A drug allergy is an acute or chronic allergic reaction to a drug. In an allergic reaction, the immune system, which fights infection and disease, reacts to the drug. This reaction can cause symptoms such as rash, itching, malaise and difficulty breathing. True drug allergies are rare. Less than 5 - 10% of negative reactions to medications are caused by a true drug allergy. The rest is the side effects of the drug. At the same time, it is important to know if you are allergic to certain medications and what to do about it.
People with drug allergies may experience symptoms regardless of whether their medication comes in liquid, tablet, or injection form. If a person is unsure about their symptoms and which medications are safe to take, they should temporarily stop all medications and consult an allergist.
What is an allergy
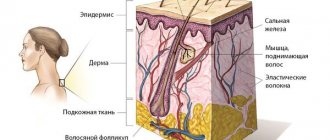
The immune system helps protect the human body from disease. It is created evolutionarily to combat foreign invaders such as viruses, bacteria, parasites and other dangerous substances. In a drug allergy, the immune system mistakes a drug that enters your body for one of these invaders. In response to what it perceives as a threat, the immune system begins to produce antibodies. These are special proteins that are programmed to attack the invader. In this case, they attack the drug.
This immune response leads to increased inflammation, which can cause symptoms such as rash, swelling, redness, or difficulty breathing. An immune response may occur when the drug is first taken, or it may only occur after a person has taken it many times without problems for a while.
Why are medications increasingly causing allergies?
Pharmaceutical companies produce a large number of new drugs. Once on the market, medications are taken uncontrollably by patients. Once in the body, they can interact with other substances, such as flavorings, dyes, and food preservatives. It is difficult to predict how the body will react to this dangerous cocktail next time.
Cross-allergy has become a big problem recently. Simply put, the increased sensitivity of the immune system to some chemical irritants can spread to others that are similar in structure. For example, the molecules of penicillin and cephalosporin, novocaine and sulfonamide drugs are similar. Therefore, if you are allergic to penicillin, it is also quite possible to have an allergy to cephalosporin.
Causes of drug allergies in adults
In principle, the cause of an allergy can be any drug that is applied to the skin or mucous membranes (taken topically), used orally in various forms (tablets, capsules, syrups or solutions, powders), injected (subcutaneously, intravenously or intramuscularly) .
A drug allergy occurs when the immune system mistakenly identifies a drug as a harmful substance, such as a virus or bacteria. Once your immune system detects a drug as harmful, it produces antibodies specific to that drug. This may happen when you first take the medicine, but sometimes an allergy does not develop until repeated exposure occurs.
The next time you take the drug, these specific antibodies signal the drug and direct the immune system towards it. The chemicals released from this activity cause the signs and symptoms associated with an allergic reaction.
However, you may not be aware of your first exposure to the drug. Some evidence suggests that trace amounts of a drug in food, such as antibiotics, may be enough to cause the immune system to create antibodies to it.
Allergic reactions may be the result of a slightly different process. Researchers believe that some drugs may bind directly to a certain type of white blood cell from the immune system called T lymphocytes. This event triggers the release of chemicals that can cause an allergic reaction when the drug is first taken.
Causes
The most common cause of allergies is penicillin. During the first course, an allergic reaction may appear after 5-6 or even 20-50 days, and during the second course, immediately after the injection. Even imported meat products containing antibiotics can cause drug allergies.
Also, other antibiotics, sulfonamides, antihistamines, antipyretic drugs, and drugs containing aspirin can often cause the disease.
The increase in cases of drug allergies is associated with uncontrolled use of medications, mainly without a doctor’s prescription.
In addition, prolonged use of one medication can lead to the development of an allergic reaction to other drugs that were previously tolerated normally.
Medicines that commonly cause allergies
Although any medicine can cause an allergic reaction, some medications are more commonly associated with allergies:
- antibiotics such as penicillin;
- pain relievers such as aspirin, ibuprofen, and naproxen sodium;
- chemotherapy drugs for cancer treatment;
- medications for autoimmune diseases such as rheumatoid arthritis;
- antibiotics containing sulfonamides (sulfonamide drugs);
- anticonvulsants;
- means for X-ray contrast diagnostics (especially iodine preparations).
Non-allergic reactions to medications
Sometimes a drug reaction can cause signs and symptoms much the same as a drug allergy, but the drug reaction is not caused by immune system activity. This condition is called nonallergic hypersensitivity reaction or pseudoallergic drug reaction.
Medications that are more commonly associated with this condition include:
- Aspirin;
- dyes used in imaging (radiocontrast media);
- opiates for pain management;
- local anesthetics.
INTRODUCTION
All data on the prevalence of adverse reactions to drugs must be taken into account.
Adverse drug effects are thought to account for 5% of hospitalizations and occur in 10–15% of hospitalized patients [1, 2]. Drug allergies often occur in patients over 50 years of age and occur in women in 63–70% of cases. Drug allergies are observed in 20–80% of HIV-infected patients and in 30% of patients with cystic fibrosis [4]. Allergy to β-lactam antibiotics is often observed [5, 6]. It is assumed that IgE-mediated allergy to antibiotics is observed in 2–3% of the total population [7] and 5% of the population to penicillin and other β-lactam drugs [8, 9]. Skin manifestations, including acute urticaria, are common in patients treated with amoxicillin and ampicillin [10]. Anaphylactic shock is rare, occurring on average in 0.004–0.015% of cases, and approximately 10% of them are fatal.
There is a trend towards an increase in drug allergies to antibiotics. Analysis of antibiotic consumption in European countries is determined by the daily dose of antibiotic (DDD) or DDD per 1000 inhabitants per day. The results of statistical analysis show that the highest consumption of antibiotics occurs in the countries of Southern and Eastern Europe [12 – 14]. Frequent use of antibiotics is the main factor that leads to the development of antibiotic resistance in microorganisms. Greece is a country with one of the highest rates of DDD and also has high bacterial resistance to antibiotics [15].
Many researchers have shown a connection between the use of antibiotics in children and immune system disorders, as well as the occurrence of atopic diseases. Studies have shown that taking antibiotics during pregnancy increases the risk of developing asthma and atopic dermatitis in children [16, 17]. Other studies show that the use of antibiotics by children in the first year of life predisposes to the development of asthma and allergies in children at 6–7 years of age [18, 19].
VARIETY OF ALLERGIC REACTIONS CAUSED BY DRUGS
Adverse drug reactions can be divided into immunological and non-immunological. Non-immunological manifestations include: intolerance reaction, pseudoallergy, idiosyncrasy and, as a rule, they are associated with the use of NSAIDs, radiocontrast agents, opiates and local anesthetics. Allergic reactions are more unpredictable, and the immune system plays an important role in their pathogenesis [20].
An allergy to medications manifests itself as an organ or systemic reaction. Examples of systemic allergic reactions are anaphylactic shock, serum sickness, various types of rash with eosinophilia and others (DRESS, drug rash with eosinophilia and systemic manifestations).
Frequent and prolonged use of drugs, inadequate cleaning during production, addition of additives and preservatives contribute to the development of allergies. Patients with atopy do not experience a high incidence of drug allergies, but when anaphylactic shock develops, its course is more severe compared to other patients [5, 6]. Anaphylactic shock is most often observed after taking aspirin, NSAIDs, β-lactam antibiotics and administration of contrast agents [20].
Drug allergies manifest themselves with various symptoms according to Gell-Coombs (Table 1), immediate reactions involving IgE are more severe.
MEDICINES AS ALLERGENS
Macromolecular substances such as hormones, enzymes or serums are the most common allergens. Only a few drugs (peptides) are full-fledged allergens. Most drugs are small molecules (haptens) and cannot induce an immune response on their own. These particles, when attached to proteins, acquire the properties of allergens. Often, the products of drug transformation are reactive and are called pro-haptens [7, 23]. Examples of full-fledged allergens are hormones, vaccines and serums. Other haptens are β-lactam antibiotics, and pro-haptens are sulfonamides, phenacetin, phenytoin [23].
Β – LACTAM ANTIBIOTICS – THE MOST COMMON ALLERGENS AMONG MEDICINES
Most drug allergies are induced by β-lactam antibiotics. The bactericidal effect of these drugs is associated with inhibition of bacterial cell wall synthesis. This action is based on the inhibition of transpeptidases necessary for the synthesis of peptidoglycan, which is the main component of the bacterial cell wall. The absence of peptidoglycan during the cell cycle leads to bacterial lysis, hence β-lactam antibiotics act during cell division. Antibiotics of this group are not effective against bacteria without a cell wall (mycoplasma, intracellular legionella, chlamydia) [24].
β-lactam drugs include penicillins, cephalosporins, carbapenems, and monobactams. According to numerous studies, this group of antibiotics is the most used in medicine. This is due to the effectiveness and safety of use, a large range of drugs, despite the fact that taking these drugs in 10–15% of cases is accompanied by allergies [24].
Allergic manifestations of β-lactam antibiotics are associated with their chemical structure. The hapten is an unstable β-lactam ring to which proteins attach, and benzylpenicilloyl-polylysine (the main antigenic determinant) is formed, which is responsible for the manifestation of an allergic reaction. Other small antigenic determinants are benzylpenicillin, benzylpenicilloate and benzylpenylloate. Clinical studies show that they are less responsible for the development of the anaphylaxis reaction. Major and minor antigenic determinants are responsible for the development of IgE-mediated allergies and the occurrence of cross-reactions of various penicillins. The side chains of the β-lactam ring are responsible for the development of IgE-independent allergies and the occurrence of cross-reactions to β-lactam antibiotics [23, 25].
In case of allergy to β-lactam drugs, cross-reactions to penicillin, ampicillin and amoxicillin are often observed. Skin tests often do not confirm an allergic reaction, even if the patient has symptoms after taking the drug. Patients who experience allergic symptoms immediately after taking amoxicillin are also at high risk of hypersensitivity to penicillin and ampicillin [26].
Despite the numerous side effects associated with the use of β-lactam antibiotics, this group of drugs is often used to treat bacterial infections.
SYMPTOMS OF ALLERGIES TO DRUGS
Skin manifestations of drug allergies can occur to almost any drug administered orally [27, 28], as well as with topical use of drugs containing salicylic acid [29], macrodides [30] and other active components [31]. One of the most common skin manifestations is a maculopapular rash. It is known that maculopapular rash occurs in 75% of cases [10]. A maculopapular rash can appear with the use of almost any drug, even some time after its use. Clinically characterized by roseola or morbilliform rashes [32 – 34]. The rash can be represented by spots, erythema and papules, often located symmetrically. Most often, the rashes are located on the trunk and limbs, accompanied by fever, eosinophilia and severe skin itching [32, 35]. The rashes tend to spread and infiltrate. The rash disappears a few days after discontinuation of the drug, and is accompanied by exfoliation of the epidermis, after which redness remains on the skin [31, 36]. Drugs that cause such rashes include NSAIDs, ACE inhibitors, barbiturates, β-blockers [7, 37, 38] and antibiotics used to treat respiratory diseases [31, 36].
The most severe manifestation of drug allergy is an acute generalized eczematous-pustular rash [37]. This symptom appears several hours after taking the drugs [39, 40], and is often accompanied by fever. The rashes are localized first on the face, then on the skin of the torso and limbs. Generalized pustular rashes are a rare occurrence and are associated with the presence of HLA-B51, HLA-DR11 and HLA-D9 antigens [41]. Rashes often occur after taking antibiotics (β-lactams, tetracyclines, macrolides) and other drugs (furasemide, NSAIDs) [40, 41].
Another cutaneous manifestation is drug-induced urticaria. Most often, its occurrence is associated with the use of penicillin and sulfonamides [11]. Urticaria may be accompanied by anaphylaxis or serum sickness [37]. After taking aspirin, NSAIDs, and contrast agents, pseudoallergic urticaria most often occurs, but the rashes are the same as in the case of allergic urticaria [11]. Urticaria is accompanied by itchy skin. Symptoms usually occur within 36 hours of taking the drug, although if the drug is used repeatedly, symptoms may occur within a few minutes. Hives often disappear quickly, usually within a few hours.
The clinical picture of drug allergies is characterized by polymorphism. Different drugs can cause identical rashes, but allergies to the same drugs can be accompanied by different clinical presentations [41]. Drug-induced skin lesions are usually mild and disappear on their own after discontinuation of the drug. Severe skin lesions include skin necrosis, epidermolysis bullosa, swelling of the face and tongue, and may also be accompanied by systemic reactions [20, 27].
The most dangerous drug-induced systemic reaction, which develops within a few minutes after repeated administration of the drug [32], less often after the first use [42], is anaphylactic shock. Symptoms of anaphylactic shock include: decreased blood pressure, tachycardia, chest pain and convulsions, as well as abdominal pain, bronchospasm, and cardiorespiratory failure [7]. Sometimes anaphylactic shock is accompanied by erythema or angioedema [40]. Anaphylactic shock often occurs after taking antibiotics (penicillin), NSAIDs, ACE inhibitors, contrast agents and muscle relaxants [1, 39, 40, 42]. In the United States, 75% of cases of anaphylactic shock are caused by penicillin [1].
DIAGNOSIS OF DRUG ALLERGIES
Diagnosis of drug allergies is quite complex and, as a rule, begins with a detailed collection of a life history. Anamnesis data should be supplemented by laboratory tests such as a complete blood count (CBC) with a description of the leukocyte formula, determination of the concentration of IgG, IgM and circulating immune complexes (CIC). In case of established IgE-dependent allergy, it is necessary to determine the IgE level. Intradermal tests are often used [2, 43]. According to the European Society of Drug Allergy (ENDA), the diagnosis of drug allergy is established on the basis of patch tests, intradermal tests, determination of the level of specific IgE against a particular drug and provocative tests [44]. Skin testing is usually performed to diagnose allergies to amoxicillin, erythromycin, fluoroquinolones, rifampicin, vancomycin. These tests may be useful for maculopapular rashes and generalized eczematous rashes (GEEs) [45].
To diagnose anaphylactic reactions, the basophil activation test (BAT) [46] is increasingly used, which is based on determining the expression of markers on the surface of basophils: CD63, CD203c using the cytometric method after stimulation with an antigen - a specific allergen. Basophils are easy to stimulate and identify by flow cytometry, and can serve as indicators of IgE sensitization [47]. Using flow cytometry, it is possible to determine several allergens at once in one procedure, and at the same time use a small amount of the patient’s blood. This is a highly sensitive and specific method, and serves for differential diagnosis when there is a discrepancy in the results of tests for the determination of specific IgE intradermal tests [48]. VAT is used in the diagnosis of allergies to β-lactam antibiotics [49], NSAIDs and cyclosporine [50], heparin [51], and hyaluronidase [52].
TREATMENT OF DRUG ALLERGIES
Treatment of drug allergies mainly consists of drug withdrawal. In some cases, with skin lesions or effects on the body, it is necessary to carry out hyposensitizing and immunomodulatory therapy [53].
There are situations when a patient needs to take a drug to which he is allergic. In such cases, the patient is given a course of desensitizing therapy. For example, desensitization to penicillin is necessary in the case of a diagnosis of bacterial endocarditis, meningitis or syphilis of the central nervous system [20]. However, in such patients the allergy to the antibiotic persists. Desensitization is also used in case of allergies to cephalosporins, cotrimoxazole, metronidazole, streptomycin, vancomycin and fluoroquinolones [53].
CONCLUSION
Many medications can cause side effects, allergic and non-allergic reactions, including effects on both the skin and the body as a whole. Diagnosis of drug allergies is based on skin tests, measuring the level of IgE to specific active substances and drugs, and conducting a basophilic activation test to diagnose anaphylaxis. Treatment of allergies is usually based on drug withdrawal and desensitization therapy. In order to prevent harm to health or even death in the case of anaphylaxis, as well as exacerbation and relapse of allergies, it is important to accurately diagnose drug allergies in patients.
Risk factors
Although anyone can have an allergic reaction to a medicine, several factors may increase the likelihood of reactions:
- a history of other allergies such as food allergies or hay fever;
- personal or family history of drug allergies;
- increased drug exposure due to high doses, repeated or prolonged use;
- certain diseases commonly associated with allergic reactions to medications, such as HIV infection or Epstein-Barr virus.
Read also
Allergic bronchial asthma
What is allergic bronchial asthma Bronchial asthma is a fairly common chronic disease, which in most cases is allergic in origin.…
Read more
Allergic dermatitis
What is allergic contact dermatitis? Anyone has ever experienced skin symptoms after using various skin care products, shower gel or shampoo. Such…
More details
Allergic conjunctivitis
What is allergic conjunctivitis With prolonged exposure of the human body to allergens, such as pollen, yeast spores, eye symptoms associated with inflammation may appear.…
More details
Food allergies
What is the difference between food allergy and food intolerance? Food allergy is the response of the immune system to the intake of a particular food that causes an allergic reaction. Even a small amount of associated...
More details
The concept of secondary immune deficiency
The concept of secondary immune deficiency Immunodeficiency disorders can be congenital or acquired. A congenital or primary disorder is something that a person is already born with. Purchased...
More details
Symptoms of drug allergies in adults
The most common signs and symptoms of drug allergies are hives, rash, or fever. Drug allergies can cause serious reactions, including a life-threatening condition that affects multiple body systems (anaphylaxis). Important! A drug allergy is not the same as a side effect of a drug, a known possible reaction listed on the drug label. Drug allergy is also different from drug toxicity caused by drug overdose. Signs and symptoms of a serious drug allergy often occur within an hour of taking the medication. Other reactions, especially rash, may occur hours, days, or weeks later. These may include:
- skin rash;
- hives;
- itching;
- high temperature;
- swelling at the injection site and swelling throughout the body;
- shortness of breath;
- wheezing;
- runny nose;
- itchy, watery eyes.
Anaphylaxis is a rare, life-threatening drug allergy reaction that causes widespread dysfunction of body systems.
Drug allergies - symptoms and treatment
Allergies to medications can occur in any part of the body and in any organ. Symptoms range in severity from minimal discomfort to life-threatening conditions, and their duration ranges from minutes to weeks or months.
There are three groups of drug allergy symptoms :
- manifestations that occur in the first minutes or within an hour after administration of the drug - acute urticaria, anaphylactic shock, bronchospasm, angioedema;
- allergic reactions of the subacute type, developing up to 24 hours after using the drug - maculopapular exanthema, fever, thrombocytopenia, agranulocytosis;
- symptoms that develop within a few days or weeks after using the medicine - serum sickness, damage to internal organs, lymphadenopathy, vasculitis, arthralgia.
The most common manifestations of drug allergies:
- urticaria - the appearance on the skin of the body and face of rash elements from small pale pink to large spots of bright pink or even burgundy color, occupying almost the entire area of the body (a distinctive feature is the itching of these elements);
- increased temperature due to rashes (not always);
- swelling of the face or eyelids (most often asymmetrical);
- damage to the upper respiratory tract (bronchospasm).
With drug allergies, various disorders are possible:
- systemic (affecting the entire body);
- localized:
- skin lesions;
- damage to other organs and systems.[11]
SYSTEMIC LESIONS
Anaphylaxis is a serious life-threatening systemic hypersensitivity reaction. It occurs literally a few minutes or hours after the penetration of the allergen.
Anaphylaxis is indicated by the occurrence of two or more of the following symptoms:
- widespread urticaria on the skin and/or mucous membranes, which is accompanied by itching and/or redness, swelling of the lips, tongue or uvula;
- coughing, sneezing, nasal congestion, wheezing in the chest, shortness of breath, difficulty breathing (sometimes with noise and whistling) and, as a result, hypoxemia (lack of oxygen in the blood);
- a sharp drop in blood pressure (BP), loss of consciousness, sphincter paralysis;
- changes in the digestive system - cramping abdominal pain and vomiting.
Another variant of the course of anaphylaxis is an acute isolated decrease in blood pressure, which also occurs a few minutes or hours after taking the allergen drug. Systolic (upper) blood pressure in adults drops below 90 mm Hg. Art. or more than 30% of the initial pressure. The level of blood pressure in children and its reduction depends on age.
Quite often, similar symptoms may indicate non-allergic anaphylaxis. Its treatment is also no different from the relief of allergic anaphylaxis. The only difference is that true anaphylactic shock is much more severe and the risk of mortality is higher.
Acute severe widespread dermatoses:
- Exudative erythema multiforme (EME) is a rash of various shapes, represented by focal redness and “target-shaped” papules, which can develop into vesicles and bullae (bubbles), as well as erosion. The rash usually occurs on the skin of the hands, feet, genitals and mucous membranes.
- Stevens-Johnson syndrome (SJS) is a severe form of MEE that affects not only the skin and mucous membranes, but also internal organs. The area of allergic rashes on the skin occupies no more than 10%. Accompanied by fever and malaise.
- Toxic epidermal necrolysis (Lyell's syndrome) is a severe allergic reaction, life-threatening, manifested by widespread damage to the skin and mucous membrane (more than 30% of the surface), peeling of the skin, severe intoxication and impaired functioning of all organs. This condition is often preceded by MEE and SSD.[2]
Serum sickness is an allergic reaction that lasts several days or weeks. Occurs after the administration of heterologous serums and the use of penicillins, cytostatics, sulfonamides (antimicrobial drugs) and NSAIDs. The first manifestations occur 1-3 weeks after the start of treatment. These include: rash, fever, pain in large joints and swollen lymph nodes. Less commonly, allergies are accompanied by Guillain-Barré syndrome, glomerulonephritis (damage to the glomeruli), damage to peripheral nerves and systemic vasculitis.
Systemic drug-induced vasculitis is an allergic reaction in which a symmetrical hemorrhagic rash appears on the skin of the lower extremities and sacrum. At the same time, fever, malaise, muscle pain and anorexia appear. In more severe cases, the joints, kidneys and gastrointestinal tract are affected. In rare cases, infiltrates (accumulations of blood and lymph) appear in the lungs, and the functioning of nerve fibers is disrupted (manifested by muscle weakness and pain in the affected area of the body).
Drug-induced lupus syndrome is an allergic reaction, the symptoms of which are similar to those of systemic lupus erythematosus. The difference is the absence of a “butterfly” on the cheeks (extremely rare). The course of such an allergy is favorable. It can manifest itself as pain in the joints and muscles with an increase in the size of the liver and impaired renal function (glomerulonephritis). After discontinuation of the allergen drug, the patient's condition improves after a few days or weeks.
Drug fever is an undesirable reaction that differs from other fevers by maintaining relatively good health despite high fever and stunning chills. It disappears 2-3 days after stopping the allergen medication, but if it is used again, it appears after a few hours.
Drug hypersensitivity syndrome (DRESS) is a potentially life-threatening reaction to drugs that causes skin rash and fever, enlarged lymph nodes, hepatitis and other systemic lesions, and increased levels of white blood cells and eosinophils in the blood. The listed symptoms can develop from one week to three months and last about several weeks even after discontinuation of the allergen drug.
SKIN LESIONS
Maculopapular rash is an itchy rash that suddenly appears 7-10 days after starting the medication. Occurs mainly on the torso. May develop into Stevens-Johnson syndrome and Lyell's syndrome. Triggering drugs: penicillins, NSAIDs, sulfonamides and anticonvulsants.
Urticaria - single or multiple blisters of various sizes and locations, capable of merging and accompanied by angioedema. As a rule, the rash disappears without a trace. Provoking drugs : NSAIDs, ACE inhibitors, radiopaque (iodine-containing) substances, B vitamins, narcotic analgesics, sulfonamides, penicillins and other antibiotics.
Angioedema is a painless swelling of various localizations with clear boundaries that is painless to the touch, which is sometimes accompanied by a rash like urticaria and itchy skin.
Allergic vasculitis is an inflammation of the vascular walls, which is accompanied by symmetrical rashes in the form of small hemorrhages on the skin of the legs (usually in the lower third), buttocks and arms. At the same time, the skin of the face and neck remains unchanged. Provoking drugs: sulfonamides, barbiturates, gold salts and iodine-containing drugs.
Allergic contact dermatitis is an allergic skin lesion that occurs at the site of drug exposure, which is manifested by erythema, edema, and sometimes the appearance of vesicles and bullae. In some cases, inflammation may spread to an area of skin that has not been in contact with the drug. Provoking drugs: neomycin, chloramphenicol, sulfonamides, benzocaine, penicillin and other antibiotics.
Fixed erythema is an inflammatory allergic rash in the form of erythema, bullae or edematous plaques of various sizes with clear ridges. It may occur again even after apparent improvement. Two hours after repeated use of the causative drug, the rash appears in exactly the same place and persists for approximately 2-3 weeks, leaving chronic post-inflammatory pigmentation. Provoking drugs: tetracyclines, barbiturates, sulfonamides and NSAIDs.
Photodermatitis is an allergic rash in the form of redness that occurs on open areas of the body, sometimes accompanied by the appearance of vesicles and bullae. Provoking agents: topical drugs, including halogenated phenolic compounds added to soap, aromatic substances, NSAIDs, sulfonamides and phenothiazines.
The Arthus-Sakharov phenomenon is a local allergy in the form of an infiltrate, abscess or fistula, which appears 7-9 days or 1-2 months after contact with the drug. Provoking drugs: heterologous serums and antibiotics, as well as insulin (1-2 months after its administration).
Exfoliative erythroderma is a life-threatening common skin lesion (occupies more than 50% of its surface), represented by redness, infiltration and extensive peeling. Provoking agents: arsenic, mercury and gold preparations, penicillins, sulfonamides and barbiturates.
Erythema nodosum is an allergic reaction in the form of symmetrical and painful when touched subcutaneous red nodes of different sizes, which usually occur on the front surface of the legs. May be accompanied by a slight increase in temperature, malaise, pain in muscles and joints. Provoking agents: sulfonamides, oral contraceptives, penicillins, barbiturates, bromine and iodine preparations.
Acute generalized exanthematous pustulosis is an allergic skin reaction in which pustular rashes appear against a background of redness. It occurs with an increase in temperature to 38°C and the number of leukocytes in the blood. Disappears 10-15 days after discontinuation of the allergen medication. Provoking drugs: calcium channel blockers (diltiazem), sulfonamides, aminopenicillins (ampicillin, amoxicillin) and macrolides.
DAMAGES TO OTHER ORGANS AND SYSTEMS
In addition to the listed clinical manifestations, drug allergies may cause:
- damage to the respiratory system - rhinitis, bronchospasm, inflammation of the lungs and the formation of an eosinophilic infiltrate in it (Leffler's syndrome) - due to allergies to pyrazolones, carbamazepine, acetylsalicylic acid and other NSAIDs, ACE inhibitors, beta-blockers, penicillins and sulfonamides;
- lesions of the hematopoietic system - hemolytic anemia and thrombocytopenia - in response to taking streptomycin, quinidine, rifampicin, penicillin, ibuprofen and other sulfonamides, sulfonylurea derivatives, thiazide diuretics and gold salts;
- damage to the circulatory system - myocarditis (extremely rare) - when taking sulfonamide, penicillin and methyldopa;
- lesions of the gastrointestinal tract and hepatobiliary system - gastroenterocolitis, cholestasis, acute hepatitis, chronic hepatitis (rarely) - when taking pyrazolones, sulfasalazine, carbamazepine, allopurinol, sulfonamides, halothane, isoniazid and phenytoin;
- lesions of the urinary system (extremely rare) - acute interstitial nephritis and glomerulonephritis - a consequence of the body’s reaction to gold salts, NSAIDs, heroin, captopril, sulfonamides, penicillamine, penicillins and other β-lactams, rifampicin, ciprofloxacin and allopurinol;
- lesions of the nervous system - peripheral neuritis - reaction to gold salts and sulfonamides.
Other conditions caused by drug allergies
Less common allergic drug reactions occur days or weeks after exposure to the drug and may persist for some time after the drug is stopped. These conditions include:
- serum sickness, which can cause fever, joint pain, rash, swelling and nausea;
- drug-induced anemia, a low red blood cell count that can cause fatigue, irregular heartbeat, shortness of breath and other symptoms;
- drug rash with eosinophilia and systemic symptoms (DRESS), which results in rash, high white blood cell counts, general swelling, enlarged lymph nodes, and recurrence of previously occult hepatitis;
- inflammation of the kidneys (nephritis), which can cause fever, blood in the urine, general swelling, confusion, and other symptoms.
Allergy definition
Mom's allergies can be passed on to the unborn baby
The pharmacy chain offers a huge number of medications that can have a positive effect and eliminate the symptoms of the disease. But when it comes to a child, it is important not only to get rid of allergies, but also not to cause significant harm to the growing body. Therefore, modern mothers face the difficult task of choosing an anti-allergenic drug that can have a therapeutic effect and be absolutely safe for their children.
Self-medication in this case is in no way encouraged; only an experienced doctor can provide proper assistance to a child with allergies. In this article, I would like to consider the characteristics of allergies, the causes of their occurrence, and consider a set of medications for treating children from this disease.
Not all symptoms that impair a child’s performance and well-being should be attributed to allergies. Many of them are signs of the development of other diseases in the child’s body. Allergies in children are characterized by itching, redness of the skin, sneezing, tearing and much more. If these signs appear in a child after a walk or contact with a certain group of objects, it means that the body has actually picked up some allergen, and the disease began to develop in the child.
Allergy refers to a whole complex of symptomatic manifestations caused by the high sensitivity of the immune system to foreign substances or allergens. Symptomatic manifestations of an allergic disease in a child’s body are:
- The appearance of edema;
- Attacks of incessant sneezing;
- Itching in certain areas of the skin;
- Severe runny nose;
- Tearing.
These signs are the most common signs of this disease in a child’s body. If they are detected, the mother should consult a pediatrician to stop the development of the disease and prevent the appearance of deeper symptoms. In a medical institution, experienced specialists will definitely give full advice on the treatment of the disease. Based on the test results, the doctor will be able to determine the type of allergen that causes allergic symptoms in the child. It is not worth joking and neglecting such a disease in a child’s body, since the consequences of neglect can be the most unpredictable. It is also not recommended to buy and give medications to a child without consulting a doctor, since the child may develop an allergy to the components of the medications themselves.
Treatment of drug allergies in adults
Call 112 or emergency medical services if you have signs of a serious reaction or suspect anaphylaxis after taking the medicine. If you have milder drug allergy symptoms, contact your doctor as soon as possible.
Diagnostics
An accurate diagnosis is very important. Research has shown that drug allergies can be over-diagnosed and that patients may report drug allergies that have never been confirmed. Misdiagnosed drug allergies can lead to the use of less appropriate or more expensive medications. The doctor will perform a physical examination and ask you questions. Details about the onset of symptoms, when to take medications, and whether symptoms are getting better or worse are important clues that will help your doctor make a diagnosis.
Your doctor may order additional tests or refer you to an allergy specialist (allergist) for testing. These may include the following.
Skin tests. With a skin test, an allergist or nurse injects a small amount of the suspected drug into your skin using a tiny needle (scarifier) that scratches the skin, an intradermal injection, or a patch. A positive test will cause a red, itchy, raised bump.
A positive result suggests that you may have a drug allergy.
The negative result is not so clear. For some medications, a negative test result usually means you are not allergic to the drug. For other drugs, a negative result cannot completely exclude the possibility of drug allergy.
Blood tests. Your doctor may order a blood test to rule out other conditions that may be causing the signs or symptoms. Although blood tests are available to detect allergic reactions to some medications, these tests are used infrequently due to relatively limited research on their accuracy. They can be used if there is concern about a serious reaction to the skin test.
When your doctor reviews your symptoms and test results, he or she can usually come to one of the following conclusions:
- you are allergic to medications;
- you are not allergic to medications;
- You may have a drug allergy - with varying degrees of certainty.
These findings may help your doctor and you make treatment decisions in the future.
What to do if you are allergic to medications?
How to treat drug allergies? The basic principles of treatment are the elimination of the allergen from consumption, taking antihistamines, dietary nutrition in the presence of a food allergy that aggravates the situation.
Pharmacies offer a wide selection of over-the-counter antihistamines that can always be kept in your medicine cabinet (Claritin, Suprastin, Diazolin, Citrek) and several prescription ones. But antihistamines are not all that a doctor can prescribe.
What to take if you are allergic to medications:
- decongestants - there are prescription and over-the-counter ones (for example, Sudafed, Citrek-D);
- steroids (nasal, inhaled, eye drops, oral);
- bronchodilators;
- mast cell stabilizers;
- leukotriene modifiers;
- activated carbon (or other sorbent) and calcium gluconate as additional agents.
Only a doctor can prescribe the right medications, especially for severe and potentially health-threatening manifestations.
Regardless of whether you or your loved ones have allergies, it is important to know what to do if you are allergic to a medicine. In case of mild skin manifestations that are not life-threatening, you must immediately make an appointment with a doctor (the NEARMEDIC clinic is open seven days a week from morning until late evening). In case of serious reactions (shock, Quincke's edema), you need to act immediately.
What to do with a drug allergy - emergency care:
- call an ambulance immediately;
- place the patient on a hard surface;
- Give any antihistamine you can find in your medicine cabinet, ideally by injection (always have antihistamines, even if no one has allergies);
- give the patient plenty of water to drink;
- if the medicine was taken orally, give activated carbon or another sorbent;
- if the condition worsens before the ambulance arrives, give 1 tablet of prednisolone.
Upon arrival of the ambulance, the doctor will administer adrenaline and hormonal drugs to the patient, after which he will be hospitalized. To quickly remove the allergen, intradroplet administration of cleansing preparations is often used. After a serious reaction, the dangerous drug and its cross-allergens are completely removed from use.
To reduce the likelihood of allergic reactions, do not prescribe medications yourself. When consulting with your doctor before getting a prescription for any medical condition, tell us if you have:
- any allergic reactions;
- reactions to any drugs in the past;
- suspicious symptoms (if the diagnosis has not yet been made) - seasonal lacrimation and rhinitis, sore throat, urticaria, itching, especially after medications;
- about relatives with allergic diseases;
- about fungal infections of nails and skin (can cause hidden sensitization to penicillin).
Modern methods of treatment
Interventions for drug allergies can be divided into two main strategies:
- treatment of existing allergy symptoms;
- treatment that may allow you to take the medicine that is causing your allergy if it is medically necessary.
Treating current symptoms. The following interventions may be used to treat an allergic reaction to a drug:
- stopping the drug - if your doctor determines that you have an allergy or possible allergy to your medications, stopping the medication is the first step in treatment: in many cases, it may be the only intervention needed;
- antihistamines – a specialist may prescribe antihistamines or recommend medications, such as diphenhydramine, that can block immune system chemicals activated during an allergic reaction;
- corticosteroids – oral or injected corticosteroids may be used to treat inflammation associated with more serious reactions;
- Treatment of anaphylaxis – Anaphylaxis requires immediate injection of epinephrine, as well as hospitalization to maintain blood pressure and support breathing.
Taking medications that cause allergies. If you have a known drug allergy, your doctor will not prescribe medication unless necessary. In some cases—if the diagnosis of a drug allergy is unclear or there is no alternative treatment—the doctor may use one of two strategies to administer the suspected drug.
When using any of these strategies, your doctor will provide close monitoring, and supportive care services are available to manage the adverse reaction. These interventions are usually avoided if medications have caused severe, life-threatening reactions in the past.
If the diagnosis of a drug allergy is unclear and your doctor thinks an allergy is unlikely, he or she may recommend dose-dose drug therapy. During the procedure, you will receive 2 to 5 doses of the drug, starting with a small dose and increasing it to the desired amount. If you reach the therapeutic dose without any reaction, your doctor will conclude that you are not allergic to the drug. You will be able to take the drug as prescribed.
Desensitization with drugs. If you need to take a medicine that is causing an allergic reaction, your doctor may recommend a treatment called drug desensitization. With this treatment, you receive a very small dose and then gradually increase it every 15 to 30 minutes over several hours or days. If you can reach the desired dosage without any reaction, you can continue treatment.
Children's allergy medications
Scientists divide the variety of medicines produced in the world that eliminate allergy symptoms into three large groups:
- The first group of allergy medications includes medications that were one of the first to be released to combat it. This includes diphenhydramine, known to many generations, diazolin, which effectively helps our parents, and, of course, Tavegil, which is well known in our country. Today, the effectiveness of these drugs is not the highest and can lead to various side effects on the child’s body. The most common of them are: the appearance of excessive drowsiness, a feeling of dryness in the child’s mouth, as well as a significant slowdown in the body’s behavioral responses. The latter, in turn, are by no means contraindicated in childhood.
- The second group of drugs includes antihistamines. These include Zyrtec and Claritin.
- Scientists include the third group of drugs: Telfast and Erius. Unlike the first group of allergy medications for children, these medications are practically safe for the child’s body.
Fenistil
Tavegil for the treatment of allergies
A good medicine for the manifestation of allergic symptoms in childhood is a new drug called fenistil. This medicine has a positive and mild effect, eliminating any allergy and its symptoms. The drug fenistil can be used by children from the first month of life. The medication should be taken based on the recommendations of the attending physician, but it should not be given before the child falls asleep.
Prevention of drug allergies in adults at home
If you are allergic to medications, the best prevention is to avoid taking the problematic medications. Steps you can take to protect yourself include the following:
- tell healthcare professionals about allergies – make sure your drug allergies are clearly noted in your medical records, tell other professionals, such as your dentist or any health care professional, about the allergies;
- Wear a bracelet - Wear a medical alert bracelet that indicates your drug allergies - this information can ensure proper treatment in an emergency.
Major potentially dangerous drugs
Hypersensitivity occurs to any drug, but statistically there is a group of medications that are more likely to provoke allergies. Let's look at common medications and how drug allergies can manifest themselves:
- Penicillins. This is a group of antibiotics that have a similar mechanism of activity. If a negative effect is observed already at the first dose, this is explained by hidden sensitization with small doses of drugs from milk, eggs, fish or cross-reactions with human pathogenic fungi. During the reaction, hypersensitivity myocarditis and rashes appear. We can talk about the allergic nature of the reaction with urticaria, measles-like and erythematous rash. Urticarial and maculopapular rashes are immune independent.
- Cephalosporins. The most common manifestation is eosinophilia (up to 8%), others are much less common. Skin manifestations are possible in 1-3% of patients.
- Tetracyclines. Allergies to tetracyclines appear rarely in the form of rash and urticaria with itching, asthma, pericarditis, headaches, etc. Photoallergic reactions are possible when taking demeclocycline. A reaction to one type of tetracycline guarantees cross-combination with other derivatives. With constant use, leukocytosis, thrombocytopenia, and leukopenia may develop.
- Macrolides. Erythromycin causes cholestasis, erythromycin estolate causes liver damage.
- Aminoglycosides. When taking Streptomycin, fever, rashes, and dermatitis occur. This is most often noticeable among workers in the medical field and pharmaceutical industry. Cross-reactions are observed with neomycin.
- Analgesics, NSAIDs. Reactions occur in the form of bronchospasm, rhinitis, shock, and skin rashes. 0.3% of people are sensitive to aspirin, most of them among patients with urticaria and bronchial asthma. Patients allergic to aspirin may be sensitive to other drugs.
In addition to the drugs described above, allergies can be caused by quinolones, sulfonamides, barbiturates, phenothiazine derivatives, local anesthetics, protein-based drugs, hormones, and ACE inhibitors.