A newborn baby is a big responsibility for young parents. When visiting a pediatrician, parents usually ask a lot of questions. Especially if the child is the first. In my personal top list, feeding and colic take first place. Second - rashes!
In photographs on social networks, babies have clean, rosy cheeks and an angelic smile. And in life, redness, pimples, peeling and other unexpected things appear on the skin. Moms are not ready for this. They get scared and start looking for the reason. Neighbors advise you to follow a diet, grandmothers complain about “bad milk.” If you are unlucky, the doctor will scare you with allergies or prescribe tests, half of which will turn out to be unnecessary.
Let's try to figure out which skin problems in infants do not require treatment and are normal in infancy, and which do not. Let’s agree right away: any rash should be examined by a doctor in person. A diagnosis cannot be made from a photograph, because the doctor examines the elements of the rash, touches it by touch, and sometimes special diagnostic tests are needed. In doubtful cases, the pediatrician gives a referral to a dermatologist.
The information below is given so that young mothers stop being afraid of every pimple, understand conditions that do not require medical attention, and understand when to take their child to the pediatrician.
What does a newborn look like?
If the birth goes well, immediately after the birth of the newborn baby, the mother is placed on her stomach. His skin can be bright pink, or it can be pale, his hands and feet have a bluish tint. This scares young mothers if they have heard or read something about hypoxia and cyanosis before. But if the doctors in the delivery room are calm and do not provide resuscitation measures, then this is a variant of the norm. A healthy child can be like this in the first minutes of life. In addition, the newborn's body is covered with vernix - the baby looks as if it has been smeared with cream cheese. And this is also normal, although unattractive. Lubricant plays an important role in protecting the skin from germs, so the baby’s skin is only lightly blotted without being completely wiped.
5-10 minutes after birth, the newborn’s skin becomes bright pink, almost red. This is a normal condition - physiological erythema . The air pressure is less than the pressure of the fluid in which the baby was in utero. When the skin ceases to experience resistance, blood actively flows to it. The body gets used to the new form of life. Gradually, the blood vessels will narrow, and the skin will become its usual pink color by the end of the week in full-term babies and after 2-3 weeks in premature babies.
Marbled leather
During the first month of life, a baby's skin sometimes looks marbled. A uniform mesh pattern of white, purple, and reddish spots is the reaction of skin vessels to cold. Therefore, this phenomenon is most often noticed during swaddling. If the marbling is symmetrical and disappears when warmed, then there is no cause for concern. In other cases, it is worth discussing this symptom with your pediatrician so as not to miss the early diagnosis of diseases of the heart, lungs or skin itself.
Peeling
On the second or third day after birth, the newborn’s skin begins to peel off. Peeling is observed in everyone, but to varying degrees of severity. Most severe if the baby is post-term. The reason is the same restructuring of the body to exist in the air. The skin loses moisture, and the top layer gradually peels off. Physiological peeling does not require treatment and goes away on its own within a few days.
If the peeling is profuse and leads to deep cracks, the skin is lubricated with special moisturizers - emollients. In case of pronounced peeling, it is necessary to exclude congenital skin diseases such as ichthyosis, hyperkeratosis and others.
Erythema toxicum
By the second or third day of life, 70% of full-term newborns develop a small red rash on the skin. Rarely, this condition occurs in premature babies. First, spots appear, and within an hour a yellow bump 1-2 mm in size forms in the center. Elements of the rash are located on the face, torso, arms and legs, and can merge with each other. The cause of erythema toxicum is unknown, but the rash goes away without treatment in 1-7 days and is not dangerous.
If the clinical picture is atypical or other symptoms are present, the doctor will prescribe additional examination to rule out other causes of the rash, such as infection.
Newborn acne
20% of newborns develop a rash similar to teenage acne from the third week of life. Small pustules surrounded by a red halo. They are located on the face, head, chest, shoulders, and less often on the stomach. The condition is called “acne,” although in the literature the term “cephalic pustulosis” (from the words “cephalo” - head and “pustule” - abscess) or “neonatal pustulosis” is more often used. The main two reasons are the influence of maternal hormones during breastfeeding and the colonization of the skin by microorganisms. Elements of the rash resolve without treatment after 1-3 months. This condition is not dangerous, does not cause discomfort to the child and leads to independent recovery, so there is no need to prescribe medications. The exception is severe cases when the rash is profuse, leads to secondary infection or heals with the formation of scars.
Capillary hemangiomas, red birthmarks, otherwise called cavernous hemangiomas or cavernous hemangiomas - cavernomas, etc. “Salmon-colored spots” (“stork bites”) are just some of the varieties of red birthmarks. Learn further about the causes of their appearance and get acquainted with the appropriate treatment.
Skin conditions: red birthmarks
Congenital birthmarks are colored spots on the skin that are either present at birth or develop shortly after birth. Birthmarks can be characterized by many different colors in appearance, including brown, tan brown, black, light blue, pink, white, red or purple. Some birthmarks are just discolorations on the surface of the skin; others are structurally raised above the surface of the skin or extend into tissues beneath the skin.
What are the causes of birthmarks?
The causes of most birthmarks are unknown. Most birthmarks are not inherited.
There are many folk stories and myths about the causes of birthmarks, but none of these stories could explain the true causes of birthmarks.
Do birthmarks need to be treated?
Most birthmarks do not require any treatment. They often go away on their own as the child gets older.
However, some birthmarks may need treatment due to their specific location. For example, a raised birthmark near a child's eye can affect his or her ability to see.
In rare cases, birthmarks are associated with other conditions, such as growths on the liver, lungs, stomach, or intestines.
Types of birthmarks
There are two main categories of birthmarks - red birthmarks and pigmented birthmarks.
Red birthmarks are colored vascular (related to blood vessels) marks on the skin that develop before or shortly after birth. Pigmented birthmarks are marks on the skin that are present at birth. The color of the marks can range from brown or black to bluish or blue-gray. Read on to learn more about pigmented birthmarks.
Red birthmarks
Hemangioma (red birthmark) is the most common type of vascular birthmark. This spot is usually painless and harmless, and its cause is unknown. The color of a birthmark is conditional and occurs due to the extensive development of blood vessels in the area.
Types of hemangiomas include:
- Strawberry hemangiomas (also called strawberry mark, nevus vascularis, capillary hemangioma, hemangioma simplex) can appear anywhere on the body, but they are most common on the face, scalp, back, or chest . They are made up of small, tightly packed blood vessels. They may not be present at birth and may not develop until several weeks later. Strawberry hemangiomas usually grow quickly, remain a fixed size, and then “freeze” or fall off.
In most cases, strawberry hemangiomas disappear by the time the child is 9 years old. Some slight discoloration or wrinkling of the skin may, however, persist and remain in the area where the hemangioma was.
- Cavernous hemangiomas (also called angioma cavernosum or cavernoma) are similar to strawberry hemangiomas, but are located more deeply. They may appear and appear as a red and blue spongy mass of tissue filled with blood.
Some of these lesions may go away on their own, usually as the child approaches school age.
- Capillary hemangiomas are flat, purple to red birthmarks formed from dilated blood capillaries. These birthmarks are most often found on the face and can vary in size. Capillary hemangiomas are often permanent (if left untreated).
- "Salmon spots" (also called stork bites) appear in 30-50% of newborn babies.
These marks are small blood vessels (capillaries) that are visible through the skin. They are most common on the forehead, eyelids, upper lip, between the eyebrows and on the back of the neck. Often these marks disappear as the baby grows.
What are the symptoms of red birthmarks?
Symptoms of red birthmarks include:
- Skin marks that develop before or shortly after birth
- Red rashes or lesions on the skin
- Markings on the skin that resemble blood vessels
- Possible bleeding
How are red birthmarks diagnosed?
In most cases, a medical professional can diagnose a red birthmark based on the appearance of the skin alone.
Deeper birthmarks can be confirmed by tests such as MRI, ultrasound, CT scans or sections, or a biopsy.
What is the possible treatment for red birthmarks?
Many capillary birthmarks, such as salmon spots and strawberry hemangiomas, are temporary and do not require any special treatment.
For persistent skin blemishes, you can use special concealing cosmetics such as Covermark. Oral cortisone may shrink the size of a hemangioma if it is growing rapidly, obstructing the field of view, or if it is pressing on vital structures.
Capillary hemangiomas on the face at a young age can be treated with a yellow pulsed laser using dyes to improve results.
Other treatments for red birthmarks may include:
- Cold treatment - cryotherapy (freezing)
- Laser surgery
- Surgical removal
In some cases, birthmarks are not treated until the child reaches school age. However, birthmarks are treated earlier if they jeopardize vital functions, such as vision or breathing, or are of aesthetic “interest” in masking a skin defect.
Can red birthmarks be prevented?
There is currently no known way to prevent red birthmarks.
Website illustrations: © 2010 Thinkstock.
Infant acne
The same rash in children after three months of age is called infant acne. It persists as persistent acne of newborns or reappears at 2-3 months. It differs from newborn acne only in the age of the children and the duration of the rash. Self-resolution occurs within 6-12 months. Infantile acne may be a risk factor for acne during adolescence.
Prickly heat
Develops in children from the second week of life when overheated. The rash has different manifestations: small red spots, nodules, pustules or blisters in the thickness of the skin. Miliaria can occur on any part of the body: in the folds, on the face, scalp, torso, arms and legs. The cause of the rash is blockage of the sweat glands.
There are several factors contributing to this:
- high room temperature;
- increased body temperature in a child;
- thick clothing, non-breathable fabric, for example, an oilcloth mattress cover;
- lying in one position for a long time.
Treatment consists of general care:
- daily bathing without soap and other chemicals;
- using lighter and looser clothing;
- maintaining the air temperature in the room at 22-24 degrees C;
- ventilation.
When these conditions are met, prickly heat disappears within a few hours. The recommendations listed above also apply to prevention.
For walks outside, the child is dressed like an adult plus one layer of clothing. No need to re-wrap. There is also no need to wear a cap in warm weather.
During the cold season, undress your child during a long stay in a store, shopping center or other premises. While awake, place your baby on his stomach and hold him vertically in your arms to diversify his movements.
What needs to be done to still avoid diaper rash on the neck of a newborn?
- Monitor the temperature and humidity in the room where the child lives;
- Give your child air baths more often so that the baby’s skin can breathe;
- Choose high-quality fabrics when choosing clothes, and also pay attention to the collars on clothes. Not only should the collar not press, it is also important that the cutouts are deep and do not create occlusion;
- Wipe the natural folds of the baby’s skin more often, especially at high temperatures and humidity;
- Choose high-quality products for washing your child’s clothes, diapers and bedding;
- Give preference to hypoallergenic cosmetics for newborn skin care. Pay attention to the availability of clinical trials and dermatologist approval.
Diaper rash
A more serious skin reaction to overheating is diaper rash. Occurs in natural folds. It looks like redness, sometimes with weeping and erosion. With a long process, a bacterial or fungal infection may develop, then the surface of the affected skin is moist, bright red, with clear or purulent discharge. Prevention measures are the same as for prickly heat.
The skin in the folds is treated with powders. If normalizing the microclimate and caring for the newborn does not lead to a reduction in diaper rash, you should see a doctor. If complications occur, antibiotic therapy or topical steroid ointments may be needed.
Diaper dermatitis
The distinctive feature of this rash is that it appears only in the area under the diaper, other areas of the body remain clean. The reason is increased humidity and irritating feces.
The rash is found in the buttocks, thighs, lower abdomen in the form of individual elements or continuous areas of changed skin. The elements of the rash are varied: red spots, bumps, pustules or peeling.
To alleviate the condition, you need to change the diaper and wash the baby immediately after bowel movement. While changing clothes, you can arrange air baths, that is, leave the child to lie naked, you can cover it with a regular dry diaper. Lubricate the skin with a special diaper cream.
Change the diaper every 3 hours, even if it is only slightly full. More often when very full. If these measures are ineffective, you should consult a doctor. Local glucocorticoid agents may be needed.
Why do diaper rash appear on a baby's neck?
This phenomenon is provoked by a number of factors, such as:
- Lack of compliance with temperature standards;
- The child’s clothes are too hot/tight, do not allow air to pass through, and also rub the baby;
- Excessive use of skincare products that lead to acid imbalance and cause increased skin sensitivity (soaps, baby creams, oils, etc.);
- Irregular air baths;
- Untimely bathing of a newborn, especially in the summer (hot) period;
- Increased temperature due to ARVI.
All of the above points lead to increased moisture on the skin, and since during infancy there are natural folds in the neck area, irritation and redness of damp skin develop more actively there.
As for diaper rash in the neck area, the rash is most often caused by tight clothing in the collar area, which reduces the access of oxygen to these areas of the skin.
Seborrheic dermatitis
Appears in infants soon after birth and lasts up to a year. Yellow scales and peeling are most often located on the scalp and behind the ears, but can also be in other folds - axillary, elbow, inguinal. In everyday life they are called “milk crusts”. Because of its similarities to atopic dermatitis, seborrhea is sometimes considered a manifestation of allergies. The causes of this condition are not fully understood, but the relationship with allergies has not been identified.
Seborrhea goes away without treatment, in most cases in the first year of life. Unlike atopic dermatitis, the rash does not cause itching and does not cause discomfort to the child. If for the sake of aesthetics you want to get rid of seborrheic crusts, before bathing the baby’s head is lubricated with oil and then combed out with a soft comb.
In doubtful cases, when seborrhea is located on the body, it makes sense to consult a doctor to clarify the diagnosis.
Causes of birthmarks in newborns
Medicine does not know a clear answer about the reasons for the appearance of postpartum red spots in children. The defect appears as a pigmented area of skin that has:
- rich pink, red, brown color;
- smooth or rough surface;
- flat or protruding areas above the skin level;
- small or giant area;
- smooth or asymmetrical edges;
- different localization.
A detailed description of spots in children depends on their type, causes of occurrence, and the course of pregnancy. The main reasons for the appearance of birth pigmentation in newborns are:
- Hypoxia of blood vessels from compression during childbirth or late pregnancy:
- infectious diseases of the expectant mother;
- prematurity of the child.
If we are talking about vascular pink or red pigmented moles, they are most often localized on the child’s head: in the back of the head, on the chin, forehead, nose, bridge of the nose, cheeks, eyelids, and the baby’s upper lip. Brown pigmentation, called moles or nevi, can be located on any part of the body, just like hemangiomas. The formations are benign, but require careful observation by a specialist and subsequent removal, since they carry the risk of cells degenerating into melanoma and spoiling the appearance. Defects never go away on their own, unlike vascular birthmarks, which disappear on their own.
Atopic dermatitis
This is a chronic inflammatory skin disease. It occurs in 15% of children, of whom two thirds experience the first symptoms before one year of age, sometimes even in infancy. The rash appears on the face, torso, and extensor surfaces of the arms and legs. There may be redness, peeling, crusts, and when scratching, infection and the presence of pustules may occur. Elements of the rash itch and bother the child.
Only 30% of children have atopic dermatitis associated with food allergies. Therefore, a nursing mother does not always need a diet.
The cause of atopic dermatitis is increased skin permeability. For treatment, first of all, creams that restore barrier function are used. They are called emollients. There are quite a few brands that produce such products. The choice is based on personal preference. From a medical point of view, there is no advantage to any particular drug.
If you suspect atopic dermatitis, you need to see a doctor to clarify the diagnosis and receive recommendations for treatment. You can contact your pediatrician or dermatologist. If the diagnosis is confirmed, keep in mind: treatment will be long. It includes skin care and constant use of emollients; in more severe cases, hormonal ointments may be needed; for food allergies, a diet. It is important to understand that with strict implementation of the recommendations, stable long-term remission can be achieved.
How to get rid of birthmarks
Most birthmarks disappear on their own as the child grows older; this does not apply to nevi. A postpartum spot, if it is on the face and interferes with the normal development of the child, should be removed. It is necessary to get rid of pigmentation under sterile medical conditions with an experienced doctor so that the procedure is painless and has no consequences for the small patient.
Infrared radiation is actively used in cosmetology to remove postpartum spots. The principle of action of the rays is based on the ability to heat the area of influence and enhance regeneration processes in tissues.
Laser therapy is the most popular method of removing skin defects. The action of the technique is based on the gradual evaporation of the tissues of the pigmented area, allowing you to act only on the nevus, leaving healthy tissues untouched.
Surgical removal of birthmarks is used if the affected area is large and there is a suspicion of the presence of malignant cells in the skin. The disadvantage of the operation is a possible scar. An experienced doctor will reduce the risk of its occurrence to a minimum.
Mastocytosis
A rare disease that can appear at an early age, sometimes even from birth. Outwardly, it resembles allergic urticaria, but spots and blisters last longer, and when the exacerbation subsides, pigmentation remains. A typical diagnostic test is the appearance of blisters on the skin due to mechanical irritation of areas of pigmentation.
Treatment for childhood forms of the disease is not required; recovery occurs spontaneously within several months, sometimes several years. If itching is present, antihistamines are used.
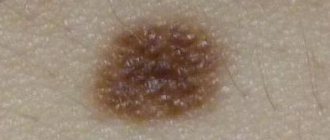
Infantile hemangioma
Hemangioma is a benign tumor of endothelial cells (endothelium is the inner lining of blood vessels). It may be congenital or appear at 1-2 weeks of life. Superficial hemangiomas are bright red and protrude above the surface of the skin. Deep - blue-purple, sometimes warm to the touch. The element size ranges from a few millimeters to an entire anatomical area (hand, buttock, etc.). In the first 5-6 months, the hemangioma may increase in size and become brighter, then the growth ends and spontaneous regression begins.
Up to 90% of hemangiomas can resolve without treatment.
In this regard, surgical treatment is no longer used routinely. The child is observed by a pediatrician and a surgeon; if hemangiomas are located on the face and neck, in the genital area and near large vessels, conservative treatment is prescribed. The operation is indicated only if it is ineffective.
Types and features of localization
Classification of birthmarks will allow you to better understand the nature of pigmentation: red and pigmented birthmarks. If the former are characterized by hypoxia or vascular hyperplasia, the latter appear due to the accumulation of melanocytes (cells that synthesize melanin) in a limited area.
Birth red moles are associated with deformation of blood vessels during childbirth due to mechanical compression of the baby's head. The localization of formations speaks in favor of this theory. Depending on the presentation of the fetus, the mother’s pelvic bones put pressure on the baby’s occipital region or face, which is why the vessels in the places of compression experience hypoxia and turn red. If the neck and back of the head are compressed, the formations are called a stork bite, if on the face - an angel's kiss, in some cases the formations are found in the lumbar region, where they reach 4 cm in size. The marks have clear edges, irregular shape, pronounced color from pink to bright red , do not rise above the surface of the skin, do not itch, and do not make themselves known in any way, except for their non-standard coloring. Over time, vascular moles disappear, becoming pale, but maintaining their outline until they disappear completely. There is no heredity factor.
Another type of vascular spots spreads throughout the newborn’s body, but is much less common than spots on the head. The formations are caused by the same reasons as the bite of a stork, however, their structure is caused not by hypoxia, but by hyperplasia - the proliferation of vascular tissue in certain areas. The phenomena are called salmon spots, have a less bright color, and a hereditary factor can be traced in their formation. Vascular hyperplasia tends to spread in the first month of a baby’s life and requires supervision by specialists. The color of the formation may change to purple and bluish; they rise above healthy skin. The disappearance of salmon nevi is characterized by a reduction in area rather than fading, which distinguishes them from stork bites.
Hemangiomas on the body of a newborn are red dots of small diameter located throughout the body. The formations are a proliferation of vascular nodules, do not cause discomfort to the baby, fade over time, are flat and protruding, the surface is smooth. Hemangiomas are removed when they are on the face. The treatment method is chosen by the doctor.
There are 2 main types of hemangiomas: simple (strawberry) and cavernous (cavernous). Strawberry is a convex nodule of vessels the color of ripe strawberries. By the age of 10 they go away on their own. The quantity is of concern: if a child has more than 3 such formations, the patient is prescribed an ultrasound of the internal organs in order to exclude pathologies. Cavernous hemangioma looks like spongy tissue filled with blood, does not have clearly defined boundaries, deforms when pressed, and then returns to its previous appearance. In the first six months, cavernous hemangioma grows, increasing in size, and disappears by puberty. During the period of growth growth, the child receives medical advice from vaccinations in order to differentiate the possible consequences of education and vaccination.
Port-wine stains/flaming nevus are dense formations on a child’s skin with intense, uniform coloration over the entire area. Features of the defect are a rich purple-red color, elevation above healthy tissues, the formation increases in size as the child grows, and is most often localized on the face, although it is also found in other parts of the body. A flaming nevus does not become inflamed, does not secrete fluid, does not itch or flake off, and over time vascular nodules form on it. Doctors monitor the connection between the fiery spot and disturbances in the functioning of the brain, and recommend consulting with a neurologist and ophthalmologist to rule out possible defects in eye development. Since flaming spots cause psychological discomfort and cause complexes, they can be easily removed using modern hardware techniques.
Non-vascular formations in infancy - nevi, appear in places where melanocytes accumulate; a failure in their uniform distribution in the skin occurs in utero; it is impossible to influence the process. The color of moles ranges from flesh-colored and light brown for raised ones to black for flat ones.
Vascular abnormalities
Congenital anomalies of vascular structure are varied
- A simple nevus is a capillary anomaly. It appears as a pale pink spot or several small spots. The common name “stork bite” or “angel kiss” arose due to its location on the back of the neck and head, on the forehead, bridge of the nose and upper eyelids. The spots fade by the age of two, but can appear when crying or physical activity. No treatment required.
- Port wine stain or flaming nevus. A dark red spot that looks like a hemangioma. It may be one of the manifestations of pathological syndromes. Lasts for a long time. Treatment is not necessary, but can be done if the spot creates a cosmetic defect.
- Venous anomaly - blue-violet painful nodules under the skin. They can also masquerade as a hemangioma. Occur alone or in combination with other anomalies. The danger lies in the possibility of thrombosis of the altered veins. Treatment consists of wearing compression clothing and using aspirin to prevent blood clots. Surgical excision is possible.
- More rare lymphatic, arteriovenous and combined anomalies are found as part of various pathological syndromes.
Baby's red cheeks: should I worry?
Children's skin is incredibly sensitive to both environmental influences and the child's general well-being. Therefore, in some cases, red cheeks are a reason to think about the baby’s health.
Response to environmental influences
Red spots on a child's cheeks may be a banal reaction to cold or heat. The process of heat exchange in infants does not proceed the same way as in adults, so red cheeks can signal overheating or, conversely, too close contact with frost. In the first case, the baby must be immediately cooled, and in the second, apply protective cream to exposed skin 20 minutes before going outside.
Manifestation of allergies
Have your baby’s cheeks turned red, started to peel and even itch? This may be a manifestation of an allergy - food, household chemicals, dust or animals. Often the redness of the cheeks in this case is also accompanied by the appearance of redness in the area of the shoulders, forearms and groin. Be sure to consult a doctor to find out why your child has red cheeks and to eliminate the allergen from the environment that causes such a reaction in the baby.
Atopic dermatitis
Babies suffering from atopic dermatitis often experience redness, which is accompanied by severe dryness, itching and even crusts. As a rule, there are pockets of dermatitis on other parts of the body, and dryness and redness do not go away with the use of conventional moisturizing creams. Atopic dermatitis is a serious reason to see a doctor.
Enzyme deficiency
Enzyme deficiency usually manifests itself in children in the first year of life. One of its symptoms is redness of the baby’s cheeks (in this case, the child may not gain weight). When a baby eats more than his body can absorb, the unprocessed protein causes an allergic reaction and, as a result, reddening of the cheeks. In this case, you should carefully monitor the amount of food offered to the child, especially when artificial feeding.
Teeth cutting
Redness of the cheeks and swelling of the gums are sure signs that a new tooth will soon appear. At this time, the baby’s behavior may also change: he rubs his ears and cheeks, becomes irritable, and sleeps restlessly. You can alleviate the baby’s condition with special teethers or a soothing gel (as prescribed by a doctor).
Viral or infectious diseases
Red spots on a child’s cheeks are far from the only symptom that parents should pay attention to. For example, with ARVI this can be a fever, cough and runny nose, and with infantile roseola - loose stools, fever and a rash (first on the cheeks, and later throughout the body from the face to the feet). Red cheeks combined with pale lips and the tip of the nose can also be a sign of pneumonia. In all these cases, it is necessary to contact your pediatrician as soon as possible.
Everything is fine!
The most common cause of red cheeks in a child is an allergic reaction. But it is quite possible that the child simply spent an active day, moved and laughed a lot, or took a long walk in the fresh air. Such a blush is a joy for the mother and a sign of the baby’s excellent health!