Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Treatment methods
Port-wine stains, also called capillary angiodysplasia or flammeus , are one of the most common vascular malformations. They are a network of pathologically altered capillaries located superficially or deep under the skin and visible through it.
In our company you can purchase the following equipment for the treatment of wine stains:
- M22 (Lumenis)
According to world statistics, port-wine stains are registered on average in 0.1–2.0% of newborns. Most often they occur in representatives of the Caucasian race, with equal probability in both boys and girls.
Acquired melanocytic nevus (mole) - symptoms and treatment
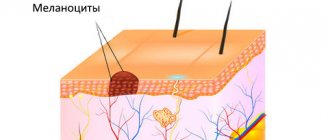
Depending on the location of melanocytes, three groups of acquired nevi are distinguished:
- Transitional nevi are formed by nests of melanocytes located at the border of the dermis and epidermis. They may be in the form of a spot or slightly raised above the skin. The color varies from light brown to black, and the center of the mole is darker than its edges.
- Complex nevi consist of nests of melanocytes located both at the border of the dermis and epidermis, and in the dermis itself. They are pigmented nodules that rise above the skin at different heights. Their surface can be smooth or spherical, color - from light to dark brown.
- Intradermal nevi occur when nests of melanocytes are located in the dermis. Nevus cells often stop producing melanin, so moles practically do not differ in color from the surrounding skin, but rise above it. They have the shape of a papule, dome or papilloma, their texture is soft and elastic [42].
Acquired nevi can be classified into typical and atypical. Some atypical variants are divided into separate forms: blue nevus, halo nevus, Spitz nevus, eclipse nevus and nevus of the sebaceous glands.
Atypical, or dysplastic nevi are benign acquired melanocytic nevi that have the characteristics of melanoma: asymmetry, irregular borders, heterogeneity of color and a diameter greater than 6 mm.
Atypical nevi are more common when there are a lot of nevi on the body as a whole. Among white-skinned people, atypical nevi occur in 2–10% of the population [22]. As a rule, they appear after puberty [23]. Typically, there are more nevi in areas exposed to sunlight, such as on the torso and legs, and fewer on the chest and buttocks.
Based on their origin, atypical nevi can be divided into two groups:
- Sporadic nevi appear spontaneously under the influence of various external factors leading to mutations in cells. Relatives of patients usually do not have atypical nevi or melanoma.
- Genetically determined nevi (dysplastic nevus syndrome) - occur due to hereditary predisposition. Relatives also have atypical nevi, and there may be cases of melanoma in the family.
Main characteristics of atypical nevi:
- diameter from 0.6 cm;
- irregular outlines with lighter edges;
- the shape is flat, the mole is flush with the surrounding skin;
- the borders are uneven, smoothly blending into the skin;
- the color is heterogeneous, the color intensity can vary from pale brown to black.
An eclipse nevus is a type of complex nevus that is brown in color with a light center and a darker, star-shaped edge. In children, it often develops on the scalp. Despite the heterogeneous color and uneven borders, such nevi are benign. If there are no other warning signs, such as induration and ulceration, then biopsy or removal of such nevi is not necessary [24].
Halo nevus (Sutton's nevus) is a melanocytic nevus surrounded by a symmetrical round or oval halo of depigmentation, i.e., a lighter area of skin. Haloing usually occurs in acquired melanocytic nevi, but can also occur in congenital nevi, blue nevi, Spitz nevus, and melanoma.
Halo nevi occur in almost 5% of white-skinned children aged 6–15 years, most often located on the back [26]. Common in people with vitiligo or relatives with vitiligo. In approximately half of the cases there are multiple nevi (more than 30) [27].
There are four stages of halo nevus development:
I. Pigmented nevus surrounded by a halo of depigmentation.
II. Pink nevus with a halo of depigmentation.
III. Round area of depigmentation without nevus.
IV. Skin of normal color after repigmentation of the halo.
Any of the four clinical stages can last from several months to several years [28]. Up to 10 years can pass between stages I–II and IV.
If the halo nevus has a typical appearance, then a biopsy is not required [29]. Since children with halo nevi usually have many nevi on their entire body, the entire body is examined. This will help identify atypical nevi and determine whether they need to be monitored or biopsied and removed. If there are atypical or concerning signs, a biopsy of the central portion of the nevus is performed. There is no need to remove the halo.
Multiple halo nevi are common among adolescents and young adults. They are rare in middle-aged and older people and may be a manifestation of an immune reaction to cutaneous or ocular melanoma. In this case, a biopsy may be required.
Blue (blue) nevus is a benign growth of dendritic skin melanocytes that actively produce melanin. The blue color is produced when short wavelengths of light are scattered by melanin in the skin, a phenomenon known as the Tyndall effect. Most often, blue nevi appear on the scalp, neck, back of the hands and feet, and in the sacral region.
There are several variants of blue nevi:
- A common blue nevus is a single, dome-shaped, blue or black-blue papule less than 1 cm in diameter. Such nevi often appear during adolescence and are found on the dorsum of the hands and feet.
- A honeycombed blue nevus is a more raised and larger nodule or plaque, measuring more than 1 cm with a smooth or slightly uneven surface. Such nevi can be congenital or acquired; they are most often found on the scalp, face, sacrum and buttocks.
If the blue nevus is stable, then it does not need to be removed. But if it appears suddenly and grows quickly, or a pre-existing nevus increases sharply, then a biopsy is necessary.
Spitz nevi are benign, usually acquired nevi, which are a collection of melanocytes. They most often appear in childhood and are located on the face and legs. Such nevi grow quickly, which often worries patients and parents.
A Spitz nevus is a papule or nodule that is uniformly pink, brown, red, or red-brown in color. Usually symmetrical with a clear outline, less than 1 cm in diameter. The surface may be smooth or warty. Sometimes the nevus includes dark pigment in the form of a star or peripheral stripes.
Pigmented spindle cell nevus of Reed is a variant of Spitz nevus that is common among adolescents and young adults. It often appears on the thighs and has the appearance of a thin papule ranging from dark brown to black in color [30].
A small, stable Spitz nevus with typical features can be observed [31]. Such nevi may shrink or disappear over time [32]. But if the Spitz nevus has atypical signs (size more than 1 cm, asymmetry or ulceration), then it is removed after a biopsy.
A sebaceous nevus is a localized lesion, predominantly consisting of the sebaceous glands. It occurs with equal frequency in men and women, regardless of skin color. It is observed in 0.3% of newborns [15]. Often at birth or in early childhood it appears as a single linear or rounded area with a smooth or velvety surface. It comes in pink, yellow, orange or light brown. Typically found on the scalp or face, extensive lesions are rare.
During adolescence, it becomes warty or nodular and may darken and enlarge. In approximately 1% of cases, such a nevus degenerates into cancer. This almost always occurs after puberty [15].
Etiology and pathogenesis of port-wine stains
In most cases, port-wine stains (nevus flaminga) are a birth defect . They are present in the baby immediately after birth and increase in size in proportion to the further growth of the child. An important feature of port-wine stains is the lack of spontaneous regression - they form for a lifetime and, as a rule, have a negative impact on a person’s psychological state.
In rare cases, port-wine stains may appear on apparently healthy skin in adulthood - this is the so-called acquired capillary angiodysplasia . Sometimes port-wine stains may not be an independent pathology, but signs of severe syndromes: Sturge-Weber (encephalotrigeminal angiomatosis with damage to the pia mater) or Klippel-Trenaunay (vein malformations with hypertrophy of bones and soft tissues).
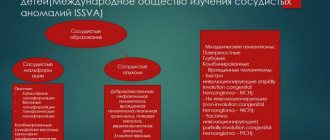
The International Society for the Study of Vascular Anomalies (ISSVA) classifies capillary angiodysplasia according to the predominant vessel type—arterial, venous, lymphatic, capillary, or complex.
Reasons for development
One of the reasons for development is heredity.
In this situation we are talking about an autosomal dominant type of inheritance. Risk groups include:
- white-skinned babies,
- premature,
- girls.
Other doctors suggest that the appearance of the formation occurs due to fetal hypoxia during the passage of the birth canal. It appears in areas where the pressure during the birth process is especially strong. Hypoxia and pressure provoke microvascular paralysis, which gives the stain effect.
Clinical manifestations of flaming nevus
In a newborn, capillary angiodysplasia is a light pink or pink spot, which, upon closer examination, consists of individual vascular branches. Statistically, most port-wine stains are found on the face or neck. Localized on the face, 45% of angiodysplasias occupy from 1 to 3 areas innervated by the V pair of cranial nerves (nervus trigeminus), and 55% occupy more than 1 area with a transition to the opposite side.
Flaming nevus (wine stain), according to T. Fitzpatrick
As the child grows and matures, the port-wine stain proportionally increases in size, becoming light red or completely red. At the same time, it looks like a continuous network of vessels in which it is impossible to distinguish individual branches.
Subsequently, the vessels of the neoplasm gradually expand, which significantly thickens it and raises it above the surface of healthy skin. A port-wine stain is easily injured and bleeds, the wound can become infected, and the pronounced size of the tumor in some cases disrupts the symmetry of the patient’s face. Malignancy of capillary angiodysplasia and its degeneration into a cancerous tumor is possible.
What is nevus of Ota?
Nevus of Ota is a dermal melanocytosis, first described by Hulk in 1860 and then expanded by Ota and Tanino in 19391, 10.
Clinically, it is distributed along the ophthalmic and maxillary divisions of the trigeminal nerve and presents as a bluish or gray patch on the skin2. In addition, it can also affect the mucous membrane of the eardrum, nasopharynx and palate3.
About 50% of cases are congenital, resulting from abnormal migration of melanoblastic neural tube cells along the first and second divisions of the trigeminal nerve during embryogenesis10.
Other cases occur during puberty and adulthood.
Initial hyperpigmentation may appear as a light-colored patch that worsens as the patient ages.
Treatment Methods for Port Port Stains
The simplest method of not so much treating as masking port-wine stains is the use of cosmetics . Properly selected products help hide the tumor and allow such patients to feel quite comfortable in public places. A more radical option, which is also not aimed at treating a port-wine stain, is to tattoo over the tumor.
Drug therapy for capillary angiodysplasia has not demonstrated significant effectiveness in treating port-wine stains. However, there is evidence of positive results from topical use of the immunomodulator imiquimod 5 times a week under occlusion with plastic film for 4 weeks.
Before the invention of lasers, the radical treatment for port-wine stains was skin grafting . This operation, like other invasive interventions, has limitations and carries certain risks.
Today, light and laser therapy - IPL and Nd:YAG lasers - are actively used to treat port-wine stains. The principle of such therapy is the selective destruction of pathological vessels due to their heating when hemoglobin absorbs light or laser energy. This type of therapy is more suitable for situations where the vascular defect is completely formed and there is no way to influence it with other types of therapy. Destruction of blood vessels leads to a pronounced and persistent aesthetic defect. Laser and light therapy procedures are carried out without compromising the integrity of the skin, are well tolerated and do not require long-term rehabilitation.
Where is the spot located and what color is it?
Nevus of Unna in a newborn (photo below) most often forms on the back of the head, near the eyes and on the bridge of the nose. The color of the formation may be pale pink or red. If the baby cries, the spot usually becomes brighter.
The spot formed on the forehead usually has a brighter and more saturated color. If you press on the formation, it turns pale.
Nevus can also appear on the body. But in this case, there is a big risk that it will not disappear with age. Quite often, a spot that appears on the back of the head remains for life, but due to its specific location it remains barely noticeable.
If the stain does not disappear by two to four years, there is a high risk that it will not disappear.
As they grow older, the formation grows in size and darkens.
Dysplastic nevus syndrome
Unfortunately, there is a syndrome that in Russian literature is often called nevus dysplastic syndrome (in foreign literature - FAMMM).
This disease has 2 diagnostic criteria
- the number of dysplastic nevi on the skin is more than 50
- melanoma in relatives
This disease may be associated with a mutation in the CDKN2A gene, which also increases the risk of developing pancreatic cancer
With this syndrome, the risk of developing melanoma, according to different authors, varies from 56 to 100%. The disease requires regular (once every few months) monitoring by an oncologist.
Diagnostic measures
As a rule, the correct diagnosis can be established by external signs. If a spot appears on the bridge of the nose or forehead, a consultation with a neurologist is usually recommended. It is extremely rare that education may indicate some problems with the child’s mental development.
On the other hand, the shape and size of the spot are in no way related to the presence or absence of any pathologies. However, a full examination will make it possible to make a correct diagnosis and exclude the presence of more serious pathologies.
In any case, if there is a problem, the child should be under constant medical supervision. You should always remember that any formation on the skin can be a symptom of an internal disease, so it is imperative to determine the cause of its appearance.
Cryodestruction
This technique involves treating Unna's nevus with liquid nitrogen. This is not as popular a procedure as laser. The essence of the technique is that the stain is exposed to cold, and eventually it disappears. If the angel's kiss is large in size, then there is a risk that there will be scars at first, but over time they will resolve.
Complete regeneration of the skin occurs within 2 months.
The procedure is the direct opposite of laser therapy. However, anesthesia is not required in this case, since the child does not feel pain from exposure to cold. The nitrogen exposure procedure is not popular for a simple reason - it requires a highly qualified doctor to perform it.