Linear nevi - symptoms
Linear epidermal nevus was first described by Baerensprung in 1863 as naevus unius lateralis. These are congenital changes, most often present at birth, but sometimes they may not appear until childhood.
At the first stage of the disease, they look like limited areas of excessive pigmentation that do not protrude above the surface of the skin, smooth spots or papules that match the color of the skin. Later in the disease they take on a papillary form. The discoloration is associated with mild hyperkeratosis.
Epidermal moles can be found on any area of the skin, including the anus and urogenital areas. They are often located on the face and neck, scalp, trunk or limbs. The most common changes are linear and unilateral, along Blaschko's line, not extending beyond the midline of the body.
They can be:
- single, clinically resembling seborrheic keratosis;
- multiple warts, sometimes generalized, affecting large areas of the skin and persisting throughout life.
Sometimes they have a linear, vortex, striped system, often generalized, covering large areas of the body.
Moles appear in early childhood, grow with the patient and do not regress. Sometimes they can flare up and disappear, especially in the case of inflammatory linear papillary epidermal nevus, which can be accompanied by pain, burning and erosions, but never completely goes away.
Cases of the development of a malignant neoplasm in an epidermal nevus are rare, but not excluded. Isolated cases of development at the site of the lesion have been described:
- keratoacanthomas;
- basal cell carcinoma;
- squamous cell carcinoma.
Such moles may be associated with other developmental defects of the central nervous system, skeletal system, vision, as well as with some developmental disorders, for example, Proteus syndrome, McCune-Albright syndrome, Klippel-Trenaune syndrome.
When does a nevus need to be removed?
Of course, it is better to remove all melanoma-dangerous nevi before they begin to malignize. As for melanoma-free moles, most often they are removed for the following reasons:
- a person wants to get rid of a noticeable defect on the skin;
- the nevus can be accidentally damaged by rubbing body parts or during hygiene procedures, which is dangerous due to possible malignancy caused by damage;
- the process of malignancy began, and the nevus began to transform into a malignant tumor.
All nevi that are on a person’s body and face should be under constant observation. The slightest changes may indicate the beginning of the process of malignancy. We strongly recommend that you do not hesitate to contact a dermato-oncologist if you notice:
- growth (increase in size);
- color change;
- hair loss from the surface;
- bleeding;
- itching or burning;
- change in shape, “blurring” of edges.
The dermato-oncologist will prescribe a histological examination, which will confirm or not confirm your suspicions. In any case, such a nevus must be removed.
Diagnosis - histopathological features of linear nevi
There is considerable variability in histopathological studies. The most common manifestations:
- hyperkeratosis;
- acanthosis;
- papillomatosis.
Some moles may exhibit acantholysis and dyskeratosis, resembling Darier's disease.
Sometimes you can find a picture of epidermolysis with hyperkeratosis, reminiscent of congenital bullous erythroderma ichthyosis. In these cases, mutations in the keratin 1 or 10 genes are found.
Diagnosis of nevus
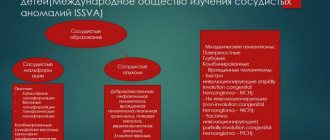
Types of epidermal nevi
There are several clinical types of epidermal nevi. This classification is not definitive, since epidermal moles can be hard, linear and inflamed at the same time.
Soft papillary nevus of the epidermis . This is most often a small flesh-colored or gray formation with a soft, velvety surface. Individual papules forming clusters resemble senile warts.
Hard papillary nevus.
Unilateral, segmented, most often located on the trunk and limbs. These are tall or flat, raised discolorations of normal skin, light or dark brown, with a papillary surface.
Inflammatory linear verrucous epidermal nevus.
This is a special form of epidermal nevus with inflammation and severe itching. ILVEN may worsen and disappear, especially in the form of psoriasis-like psoriasis.
According to the conclusions of the study. Altman and Mehregan, diagnostic criteria for such moles include a number of features:
- early onset is noted - in 75% of cases before 5 years,
- more common in females (4 times more often);
- frequent localization on the left lower limb and buttocks;
- itching is usually present;
- histopathological appearance resembling psoriasis - a characteristic pattern of parakeratotic areas with visible psoriasis-like epidermal hyperplasia, mild spongy edema and exocytosis of lymphocytes;
- Such nevi have no tendency to spontaneous regression and resistance to treatment.
The lesions are linear, pruritic, erythematous lesions with a flaking surface and may resemble psoriasis lesions with a linear pattern. They are distinguished from psoriasis by the absence of Munroe microcirculation and the lack of epidermal involucrin expression in ILVEN. The connection with psoriasis is confirmed by the participation of the cytokines IL-6, IL-1, TNF-alpha, ICAM-1 in the pathogenesis.
Horny nevus (nevus corniculatus)
. This is the rarest form of epidermal nevus. The clinical picture shows very intense keratosis with the formation of thick papillary growths and filamentous formations. Histopathological examination shows foci of acantholysis with depressions in the epidermis filled with dense keratin.
Pediatric epidermal nevus.
This variety is characterized by congenital hemidysplasia, unilateral ichthyosis and limb defects. All of these disorders can occur, but it can only be the cutaneous form. The lesions are located unilaterally and do not extend beyond the midline of the body, with the most common lesions being the flexor folds. They have the character of erythematous lesions covered with yellow hyperkeratotic scales and sometimes with horny plugs. This type of mole occurs only in women because the gene responsible for the condition is located on the X chromosome.
Epidermal nevus syndrome, which is a combination of epidermal nevus with other developmental defects, has been clinically identified.
There are 4 clinical variants of the syndrome (Michalovsky classification):
- four-symptom form - lesions of the skin, bones, nerves and eyes.
- three-symptomatic form - skin, bone and nervous changes.
- two-symptomatic form - skin and bone changes.
- monosymptomatic form - the presence of a linear papillary epidermal nevus.
Introduction
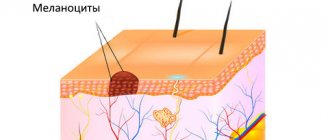
The process of formation and development of cutaneous melanoma (MC) remains a subject of interest to many scientists. To date, data have been obtained on the heterogeneous genetic nature of various forms of tumors and the influence of exogenous factors on the appearance of melanoma [1], there is an understanding of the initial manifestations of the disease, and experience has been accumulated in non-invasive diagnosis of melanoma [2]. Numerous studies have shown that the tumor process occurs against the background of a pre-existing melanocytic nevus in no more than a third of cases [3, 12], however, the biological role of “moles” in this situation remains unclear. The article provides a description of clinical cases of MK that arose against the background of melanocytic nevi, a review of the literature and a discussion of this problem.
Clinical case 1
A 37-year-old woman came for examination of a pigmented formation on the skin of her back. According to the patient, several years ago she noticed changes in a pre-existing “mole” after repeated sunburns. Clinical examination revealed multiple melanocytic nevi, incl. clinically atypical. The changing formation was located in the interscapular region and was represented by a light brown plaque with blurred boundaries, slight hypertrichosis and preserved skin pattern, measuring 17x10 mm. Along the lower edge of the formation, the formation of an intensely colored black plaque of irregular shape, with sharp boundaries, a disturbed skin pattern, measuring 10×7 mm was noted
(Fig. 1). During dermoscopic examination, a symmetrical reticular-globular model of structure without atypical structures was determined in the light formation (Fig. 2); in the dark one, an asymmetric, multicomponent model of the structure was determined (Fig. 3). Based on the results of the examination, a preliminary diagnosis was made: “superficial spreading melanoma of the skin, arising against the background of a medium-sized congenital melanocytic nevus. Histological examination confirmed the clinical diagnosis; the tumor thickness according to Breslow was 1.8 mm. The examination, including a biopsy of the sentinel lymph node, did not reveal any evidence of metastatic lesions; the patient was left under dynamic observation.
Clinical case 2
A 36-year-old man presented for examination of multiple skin neoplasms as part of a screening campaign. On the skin of the back (Fig. 4) a small, intensely colored black spot with sharp boundaries, 3x3 mm in size, was revealed.
Along the lower edge of the formation, the presence of a flesh-colored papule, soft consistency, measuring 4x3 mm was noted. The dermoscopic picture of the pigmented area was represented by an atypical pigment network and a zone of hyperpigmentation, while the papular area was represented by a structureless, flesh-colored area and single linear telangiectasias (Fig. 5). Based on the examination results, a preliminary diagnosis was made: “superficial spreading skin melanoma arising against the background of an intradermal melanocytic nevus.” Histological examination confirmed the clinical diagnosis; the tumor was represented exclusively by the intraepidermal component (melanoma in situ).
Clinical case 3
A 57-year-old woman came for an examination on the recommendation of relatives who noticed the appearance of a “strange mole” on the skin of her back.
In the area of the right scapula, a dark brown papule was identified (Fig. 6) with uneven coloring and sharp boundaries, up to 3 mm in size. Light brown pigmentation was visible along the upper edge of the formation. Dermoscopically, the formation was presented with an atypical globular pattern, and there was a pronounced tendency towards peripheral growth (Fig. 7). Based on the results of the examination, a diagnosis of emerging superficial spreading melanoma of the skin was suggested. Histological and immunohistochemical studies with markers of melanocytic differentiation and proliferative activity confirmed the presumptive clinical diagnosis; the tumor thickness was 0.4 mm according to Breslow. An immunohistochemical study also revealed a component of a small congenital melanocytic nevus, which became a background process for the development of a malignant tumor. Comparing the histological data and the clinical picture, it becomes clear that the light brown pigmentation corresponded to a congenital nevus.
Literature review
According to the literature, cases of MC arising against the background of melanocytic nevus have common features: for example, the tumor develops at a younger age, is more often located on the skin of the body and has a smaller Breslow thickness [3–9]. The main risk factor for the development of MC against the background of a nevus is the presence of multiple melanocytic nevi, incl. familial syndrome of dysplastic nevi and MK (FAMMM syndrome) [8, 10].
The clinical manifestations of this combination depend on the histological type of developing melanoma, the stage of the tumor process and the type of melanocytic nevus.
In some cases, it is not possible to unambiguously assume the presence of an underlying benign formation during examination. The most common diagnosis is superficial spreading MK, which forms along the periphery of the melanocytic nevus; less commonly, the nodular form, which can develop within the nevus [6, 10, 11]. The dermoscopic picture in most cases is not difficult and is manifested by a “dermoscopic island” - a focus of atypical or sharply different signs from the structural model of the melanocytic nevus, allowing one to suspect MC [12]. Differential diagnosis should be made with certain types of melanocytic nevi (dysplastic, combined or spotted), the formation of a proliferative node or the development of certain dermatoses within a pre-existing nevus (folliculitis, molluscum contagiosum).
Various congenital and acquired melanocytic nevi can act as a background process for the development of MK, and often “moles” will have banal clinical and, more importantly, histological manifestations [3, 6, 9, 13]. There is a direct correlation between the size of the nevus and the time of its malignancy, as well as the type of MV that forms. It is believed that within giant nevi, the tumor is more often of the nodular variety and forms in the first 10 years of a child’s life, while in smaller formations the MC appears after puberty and is located superficially in the skin [14–16]. The development of a tumor within a blue nevus is characterized by a deeper location of the pathological process [17].
The prognosis for life in the case of the development of melanoma against the background of a melanocytic nevus, according to various sources, is considered more favorable or the same compared to primary tumors [5–7, 11, 18].
Discussion
In the literature one can find such a term as “melanoma-dangerous nevus”, implying the possibility of developing a malignant tumor against the background of a pre-existing benign pigmented formation [19, 20]. Researchers note that the main triggers for possible malignancy may be exposure to ultraviolet radiation, changes in hormonal levels during puberty or pregnancy, repeated household trauma, etc. Often, patients with identified MC indicate that a “regular mole” previously existed in the area of the tumor for a long time and for some reason she was "reborn". The established opinion about the degeneration of melanocytic nevi often leads to “preventive” removal of individual formations (in particular, dysplastic nevi) or elements located on the scalp and acral areas.
However, literature data indicate the absence of such a need. If constant mechanical action or ultraviolet radiation led to the “degeneration” of melanocytic nevi, then the predominant localization of the tumor process would change significantly. Thus, instead of the torso, MK against the background of a nevus would develop in areas of high pressure (soles) or in open areas exposed to prolonged exposure to ultraviolet radiation. Moreover, the term “melanoma-dangerous nevus” should be treated critically, given that early manifestations of MC lack the usual polymorphism of the clinical and dermoscopic picture, are difficult to diagnose and can imitate the manifestations of melanocytic nevi [2].
The clinical cases we have presented show that the formation of a malignant tumor against the background of a nevus is accompanied by noticeable changes and can be detected in a timely manner with proper professional training and/or the use of auxiliary means (for example, artificial intelligence). Considering the banal external manifestations of melanocytic nevi, against which MK developed, or the accidental detection of nevus cells during histological examination, the doctor cannot predict which particular “mole” of the patient may turn out to be a “time bomb”. There is also data on the extremely low probability of malignancy of a single melanocytic nevus - the annual risk does not exceed 0.0005% for people under 40 years of age and 0.003% for men over 60 years of age [21]. Thus, the process of removing melanocytic nevi in most cases should be considered either a diagnostic procedure, in which the doctor does not have enough clinical data to make a diagnosis, or an aesthetic one, in which the appearance of the formation does not suit the patient, but not a preventive measure!
On the other hand, cases of MK development against the background of melanocytic nevus cannot be called rare. The presented statistical data are generalized, but if we take a group of high-risk patients, the incidence of MC development against the background of melanocytic nevus can increase to 54.2% [10]. Moreover, the likelihood of detecting nevus cells during a morphological examination can be influenced by the process of preparing histological preparations at the stage of cutting material in the laboratory, the qualifications of the pathologist and the stage of the tumor process. Molecular genetic studies have shown that as tumor thickness increases, the likelihood of detecting preexisting melanocytic nevus cells with standard hematoxylin-eosin staining decreases [22]. One of the recent studies showed that in some nevus-associated tumors, nevus and melanoma melanocytes have an identical genetic profile [23]. These findings support the concept of "degeneration" and indicate the need for further study of the problem.
An urgent task is to determine the sequence of events that trigger carcinogenesis and contribute to its progression. Today, in the genetics of malignant melanoma, in addition to the congenital predisposition to tumor development, there is the possibility of the formation of local somatic mutations that trigger carcinogenesis [24]. The ideally simple theory of “degeneration” assumes a single path of evolution: the gradual transformation of a simple nevus into an atypical one (for example, dysplastic), and then into melanoma. But in reality, the theory of tumor progression proposed by WH Clark [25] is not limited only to dysplastic nevi as precursor formations. The proposed alternative theories of carcinogenesis [26] are also not compared with clinical data, since they do not take into account the likelihood of developing CM against the background of congenital nevi.
Conclusion
Thus, the process of formation of nevus-associated melanoma today is more correctly considered an accident, the likelihood of which the medical community cannot predict. In this regard, one of the most important areas for preventing late detection of skin melanoma can be the timely formation of high-risk groups and active dynamic monitoring of patients. The importance of identifying MK at an early stage and the presence of visible signs of the development of a malignant tumor dictate the need to use dermoscopic technology with the possibility of significant optical magnification and work with series of images. The complexity of analyzing series of images of dozens and sometimes hundreds of tumors in patients at risk at a medical appointment creates conditions for the development of artificial intelligence technologies and the introduction of automated digital image processing [27].
Differential diagnosis
To make an accurate diagnosis, a dermatologist must conduct a series of tests, since the symptoms of linear moles are similar to those of other skin diseases.
At issue are:
- warty neurodermatitis
- characterized by lycosis and itching; - lichen planus papillary
- characterized by itching and its occurrence at a later age, determined by the presence of typical lesions of lichen planus in other places and histological examination; - lichen striata - characterized by inflammatory papular rashes and spontaneous resolution within a few months.
WHAT NEVUS ARE DANGEROUS?
Nevi should be constantly examined for possible changes in size or shape, because this is one of the symptoms of melanoma. With an increase in the number of moles, there is a risk of cancer. There are many cases where a nevus has degenerated into a malignant neoplasm. You should see a doctor when:
- The nevus is subject to constant trauma;
- Nodules and other formations form in the area of the mole:
- The mole itches, tingles and itches;
- The nevus has changed in size, pigmentation or shape;
- A new nevus has formed and is bleeding.
These manifestations may indicate the degeneration of a mole into a malignant formation.
Treatment of epidermal moles
Epidermal moles persist throughout life, do not tend to disappear spontaneously and are primarily a cosmetic problem, especially on the skin of the face and neck. These are benign formations, although there are risks of developing cancer. A case of squamous cell carcinoma inside a nevus has been described in the literature. Treatment of epidermal moles is necessary for cosmetic reasons.
Treatment uses many different methods, varying in effectiveness and availability. When treating epidermal nevi, the following is used:
- surgical removal of the lesion;
- electrocoagulation;
- cryotherapy;
- dermabrasion;
- CO 2 laser;
- dye laser;
- tretinoin;
- 5-fluorouracil;
- acitretin;
- calcipotriol;
- dithranol;
- podophyllin;
- keratolytic drugs.
Conservative methods fail to achieve complete recovery, and scars remain after surgical removal of the lesion. The mechanism of action of individual methods is not always fully understood. For example, calcipotriol can affect the production and function of cytokines and normalize the differentiation of epidermal cells, 5-fluorouracil has an antiproliferative effect.
Some of the treatments that were used in the past are now only of historical significance.
According to many scientists, the most effective method of treating linear lesions in a small area is to remove the nevus by surgical excision; however, when completely removing large lesions, it is necessary to cover the defect with a free skin graft, which is often associated with the formation of an unaesthetic scar.
The effect of laser on moles
Treatment of papillomatous nevus
Due to the fact that the nevus is constantly exposed to external factors, it can become damaged and then inflammation will begin, which can be easily recognized by soreness and redness. If during the diagnostic process doctors managed to completely exclude melanoma, dermatologists recommend removing the nevus with mandatory further histological examination of the formation.
Removal of papillomatous nevus can be carried out using a laser, cryodestruction, radio wave, electrocoagulation or surgical excision. Typically, all of the above operations are performed under local anesthesia.
Laser removal of warts
The use of lasers gives promising results. Various types of lasers have been used to treat moles, including: CO 2 lasers, dye laser. Landthalter et al. Dermatologists have successfully used argon laser in patients with localized papillary epidermal nevus. Also, very good results are achieved using the argon laser in most patients with superficial nevus, while satisfactory results have not been obtained in patients with papillary nevus.
Another method of laser treatment of warts is the removal of epidermal nevus with a pulsed Er: YAG laser operating at a wavelength of 2940 nm and having the properties of high absorption of water contained in the tissue, as well as CO 2 laser removal.
The pulse energy is aimed at ablation, and the area of thermal damage is small, which minimizes the possibility of scarring and guarantees a relatively rapid healing process. This type of laser can remove superficial changes with very good cosmetic results.
In the case of large papillary moles of the epidermis, the best method is CO2 laser treatment.
Uch. Michel et al have used the CO 2 laser in the treatment of papillary epidermal moles with good cosmetic results when the appropriate specifications are met. The small lesions have completely disappeared, leaving only a discolored scar. Relapses were observed with too gentle procedures.
Based on these results, scientists claim that CO 2 laser treatment is more effective than other lasers, but at the same time has a higher risk of scarring. Laser treatment is a relatively new, but very promising method of treating papillary nevi of the epidermis.
Sources
- Du Vivier A.: Atlas of Clinical Dermatology, 2002.
- Gur E, Zucker R: Complex facial nevi: a surgical algorithm, 2000.
- Rosen T: Keratoacanthomas arising within a linear epidermal nevus. J. Dermatol. 1982.
- Mikhalovsky R.: Dermatological syndromatology, 1984.
- Goldberg HS: Basal cell epitheliomas developing in a localized epidermal nevus. 1980.
- Ichikawa T. et al.: Squamous cell carcinoma arising in a verrucous epidermal nevus, Dermatology, 1996.
- Molin L, Sarhammar G: Perivulvar inflammatory linear verrucous epidermal nevus treated with CO2 laser, 1999.
- Michel JL et al: CO 2 laser dermabrasion in the treatment of linear papillary epidermal nevi, Dermatologica, 2001.
- Pavlacik M. et al.: Epidermal nevus syndrome - a two-symptomatic form, 1996.
- Zvulunov A. et al.: Calcipotriol for topical use for the treatment of inflammatory linear verrucous epidermal nevi: 1997.
- Pearson IC, Parland CC: Treatment of epidermal nevi with pulsed erbium laser, 2005.
- Boyce S, Alster TS: CO 2 laser treatment of epidermal nevi long-term success. 2002.
Popular methods for removing nevi
Removal of nevi in Moscow involves the possibility of using a number of minimally invasive methods; the most popular are:
- cryodestruction, that is, exposure to very low temperatures (freezing), the conductor is liquid nitrogen, which allows you to remove nevi in the epidermis and dermis, but does not make it possible to control the depth of exposure; in addition, there is a certain risk of affecting nearby tissues, which can lead to burns and scars;
- laser, or gentle selective exposure to laser radiation exclusively on pathological tissues at different depths (can be set by settings); does not cause skin burns, does not leave scars;
- cauterization with current, or electrocoagulation, when pathological tissues are destroyed under the influence of high-frequency current, suitable only for superficial (epidermal) neoplasms;
- chemical cauterization, which is used less and less due to the high risk of damage to healthy skin.
When it comes to eliminating a malignant nevus, only surgical excision
. Any minimally invasive method can provoke rapid tumor development. If they are benign in nature, it is preferable to remove nevi with a laser. It is fast, safe, does not cause side effects or scars on the skin. At DECA, the procedure is carried out using high-tech Italian equipment.
Do you need a consultation with a dermato-oncologist? Do you want to get rid of nevi? Call!