 and 66) and low (6.11, 40, 42, 43, 44, 54, 61, 70, 72, 81) oncogenicity. Cervical cancer is most often associated with infection with strains 16 and 18, therefore, when such a virus is detected, maximum monitoring of the patient’s condition is required.
Important clarification! Highly oncogenic viruses detected in the body do not mean that a person will necessarily have cancer. This increases the risk of developing cancer, but is not a 100% determining cause. Moreover, oncology is usually preceded by so-called precancerous conditions. With regular monitoring, doctors have a very high chance of “catching” the disease at an early stage and preventing it from developing into cancer. And cancer itself at the first stage is treated quite successfully. If you have been diagnosed with a virus, do not panic - with proper control, this is not a death sentence for your health and life.
Types of papilloma virus
Research scientists have divided the types of HPV in women into those that are more likely to develop into cancer and those that are less likely. So-called “high-risk” HPV types are more likely to lead to cancer, while “low-risk” viruses rarely develop into cancer. High-risk sexually transmitted HPV types include the following types: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56-59, 68/69.
Low-risk types of papillomavirus do not cause cancer in humans. Warts or papillomas may grow weeks, months, or even years after exposure to infection, or may never appear. In fact, most people with low-risk HPV types never know they are infected without testing because they do not have any other symptoms.
Oncogenic HPV type
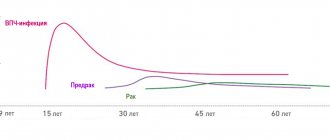
There are more than 40 types of HPV that can affect the genital area, but 9 of them are known to cause the majority of HPV-related cancers and diseases. Against their background, changes in the cervix that lead to cancer often develop over 10 or more years, and non-oncogenic types of HPV often resolve on their own within one or two years without causing cancer.
⚠ High-risk HPV types are 6, 11, 16, 18, 31, 33, 45, 52, 58 and some others. But these 9 main oncogenic types are responsible for approximately: ☛ 90% of cases of cervical cancer, ☛ 85% of anal cancer in men and women,* ☛ 90% of vulvar cancer cases,* ☛ 85% of vaginal cancer detections,* ☛ 90% of cases genital warts.
* - Not all cases of cancer of the vagina, external genitalia and anus are caused by high-risk HPV. About 70% to 75% of cases of vaginal cancer, 30% of cases of vulvar cancer, and 85% to 90% of cases of anal and rectal cancer are associated with the complex influence of individual risk factors in combination with these highly oncogenic types of HPV.
The main cause of HPV of the anus, including the high oncogenic type in a woman or man, is the practice of anal sex and the introduction of objects contaminated with viruses into the rectum (dildos, anal toys, etc.).
HOW IS THE PAPILLOMA VIRUS TRANSMITTED?
Most people get HPV through direct sexual contact in the vagina or rectum, or through oral sex. Since HPV is a skin-to-skin infection, sexual intercourse is not a requirement for infection. Up to 30% of cases of PVI transmission occur through contact at home. This may be one of the explanations for the presence of both genital warts and the detection of HPV in girls and virgin girls who have never had intimate contact.
In rare cases, a mother with HPV can pass the virus to her baby during childbirth. Often the virus is hidden in the body of the infected person. As a result, that person may unknowingly transmit HPV to their sexual partners. The virus is also more likely to be transmitted if there is an opening in the skin, such as a cut, abrasion or tear. These holes can be microscopic in size and not noticeable to the naked eye. Thus, any contact of these areas with a person who has the infection can transmit the virus.
HPV symptoms
The papillomavirus is one of the most common types of sexually transmitted infections (STIs). Almost all sexually active people will have HPV at some point in their lives, and they may not even know it. Most people never experience any symptoms of HPV. According to various estimates, up to 8 out of 10 cases of infection go away without treatment, often within two years. However, there are cases when the papilloma virus persists in the human body and symptoms appear.
Signs of infection depend on the type of HPV you were given. Some can cause genital warts, such as HPV types 6 and 11. Other types, such as HPV 16 and 18, do not cause warts or papillomas in women, but can lead to certain types of cancer.
Ⅰ WARTS.
They are a common symptom of HPV infection. They may appear weeks, months or even years after exposure to the virus. How warts look and where they are located on the body is determined by the type of HPV. Here is their list:
- Common warts. These rough, red bumps usually appear on the elbows, fingers, and hands. Common warts may be painful or bleed easily.
- Genital and anal warts. Condylomas and papillomas of intimate places, or genital warts, as their name indicates, most often appear near the anus and on the external genitalia of women and men. They may also appear near the anus, in the vagina, or on the cervix. These warts resemble irritated, cauliflower-like clumps, fringes, grapes, tiny raised bumps, or flat bruises. In men, genital warts most often affect the tip of the penis, the opening of the urethra, and the skin around the anus (especially in men who have anal sex). They usually have no symptoms and may be slightly itchy, but rarely cause pain. Genital condylomatosis is the most common manifestation of HPV infection in gynecology.
- Flat warts. They appear as darkened areas of skin with slightly raised flat tops. They can appear anywhere on the body.
- Plantar warts. These are thick, painful growths of skin on the soles of the feet. They are often mistaken for simple calluses. They may appear irritated, hard, and grainy (called a callus).
- HPV of the mouth and throat. The same types of HPV that can cause genital warts can also cause warts in the mouth and throat. This is called oral HPV. With this localization of HPV, symptoms may include: ear pain, hoarseness, sore throat that does not go away, difficulty swallowing, swollen lymph nodes.
Ⅱ HPV AND CANCER.
Certain types of HPV, most commonly 16, 18, 31, 33, 51 and 52, 45 and 49, can also lead to certain types of cancer. Cervical cancer is the most common HPV-related cancer. Symptoms of cervical cancer may include:
- irregular vaginal bleeding,
- unusual vaginal discharge,
- difficulty urinating or bowel movements,
- fatigue, weight loss.
Other types of cancer that are possible due to HPV include diseases of the vagina and vulva, cancer of the penis and scrotum, anus and rectum, and the back of the throat (oropharynx).
Table 1. “Manifestations of papillomavirus infection on the human body depending on the type of virus”
| Localization of education | Culprit |
| Skin warts | Types 2 and 7 |
| Plantar warts | Types 1, 2, 4 and 63 |
| Genital and anal papillomas | Type 6, 11, 42, 44, etc. |
| Cancer of the mouth, throat | Type 16, 33, 52 |
| Cervical tumors | Types 16, 18, 31, 45, etc. |
| Precancerous changes in the vulva | HPV 16, 18, 34, 39, 42, 55 |
HPV in girls, adolescents and virgins
As mentioned earlier, the spread of HPV in up to 80% of cases occurs through sexual contact. But this virus is also transmitted non-sexually. In children, it spreads from skin to skin through close contact. This leads to warts on the hands and face.
Genital papillomas are rare in childhood and are observed less frequently than in adults. However, there is an increase in the incidence of HPV in adolescents during puberty. In girls of primary and secondary school age, gynecologists often find warts in intimate places in the vaginal, vulvar and perianal area. Virgin girls get condylomas and HPV either as a result of surrogate sex without mechanical damage to the hymen, or sexual intercourse in the rectum or blowjob, as well as through contact and household contact.
Manifestations of HPV in children
Skin warts: At least 10 percent of children suffer from skin warts. These can be ordinary warts, plantar and flat. They are more common in girls than in boys. They are usually visible on the hands, fingers and nails. Genital warts, although rare in children, can appear as multi-colored cabbage-like growths in and around the genital and anal area. Genital condylomas are usually painless. Plantar warts are painful and cause discomfort.
In many children and adolescents, the infection remains latent and symptoms go unnoticed. It is believed that many women with cervical cancer were likely exposed to oncogenic types of HPV during adolescence or before the age of 20–25 years.
Photo of HPV
In the photographs below you can see what the mucous membrane and skin of the genitals affected by the papilloma virus look like. Some photos show manifestations of different types of HPV (high and low oncogenic risk) in women and men, taken under an electron microscope with high magnification.
Table No. 1.
HPV types
| Photo of HPV 16 | Photo of HPV 18 | Photo of HPV 6 |
| HPV 31/33 | HPV 42/45 | HPV 51/59 |
Table No. 2.
Photos of HPV in women
| HPV in the uterus | HPV on lip |
HPV DNA
International guidelines updated in 2014 recommend that girls undergo their first PAP and HPV testing at age 21, regardless of sexual activity.
After that, young women aged 21 to 29 should have a Pap smear every two years. Regular examination will help identify abnormal cells. They may signal cervical neoplasia or other problems associated with viral carriage.
Then, if previous test results are favorable, patients aged 30 to 65 years should be screened every three years with PAP and HPV tests simultaneously.
How to effectively detect human papillomavirus?
Donating DNA for HPV types is the main method for diagnosing this infection. This analysis can help identify the types of HPV that can cause cancer, and an expanded list of indicators will establish not only the genotype of the virus, but also its amount in the tissue. The gynecologist usually combines DNA testing for the papilloma virus with a Pap test. Next we will talk about these studies.
- "HPV DNA." The most common diagnostic method that allows one to detect the presence of infection even in a minimal sample of biological material. Most often, HPV DNA tests in women identify types 6, 16, 18, 31, 11, 33, 35, 39, 45, 51 and 52.
- “HPV DNA + PAP” liquid. Combined diagnosis of carriage of human papillomavirus infection and the degree of its possible influence on the epithelium of the cervix.
- "DNA for HPV types extended." The genotyping method allows you to both find out the type of HPV and determine its quantity. This has important prognostic significance in gynecology.
✔ You can donate HPV DNA to women and men in Moscow at reasonable prices from the specialists of our clinic. Gynecologists (for ♀) and a treatment room (for ♂) work daily, from 10-00, seven days a week. The clinic staff will tell you what types of HPV to test for. At the following link you can see all prices for analysis for the papilloma virus and advanced Digene tests.
Questions - answers on the topic
What types of HPV cause condylomas? There are 30-40 strains of the virus that specifically affect the genitals, but only some of them can cause genital warts in women and men. HPV types 6 and 11 cause the growth of condylomas and papillomas in the intimate area in 80% of cases.
What are the most dangerous types of HPV (for women)? Low-risk types cannot cause cervical cancer and are treatable. High-risk types 16 and 18 are dangerous because they can cause a woman to develop abnormal cells on her cervix, which often turn into cancer if left untreated.
What to do if a woman has HPV? During the examination, did the doctor find condylomas or did testing for the virus give a positive result? First of all, you need to get advice from a good gynecologist, a specialist in this pathology. After discussing the test data, conducting a colposcopy and a full examination to identify possible foci of condylomatosis, you can plan further tactics. In the future, after recovery from the virus and removal of condylomas, women are advised to “watchful waiting” with regular repeat HPV tests and colposcopy.
How to find out if you have HPV? Getting tested is the only and correct way to clarify your health status. A possible list of services and prices are presented in the table above. The status of a virgin does not prevent you from undergoing examination and knowing about the presence or absence of the human papillomavirus in the body.
How the virus is transmitted
To properly prevent human papillomavirus, you need to know the routes of infection. There are several transfer methods:
- sexual. Infection is also possible when using a condom - for example, during unprotected oral sex or during kissing;
- from mother to child;
- in domestic conditions, for example, if a person uses an infected person’s towel, razor or toothbrush;
- in public places such as a swimming pool, gym, bathhouse;
- autoinfection. This means that a person can “spread” the virus to other parts of the body himself.
The first route is most common, because the virus does not survive very well in the external environment.
It is also important to understand that the cause of human papillomavirus is weakened immunity - it is under this condition that infection is most likely. The situation is aggravated if the patient already has an STD, has bad habits, and is constantly under stress. Immunodeficiencies and various injuries to the skin and mucous membranes also contribute to the acquisition of the virus.
Women are most often infected. And strains with a high risk of cancer become more dangerous for them.
Cytomegalovirus
This is another member of the herpes virus family. It is very common and in most cases is in an inactive state in the body. Its activation occurs when the immune system is weakened, as well as during stressful situations. The virus is contained in all biological fluids of the infected person, and therefore can easily be transmitted through saliva during a kiss. Cytomegalovirus is especially dangerous for pregnant women, since when infected with it, the child often dies in utero. Surviving children who were infected in utero subsequently develop various abnormalities.
Signs
If HPV does not manifest itself in formations (warts, papillomas and condylomas), then without special tests the patient usually does not know that he is infected. In this case, the symptoms of the human papillomavirus are precisely the neoplasms - they can be accompanied by itching and discomfort.
If formations appear in the genital area, they can also manifest as painful and unpleasant sensations during or after sexual intercourse.
Are you experiencing symptoms of human papillomavirus?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Hepatitis A
This is an infectious disease that affects the liver. Hepatitis A in most cases ends in complete recovery. The disease does not become chronic. But the danger is that the disease is extremely contagious and a sick person can infect a huge number of people without even knowing that he is a carrier of the virus. The infection is most contagious in the last days of the incubation period, while there are no symptoms. In this case, infection can occur not only through a kiss, but even through objects touched by the patient.
Diagnostics
Diagnosis of human papillomavirus includes a doctor’s examination, enzyme-linked immunosorbent test, PCR diagnostics, as well as special tests to determine the oncogenicity of the strain. Women undergo a Pap test, that is, a cytological examination, for which a smear is taken from the vagina. A colposcopy is required - a thorough examination of the cervix using a special device.
Is HPV transmitted through kissing?
The papilloma virus is extremely rarely transmitted to a healthy person through a kiss. It accounts for on average no more than 10% of all cases of infection. It belongs to the contact-everyday category, but is not very common precisely because of the need for close, intimate communication with the carrier.
The type of kiss is also of great importance, since not all of them involve the impact of the saliva of an infected partner on the mucous membrane of a healthy person. Those who are fans of the “Inato”, “Sink”, “Sari”, “Enjoying the Bud” techniques are least likely to experience this.
The most dangerous is the classic French kiss with the tongue. In this case, he touches the partner's tongue and acts on his lips.
Treatment
Treatment of HPV does not imply the presence of any specific program that would completely destroy the pathogen. But patients are prescribed therapy that helps strengthen the immune system and self-heal. The assignments come down to several points:
- taking special medications. These are vitamins, antiviral medications and immunomodulators;
- removal of tumors. For this purpose, cryodestruction, laser, and electrocoagulation are used. Removal is possible using the classical surgical method;
- all kinds of strengthening of the immune system. A healthy lifestyle, giving up bad habits, giving up promiscuity - all this helps maintain immunity.
There are now vaccines for some types of HPV that are optimally used at 11-12 years of age (but can be used up to 26 years of age). Patients over 12 years of age are prescribed the vaccine if the doctor sees indications for this. The vaccine is not able to destroy the virus, but it can protect against other dangerous strains.
Questions and answers
How to get rid of the human papillomavirus forever?
It is impossible to get rid of it 100% using certain medical programs. But the virus can disappear from the body on its own, which does not eliminate the risk of re-infection.
How dangerous is the human papillomavirus?
The human papillomavirus is dangerous because some of its strains contribute to the development of cancer - in particular, cervical cancer.
If a virus is detected, will there definitely be cancer?
No, there is no absolute dependence in this case. We are talking about increasing risks, but this does not mean that cancer will definitely develop - people who have been diagnosed with the virus need to undergo regular examinations with doctors, and then the probable disease
Literature
- Nobel Prize winners in genetics. Electronic student library “Bibliofond”;
- Seeing viruses in cancer. Harald zur Hausen;
- The 2008 Nobel Prize in Physiology or Medicine was awarded for virological research;
- Belokoneva O. (2008). Nobel Prize in Physiology or Medicine 2008. Science and life. 11;
- Abbott A. (2008). Virus discoveries secure Nobel prize in medicine. Nature News;
- Young L. S. and Murray P. G. (2003). Epstein-Barr virus and oncogenesis: from latent genes to tumors. Oncogene. 22, 5108–5121;
- Gulley M. L. (2001). Molecular diagnosis of Epstein-Barr virus-related diseases. J. Mol. Diagn. 3, 1–10;
- Smith TF Herpes viruses. In: Clinical and pathogenic microbiology (2nd edition) /ed. by Howard BJ St.Louis: Mosby, 1994. P. 785-800;
- What are the dangers of the Epstein-Barr Virus? Website Herpes911.ru;
- Nikolsky I.S. (2006). Epstein-Barr virus infection: immunopathogenesis, clinical picture and treatment. Medical news. 9, 24–30;
- Faulkner GC, Krajewski AS, Crawford DH (2000). The ins and outs of EBV infection. Trends Microbiol. 8, 185-189;
- Kelly GL, Long HM, Stylianou J, Thomas WA, Leese A, Bell AI et al. (2009). An Epstein-Barr virus anti-apoptotic protein constitutively expressed in transformed cells and implicated in burkitt lymphomagenesis: the Wp/BHRF1 link. PLoS Pathog. 5 (3), e1000341;
- Kudin A.P. (2006). This “harmless” Epstein-Barr virus infection. Part 1. Characteristics of the pathogen. The immune system's response to the virus. Medical news. 7, 14–22;
- Boyle P. and Levin B. World Cancer Report 2008. Lyon: IARC-press, 2008. - 512 p.;
- Jaffe ES, Harris NL, Stein H, Campo E, Pileri SA, Swerdlow SH Introduction and overview of the classification of the lymphoid neoplasms. In: WHO Classification of Tumors of Haematopoietic ans Lymphoid Tissues / ed. by Swerdlow SH, Campo E. et al. Lyon: IARC-press, 2008. P. 158–166;
- Stein H. Hodgkin lymphoma - introduction. In: WHO Classification of Tumors of Haematopoietic ans Lymphoid Tissues / ed. by Swerdlow SH, Campo E. et al. Lyon: IARC-press, 2008. P. 322;
- Gurtsevich V.E. (2010). The role of the Epstein-Barr virus in human oncohematological diseases. Clinical oncohematology. 3, 222–234;
- Hjalgrim H. and Engels E. A. (2008). Infectious aetiology of Hodgkin and non-Hodgkin lymphomas: a review of the epidemiological evidence. J. Intern. Med. 264, 537–548;
- Damania B. (2007). DNA tumor viruses and human cancer. Trends Microbiol. 15, 38–44;
- Panagopoulos D., Victoratos P., Alexiou M., Kollias G., Mosialos G. (2004). Comparative analysis of signal transduction by CD40 and the Epstein-Barr virus oncoprotein LMP1 in vivo. J. Virol. 78 (23), 13253–13261;
- Smirnova K.V., Diduk S.V., Jabbarov S.M., Yakovleva L.S., Goncharova E.V., Shcherbak L.N. et al. (2010). Epstein-Barr virus: genetic variants of the LMP1 gene in patients with tumors of lymphoid and epithelial origin in Russia. Molecular medicine. 1, 46–53..